About this course:
This course reviews relevant terminology and statistics related to concussions, including health disparities that increase the risk of concussion in certain groups. This course will also review the pathophysiology, clinical manifestations, diagnosis and evaluation, and concussion management strategies. Finally, this course will review prevention strategies that can reduce the incidence of concussions.
Course preview
This course reviews relevant terminology and statistics related to concussions, including health disparities that increase the risk of concussion in certain groups. This course will also review the pathophysiology, clinical manifestations, diagnosis and evaluation, and concussion management strategies. Finally, this course will review prevention strategies that can reduce the incidence of concussions.
After this activity, learners will be prepared to:
review relevant terminology and statistics for concussions, including sports-related concussions
identify health disparity factors that increase the risk of sustaining a concussion
describe the pathophysiology and clinical manifestations associated with concussions
describe the critical components of the diagnosis and evaluation of concussions
discuss various strategies for the management of concussions and prevention of complications
identify various prevention strategies to reduce the incidence of concussions
According to the Centers for Disease Control and Prevention (CDC, 2020), concussions have become a prominent public health issue in health care, contributing to significant morbidity, permanent disability, and mortality among adults and children. Heightened media coverage surrounding the long-term effects of sports-related head injuries experienced by professional athletes has sparked interest among healthcare providers (HCPs), coaches, parents, and athletes. While most patients will return to baseline and experience a full recovery following a concussion, some will endure persistent symptoms and effects. Individuals who sustain repetitive concussive injuries are at increased risk for experiencing prolonged impairments and deficits. Long-term neuropsychiatric testing on athletes who have sustained frequent concussions has demonstrated that multiple concussions over a lifetime can lead to irreversible cognitive impairment, and appropriate management is critical for improving long-term outcomes. HCPs play a critical role in preventing concussions and improving patient outcomes through timely recognition, diagnosis, management, treatment, and referral to appropriate services (i.e., neurology; CDC, 2020; Corrigan et al., 2019; Sarmiento et al., 2019).
Background
A concussion, otherwise known as a mild traumatic brain injury (mTBI), is a “disruption of brain function and/or structure due to the application of an external physical force that produces signs and symptoms of brain dysfunction in the acute injury period” (Corrigan et al., 2019, p 3). Essentially, a force outside the body shakes the head and harms the brain. The brain injury may arise directly from the forceful blunt or penetrating trauma to the head or from acceleration/deceleration forces, inducing clinical symptoms. The term concussion is not well-defined among medical communities and organizations, and descriptions are often inconsistent. These inconsistencies have led to confusion among patients, family members, and HCPs regarding the importance of the diagnosis. Controversy surrounds the term concussion, as many HCPs believe it unintentionally communicates that a brain injury did not occur, downplaying the potential severity of the injury and future sequelae. As a result, current guidelines recommend that HCPs use the terms mTBI or TBI instead of concussion, as it highlights the seriousness of the injury. For this educational module, the term concussion will be used interchangeably with mTBI. Not all bumps, blows, or forceful trauma to the head will result in an mTBI, and not all individuals who endure an mTBI will have associated cognitive and physical deficits. The impact of an mTBI on brain function can present uniquely, and damage can occur to varying degrees based on the extent of the injury, which is why it is critical to understand the mechanism of the injury and associated clinical manifestations. Every concussion has an identical disease trajectory or outcome. The location of the impact has no defined influence on prognosis or outcome, although trauma to the top of the head does carry an increased risk for loss of consciousness (Corrigan et al., 2019; Sarmiento et al., 2019; Sussman et al., 2018).
Incidence
The CDC (2021g) collects and reports TBI data to understand who is at risk, how many people are affected, the most common mechanisms for TBI, and whether prevention programs are helping. Approximately 2.5 million people in the US sustain a TBI each year, with 75% to 95% of these classified as an mTBI. In 2018, there were 223,050 TBI-related hospitalizations, and in 2019 there were 60,611 TBI-related deaths. To further quantify the magnitude of TBIs, these numbers represent approximately 610 TBI-related hospitalizations and 166 TBI-related deaths per day in the US. However, this number does not include individuals who sustain a TBI and do not seek care at a hospital, primary care office, or urgent care. In 2018, children (i.e., birth
...purchase below to continue the course
Sports-Related TBIs
Although sports-related TBIs make up a small percentage of all TBI-related injuries, significant research funding is allocated to identifying, evaluating, and treating these injuries. The CDC estimated that in 2019, approximately 15% of high-school students reported one or more sports-related TBIs in the previous year. Researchers estimate this percentage is likely higher because high-school athletes may conceal TBI symptoms, often due to fear of missing playing time or letting their team down. Sports-related TBIs can occur at all ages, but some groups are at higher risk for injury. Football accounts for the highest percentage of sports-related TBIs at the high-school and collegiate levels. Soccer has the highest rate of sports-related TBIs in female athletes, and female athletes are twice as likely to experience a TBI as males in the same sport. Other collision-related sports with increased rates of TBI include rugby, ice hockey, boxing, lacrosse, and field hockey. The prevention of sports-related TBIs is a public health priority since TBIs can impact a child’s health, thinking, and behavior, including learning and self-regulation (CDC, 2021a; Ferry & DeCastro, 2022; Meehan & O’Brien, 2020).
Health Disparities Related to TBIs
Although TBIs can affect people of all ages, some groups are at greater risk of sustaining or dying from a TBI or experiencing long-term health consequences from their injury. Health disparities related to TBIs have been found for various groups, including older adults, service members and veterans, people who experience homelessness or are in correctional facilities, survivors of intimate partner violence (IPV), racial and ethnic minorities, and people living in rural areas (CDC, 2021a). Specific examples of health disparities related to TBIs include the following (CDC, 2021a, 2021c, 2021g):
Older adults (i.e., over 75 years of age) account for approximately 32% of TBI-related hospitalizations and 28% of TBI-related deaths, the highest among all age groups. Accurate TBI diagnoses in this age group can be missed due to other medical conditions with overlapping symptoms (e.g., dementia).
Males are twice as likely to be hospitalized and three times more likely to die from a TBI than females.
American Indian/Alaska Native adults and children have higher TBI-related deaths and hospitalization rates than other racial or ethnic groups. Contributing factors to this disparity include limited access to health care and higher rates of motor vehicle accidents, suicide, and substance abuse. In addition, Hispanic and non-Hispanic Black individuals are less likely to receive rehabilitation and follow-up care and more likely to have poor psychosocial and functional outcomes post-TBI than non-Hispanic Whites.
Military service members and veterans who have sustained a TBI are more likely to have ongoing symptoms, difficulty accessing health care, recurring post-traumatic stress disorder (PTSD), depression, and suicidal thoughts. An estimated 400,000 US service members were diagnosed with a TBI between 2000 and 2019, with 20% occurring while on active duty.
Approximately 50% of people in correctional facilities have a history of a TBI. These individuals also have higher rates of mental health problems, including substance use disorders, suicidal thoughts, and difficulty controlling their anger.
People who experience homelessness are 2 to 4 times more likely to experience a TBI and 10 times more likely to sustain a moderate to severe TBI. Individuals with a history of TBI are more likely to have poor physical and mental health, substance abuse, and suicidal thoughts.
Survivors of IPV who sustain a TBI due to an assault are more likely to experience insomnia, depression, and PTSD and report poor overall health.
TBI survivors with low income and/or who are uninsured or underinsured face significantly more barriers to treatment than people with private insurance. These individuals are more likely to die in the hospital and are less likely to receive a TBI procedure (e.g., craniotomy, ventriculostomy, intracranial pressure monitor) or inpatient services (e.g., rehabilitation).
People living in rural areas are more likely to die from a TBI than people living in urban areas due to limited access to appropriate facilities for treatment (e.g., a Level I trauma center and specialty services).
Pathophysiology
A head injury encompasses any damage to the head due to trauma; however, a head injury does not mean that an injury to the brain occurred. A TBI or craniocerebral trauma occurs when external forces produce an injury that affects how the brain works. TBIs vary in severity from mild, transient symptoms to severe and debilitating symptoms that impact a person’s quality of daily life. A concussion or mTBI occurs when a mechanical force or trauma occurs to the head, neck, or body, resulting in the rotational acceleration of the brain within the skull. As a result, the brain moves rapidly back and forth inside the skull, leading to a cascade of events within the brain, such as chemical changes, neuronal depolarization, metabolic derangements at the cellular level, and decreased blood flow (see Figure 1). The stretching, damage, and/or death of brain cells associated with the injury subsequently provoke a clinical syndrome characterized by an immediate and/or transient alteration in brain function. The acute clinical symptoms are thought to be related to the disturbance of brain function rather than a structural injury (American Association of Neurological Surgeons [AANS], n.d.; Evans & Whitlow, 2022; Hinkle & Cheever, 2018).
Traumatic brain injuries take two forms: the primary event (primary brain injury) and the secondary event (secondary brain injury). The primary event refers to the damage resulting from the direct contact to the head or brain during the immediate injury, causing extracranial focal injuries (e.g., lacerations, contusions, external hematomas, and skull fractures) and focal injuries from the brain moving inside the skull (e.g., subdural hematomas [SDH], concussion, and diffuse axonal injury [DAI]). The secondary event encompasses the damage that evolves hours to days after the initial injury due to inadequate delivery of nutrients and oxygen to the cells. In addition, intracranial pathologic processes—including cerebral edema, intracranial hypertension, intracranial hemorrhage, seizures, hyperemia (excess blood in the vessels supplying the brain), and vasospasm—contribute to secondary events. Other systemic effects such as hypotension, hypoxia, hypercarbia, hyperthermia, infection, electrolyte imbalances, and anemia can add to the complexity of the biochemical, metabolic, and inflammatory changes, further injuring the brain. Morbidity from a secondary event can be more severe than damage from the primary event (Romeu-Mejia et al., 2019; Shimoda et al., 2019).
The Monro-Kellie doctrine (hypothesis) helps explain the dynamic equilibrium of the cranial contents. The cranial vault contains the brain, blood, and cerebrospinal fluid. According to the Monro Kellie hypothesis, the cranial vault is a closed system; therefore, if any component increases in volume, another component must decrease in volume to maintain equilibrium. However, if that decrease in volume does not occur, then the pressure in the cranial vault will increase. Therefore, when a TBI occurs, swelling or bleeding within the skull will increase the volume of contents in the cranial vault, increasing intracranial pressure (ICP). When ICP rises too much, there is a displacement of the brain through or against the structures of the skull, resulting in a restriction of blood flow to the brain. Without adequate oxygen delivery and waste removal, cellular hypoxia can occur, resulting in ischemia and irreversible brain damage (Hinkle & Cheever, 2018).
Primary Events: The Initial Trauma
Tearing of brain cells (axonal shearing)—When an outside force strikes the head, the brain can bang back and forth inside the inflexible skull. Since the brain is soft and pliable and brain cells are fragile, the cells can be stretched to tearing (i.e., axonal shearing) in the cerebral hemispheres, corpus callosum, and brainstem. The damaged brain cells die when this occurs, resulting in a prolonged traumatic coma (Hinkle & Cheever, 2018; Shimoda et al., 2019).
Contusion—When the brain crashes against the inside of the hard skull, small blood vessels can be torn, resulting in one or more contusions (bruising and bleeding). These contusions can cause disability and death of brain cells. Although contusions can happen anywhere in the brain, they are more likely to occur in the anterior portions (i.e., frontal and temporal lobes) and the orbital areas (Hinkle & Cheever, 2018; Romeu-Mejia et al., 2019; Shimoda et al., 2019).
Skull fracture—When skull bones are cracked or broken, they may press on the brain and/or penetrate the brain with shards of broken bone. With an open skull fracture, in which the outside environment comes in contact with the cranial cavity, there is an associated risk of hemorrhage and infection (Corrigan et al., 2019).
Coup-contrecoup Injury—Brain damage can occur at the point of impact (coup) as well as on the opposite side (contrecoup; Shimoda et al., 2019). This type of injury results from the brain's forward and backward motion (acceleration/deceleration) inside the skull upon forceful impact (Hinkle & Cheever, 2018).
Secondary Events: The Body’s & Brain’s Responses to the Trauma
Brain swelling (edema)—The brain swells like any other body part following a traumatic injury. However, the brain is inside a rigid shell (the skull), which cannot expand and accommodate the increased tissue volume resulting from the swollen brain cells. Due to the rigid nature of the skill, swelling of the brain is dangerous and can cause damage by interrupting blood and oxygen flow to brain tissue, resulting in cellular death (Hinkle & Cheever, 2018).
Hematoma—If damaged blood vessels are large, they can develop into a hematoma (a collection of blood outside of blood vessels) inside the skull. A hematoma can increase pressure on the brain, and surgery may be required to drain the blood from the skull (Hinkle & Cheever, 2018).
Shock—With more severe brain injuries, there may be associated blood loss to the brain caused by the injured cells and tissue. Shock is the body’s response to a sudden and life-threatening drop in blood pressure, in which the body reacts by inducing vasoconstriction. Vasoconstriction is a narrowing of blood vessels in the extremities to conserve blood flow to the vital organs, such as the heart and brain (Romeu-Mejia et al., 2019; Shimoda et al., 2019).

Clinical Manifestations
The signs and symptoms of mTBI may appear immediately after the injury with a rapid onset of temporary impairment of neurological function that resolves spontaneously, or symptoms may evolve after several minutes or hours following the trauma. In some cases, symptoms last for days, weeks, or months. In rare cases, symptoms may persist for years. Confusion is the hallmark symptom with three principal features: (a) inability to maintain a coherent stream of thought, (b) disturbance of awareness with heightened distractibility, and (c) inability to carry out a sequence of goal-directed movements. When individuals experience amnesia after a head injury, it usually involves a loss of memory of the traumatic event, retrograde amnesia (loss of recall of events immediately before the injury), and anterograde amnesia (loss of recollection of events immediately after the injury; AANS, n.d.; Shimoda et al., 2019).
An mTBI may or may not involve loss of consciousness (LOC), but 90% of cases have no LOC. In general, symptoms of mTBI fall into four distinct categories: physical (somatic), sleep, cognitive, and emotional. Symptoms within these categories may change throughout the recovery period. For example, an individual may have a headache and nausea in the first few days following the mTBI, and they may experience mood disruption or trouble sleeping a week or two later. Symptoms of an mTBI may be challenging to determine due to other health problems. In addition, individuals may not recognize their symptoms or will minimize the impact of the symptoms on their daily life. Therefore, a validated concussive scale should be used to assess symptoms (e.g., Sideline Concussion Assessment Tool 5 [SCAT5]; CDC, 2021f; Ferry & DeCastro, 2022; Shimoda et al., 2019). See Table 1 for a list of the most common symptoms of mTBI organized by category.

Young children can experience head trauma, especially from falls, as they learn to walk and improve their strength and coordination. Other head trauma causes in this population include child maltreatment or pediatric abusive head trauma (AHT). Concussion or mTBI symptoms in this population can be difficult to diagnose because infants and toddlers cannot verbally explain how they feel. HCPs should monitor for listlessness or fatigue, irritability, excessive crying, a loss of balance or unsteady gait, a dazed appearance, a change in eating or sleeping patterns, vomiting, and/or seizures (Mayo Clinic, 2022). See the Nursing CE course Pediatric Abusive Head Trauma for more information.
Diagnosis and Evaluation
mTBI is a clinical diagnosis based on patient history and physical examination findings. However, making a diagnosis can be challenging since no finding or a minimum number of symptoms is required for an mTBI. Several standardized concussion scales can be used in a pre-hospital setting to assist in determining the presence of an mTBI, such as the SCAT5 (often used by athletic trainers) and the Child SCAT5 (for children between 5 and 12 years of age). These tools should be administered in a quiet environment with minimal distractions. However, these tools are only validated when a preinjury baseline score is available for comparison. HCPs, parents, coaches, and athletic trainers should also monitor for signs and symptoms of neurological deterioration because delayed symptom onset can occur. Neurological deterioration signs or symptoms should prompt an immediate referral to an emergency department for further evaluation (Ferry & DeCastro, 2022). The following warning signs require urgent and immediate assessment:
- worsening headache
- seizures
- repeated vomiting
- slurred speech
- weakness in the arms or legs
- persistent confusion
- worsening drowsiness
- LOC or somnolence (Corrigan et al., 2019; Stein et al., 2017).
Physical Examination
HCPs should conduct a physical examination to assess for signs of an mTBI. The physical examination for patients with a suspected mTBI is critical since a diagnosis is primarily based on clinical findings. Therefore, a trained, licensed HCP (e.g., primary care provider, emergency department or urgent care provider, or athletic trainer) should complete the physical assessment. An estimated 80% of individuals with a past mTBI experienced a missed diagnosis when a nonmedically trained observer completed the evaluation. The acute physical examination will include a neurologic assessment and mental status testing. In some cases, a formal neuropsychological evaluation by a trained neuropsychologist can further supplement the HCP’s assessment of the various domains impacted by an mTBI (Evans & Whitlow, 2022; Ferry & DeCastro, 2022).
Thorough history-taking for patients who present with suspected trauma to the head is essential. A patient's ability to answer these questions can also assess the degree of amnesia (Corrigan et al., 2019). Key information to obtain includes the following:
- the nature of the head trauma
- history of prior head trauma
- prior or current military duties and trauma
- current medications
- alcohol and drug use patterns
- past medical history, including any comorbid conditions (AANS, n.d.)
While trauma to the head, neck, or body is a primary characteristic of mTBI, several common features are used clinically to define a head injury. The conclusive definition of concussion versus mTBI remains variable throughout the literature. However, the leading organizations emphasize four primary diagnostic criteria: level of consciousness, post-traumatic amnesia, mental status, and neurological signs (Corrigan et al., 2019). In addition, it is critical to evaluate all head trauma patients initially for cervical spine damage and scalp/skull fracture. An examination of the head and neck should be completed, looking for signs of basal skull fracture. These signs on a physical exam can indicate more severe intracranial injuries and may warrant further diagnostic imaging (e.g., CT scan or MRI scan of the brain):
- cerebral spinal fluid leakage (clear fluid) from the nose or ears (positive pledget test)
- blood behind eardrum
- bruising around the eyes or behind the ears
- weakness of the facial muscles
- loss of hearing or smell
- loss of vision or double vision (Martin, 2017)
A comprehensive neurological exam should be completed, including:
- cranial nerves (at least cranial nerves III through VII)
- reflexes
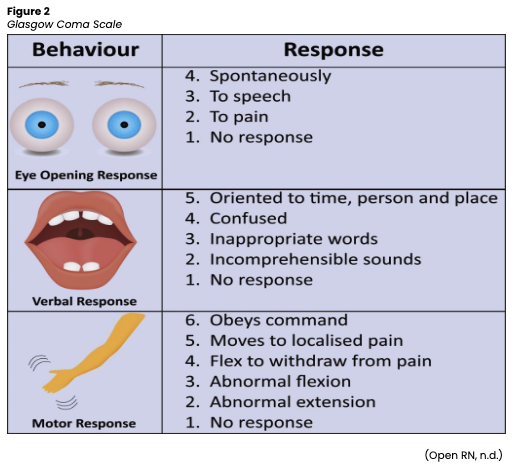
- Glasgow coma scale (GCS; see Figure 2)
- coordination, gait, balance
- sensory exam
- motor exam
- visual field testing (Martin, 2017)
A mental status examination should be completed. Questions focused specifically on orientation (e.g., name, date) are inadequate to detect an mTBI. A mental status assessment should include:
- memory loss (short-term and long-term)
- ability to concentrate
- ability to recall information (Mayo Clinic, 2022)
If the neurological examination raises a concern, an eye exam should be performed by an optometrist or ophthalmologist to detect dysfunction in central and peripheral vision caused by medical conditions and other neurologic deficits. Visual field problems can result from injury to the visual pathways, including retinal damage, optic neuropathy, and structural brain injury or pathologies. An electroencephalogram (EEG) is an electrophysiological monitoring test used to identify any problems related to the brain's electrical activity. An EEG should be performed if seizures are witnessed or suspected (Martin, 2017).
A diagnosis predominantly relies on the nature of the incident, the presence of specific symptoms, and the clinician's skill in evaluating the patient. A diagnosis of mTBI should be considered when one or more abnormalities of brain function are noted after an identified traumatic head injury. Since an mTBI primarily reflects a transient disturbance in brain functioning, it is not typically associated with structural injuries detected on routine neuroimaging studies. Therefore, diagnostic tests usually will not show any changes, and HCPs are advised not to perform routine computed tomography (CT) imaging, magnetic resonance (MRI) imaging, or skull X-rays when screening for or diagnosing an mTBI due to unnecessary radiation exposure. However, it is critical to identify and rule out patients at risk for intracranial injury (ICI) who may need head imaging. Symptoms such as severe headaches, vomiting, and seizures warrant brain imaging. A CT scan uses a series of X-rays to obtain cross-sectional images of the skull and brain, making it ideal for evaluating the brain right after an injury. An MRI uses powerful magnetic waves to produce a detailed image of the brain to identify changes or complications after a concussion. There is evidence that patients with an mTBI can be selected for CT imaging based on validated clinical criteria (e.g., Canadian CT head rule [CCHR], New Orleans criteria [NOC], and National Emergency X-Radiology Utilization Study II [NEXUS II] criteria). These criteria offer high sensitivity for identifying patients with clinically significant CT findings over reducing the number of CT examinations performed (AANS, n.d.; Evans & Whitlow, 2022; Martin, 2017; Mayo Clinic, 2022; Stein et al., 2017).
The CCHR criteria suggest a head CT for any patient with an mTBI and any of the following criteria:
suspected open or depressed skull fracture
GCS below 15 by 2 hours after the injury
any signs of a basilar skull fracture (i.e., intraorbital bruising [raccoon eyes], retroauricular bruising [battle sign], hemotypanum, or cerebrospinal fluid leak)
age 65 years or older
two or more episodes of vomiting
amnesia for events more than 30 minutes before impact
dangerous mechanism (i.e., ejection from a motor vehicle, pedestrian struck, fall from greater than 3 feet or 5 stairs)
neurologic deficit
seizure
presence of bleeding diathesis or oral anticoagulant use
return visit for a reassessment of a head injury (Evans & Whitlow, 2022)
The NOC criteria suggest a head CT for patients with a GCS of 15 in the following circumstances: headache, vomiting, drug or alcohol intoxication, persistent anterograde amnesia, age 65 years or older, seizure, or visible trauma above the clavicle. The NEXUS II criteria suggest a CT scan for a significant skull fracture, neurologic deficit, GCS under 14, abnormal behavior, scalp hematoma, coagulopathy, or persistent vomiting. Many healthcare organizations will develop a clinical pathway for evaluating an mTBI using a combination of these criteria. In addition to these options, the American College of Emergency Physicians (ACEP) has criteria similar to the NOC, and the National Institute of Health (NIH) has criteria similar to the CCHR (Evans and Whitlow, 2022). The ACEP and the CDC set guidelines for mTBIs in adults in 2002 as part of the HEADS UP Program. These guidelines were most recently updated in 2008, and key recommendations are as follows:
Evidence supports the use of CT over MRI in acute evaluations.
A non-contrast CT is warranted for patients with or without LOC or post-traumatic amnesia after a head injury with specific symptoms.
An intracranial injury can occur even without LOC. Therefore, imaging should be done if an intracranial injury is suspected.
There is minimal risk of developing an intracranial lesion for patients with a negative CT, and they can be discharged safely home (CDC, 2021h).
A CT scan should only be used for children if specific criteria are met, such as the type of head injury or signs of a skull fracture. The following list outlines warning signs in children that require immediate and urgent evaluation, including imaging with a CT scan:
worsening headache
seizures
repeated vomiting
slurred speech
weakness in the arms or legs
persistent confusion
worsening drowsiness
somnolence (Corrigan et al., 2019; Stein et al., 2017)
Classification of Traumatic Brain Injury
The severity of an mTBI is classified along a clinical and pathological continuum ranging from mild to severe, with symptoms varying from a headache or brief change in mental status to extended periods of unconsciousness, coma, or death. The severity of symptoms when the injury first occurs does not necessarily predict the extent of future symptoms. It is impossible to predict at the time of the injury which patients will recover rapidly and which will have persistent symptoms and deficits. As a result, guidelines and scales have been developed to grade TBI severity, and HCPs are trained to use validated symptom scales to determine the severity of an injury. These scales are essential tools that help guide medical decision-making, track changes following treatment, and improve patient outcomes (Martin, 2017; Stein et al., 2017).
The CDC (2021e) offers a list of age-appropriate validated neuropsychological tools to assess the severity of symptoms. The GCS is among the most widely utilized measures to determine the severity of an injury. Some other commonly used and validated tools include:
Post-Concussion Symptom Scale
Health and Behavior Inventory
Post-Concussion Symptom Inventory
Acute Concussion Evaluation (CDC, 2021e)
The US Department of Veterans Affairs (VA) and the Department of Defense (DoD; 2021) devised an evidence-based clinical practice guideline to classify and manage concussions and mild traumatic brain injuries. The guideline is grounded in extensive research and updated every 2 years to ensure accuracy; it lists symptom criteria used to grade concussion severity, as outlined below.
Mild TBI (Grade 1) is defined as either no loss of consciousness or a loss of consciousness lasting under 30 minutes. Post-traumatic amnesia (PTA), a loss of memory following the trauma, may last up to 1 day (24 hours). In addition, an altered mental state such as feeling dazed, disoriented, or transiently confused may last up to 24 hours. About 75% of TBIs are initially rated as mild with a GCS of 13-15.
Moderate TBI (Grade 2) is defined as a loss of consciousness lasting between 30 minutes and a few hours, up to 24 hours, followed by a few days or weeks of mental confusion. About 10%-25% of TBIs are rated moderate. PTA can be apparent between 1 and 7 days, with a GCS score of 9 to 12.
Severe TBI (Grade 3) is defined as a loss of consciousness for over 24 hours, either immediately after the injury or following a period of initial clarity. Fewer than 10% of all TBIs are rated severe. People who remain unconscious for a prolonged time may be described as being in a coma or permanent vegetative state with a GCS below 9 (US Department of VA and DoD, 2021).
Concussion Management
Ultimately, mTBI management focuses on preventing secondary events (i.e., secondary prevention). Therefore, education should be the central component of all concussion interventions. Outpatient observation by a responsible individual educated on warning signs requiring further evaluation is generally appropriate. Continued hospital observation is appropriate for patients with more concerning signs or symptoms. No pharmacologic interventions will speed the recovery process; therefore, concussion management is largely supportive. The mainstay treatment for the initial management of the acute symptoms resulting from an mTBI is cognitive and physical rest. Symptoms generally worsen when the metabolic trauma to the brain at the cellular level is challenged by stressful activity. Therefore, patients should be advised to rest for the first few days following an injury and limit physical and cognitive activities to avoid worsening symptoms. Due to the high variability in initial and future symptoms, there is no definitive and quantifiable timeline for physical and cognitive rest following an mTBI. While a rest period should be managed based on the individual patient, and a consensus has not yet been achieved, the patient should have at least a 24- to 48-hour initial rest period. Resting the brain includes avoiding sports and reducing visual stimulation by avoiding electronics, computers, video games, and bright screens. In addition, patients should be counseled to avoid activities that place them at risk for another injury to the head and brain (AANS, n.d.; Ferry & DeCastro, 2022; Martin, 2017).
For headaches and other somatic symptoms, medications such as acetaminophen (Tylenol), nonsteroidal anti-inflammatory drugs (Ibuprofen), amitriptyline (Elavil), or gabapentin (Neurontin) may be used. However, limited evidence demonstrates their efficacy in treating concussion-related headaches and other symptoms. Patients should be strongly advised to avoid medications that lower their seizure threshold (i.e., bupropion (Wellbutrin), traditional antipsychotic medications) or those that can cause confusion (i.e., lithium (Lithobid), benzodiazepines). Patients with a history of TBI can be more sensitive to side effects from medications, so they must be monitored closely for toxicity and drug-drug interactions. Furthermore, patients should be advised to limit quantities of medications with a high risk for suicide, as patients with a history of TBI have a higher suicide rate (Corrigan et al., 2019; Ferry & DeCastro, 2022; Martin, 2017; Stein et al., 2017).
Sleep is essential for people with concussions as it allows the brain to heal. Sleep hygiene counseling and screening for anxiety, depression, or PTSD should be considered for sleep dysregulation symptoms. Medications such as melatonin (Circadin) and trazodone (Desyrel) may be beneficial for regulating sleep. Cognitive disruptions and impairments must be monitored cautiously, and school and/or work accommodations are often necessary due to cognitive fatigue and concentration deficits. Emotional symptoms should be observed with extreme caution, and patients should be screened for risk of self-harm. Anti-anxiety and antidepressant medications may be used to alleviate some of these emotional symptoms (AANS, n.d.; Martin, 2017; Stein et al., 2017; Tjong et al., 2017).
Prognosis and Recovery
According to epidemiological data on the prognosis and recovery of individuals after mTBI, most will experience a full recovery within 3 weeks of injury. However, some individuals endure persistent symptoms (CDC, 2021e).
Approximately 30% of patients experience symptoms at 1-month post-injury.
Approximately 10% of patients experience symptoms at 3-months post-injury.
Approximately 5% of patients experience symptoms at 1-year post-injury.
Once symptoms have resolved, patients should be reintroduced to daily activities. Returning to work (or school) is generally advised as a symptom-guided and graded process that is unique to the individual patient, the extent of deficits, prior concussions, and recovery of symptoms. It is crucial to avoid over-exertion and re-injury during the recovery period, so patients should be counseled on resuming their full daily activities as a gradual transition to preserve function and avoid overstimulation. Abrupt re-entry to normal activities (e.g., work, school, or sports) may induce cognitive fatigue, overwhelm the brain, and lead to a setback in healing with a recurrence of symptoms. The recovery process may be slower for older adults, young children, teens, and individuals with a history of previous TBI. If symptoms return or worsen with activity, the activity should be stopped. Before engaging in sports, athletes recovering from concussions must be symptom-free at rest and after physical and mental exertion (AANS, n.d.; CDC, 2021b; Stein et al., 2017; Tjong et al., 2017).
The length of time the patient should refrain from strenuous activity is based on the grade of the mTBI, history of prior mTBIs, and severity of symptoms. Patients with a history of prior mTBIs have longer restrictions than those without this history. Those who have had a TBI in the past are at higher risk for impaired recovery, post-concussion syndrome, and long-term deficits. Additional factors that potentially delay recovery time include preexisting neurological or psychiatric health conditions; learning disabilities or difficulties; family, social, or psychosocial stressors; and the use of alcohol or other CNS-depressant drugs, which can slow recovery and put patients at risk of further injury (CDC, 2021b; Kapadia et al., 2019; Stein et al., 2017).
Post-Concussion Syndrome (PCS)
PCS refers to a collection of symptoms following an mTBI that persists for a prolonged period (i.e., weeks to months) despite an adequate rest interval. These symptoms are similar to those of an mTBI, but instead of improving with time and rest, they persist or worsen and are refractory to interventions. Approximately 15% to 20% of patients with an mTBI will experience some symptoms of PCS. The transition from mTBI to PCS is not well defined and poorly understood. PCS is a complex pathophysiologic process, and there is no current consensus on the duration of symptoms needed to make the diagnosis. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines the condition as concussive symptoms for more than 3 months. Although any mTBI symptoms can be present, PCS often comprises multiple somatic, emotional, and cognitive symptoms. PCS occurs most commonly in patients with a history of multiple mTBIs and does not appear to be associated with the severity of the initial injury. Treatment generally consists of resting and allowing the brain’s natural recovery process to heal the damage caused by an mTBI. However, given the complexity of the diagnosis, those with suspected PCS should be referred to a specialist in mTBIs. No single treatment is effective in all cases, but clinicians may prescribe pharmacologic or other active therapies to help alleviate specific symptoms. In addition, cognitive and physical rest and the management of sleep-wake disorders can be helpful (AANS, n.d.; Evan & Whitlow, 2022; Kapadia et al., 2019; Tjong et al., 2017).
Second Impact Syndrome (SIS)
SIS occurs when a person develops LOC or altered mental status within seconds to minutes after a second mTBI while still symptomatic from a previous mTBI. Although this is rare, it can be a potentially fatal complication. Researchers propose that the second mTBI causes profound changes in the still-recovering brain, as impaired cerebral autoregulation leads to cerebrovascular congestion and malignant cerebral edema with increased ICP. Unfortunately, there is no specific treatment for SIS, and management focuses on mitigating ICP. A 2021 literature review looked at 45 cases of SIS in males between 10 and 29 years of age. The timing of the second mTBI occurred anywhere from 1 hour to 5 weeks after the initial mTBI. Of the 45 cases, there were 19 fatalities attributed to SIS. Therefore, the prevention of SIS is a primary factor in return-to-play protocols for sports-related mTBIs (Evans & Furman, 2021).
Chronic Traumatic Encephalopathy
Chronic traumatic encephalopathy (CTE) is a progressive degenerative brain disease associated with repetitive head trauma that most commonly affects military veterans or professional athletes. In CTE, a protein called Tau forms clumps that slowly spread throughout the brain, killing brain cells and causing brain function to deteriorate gradually over time. CTE can only be confirmed post-mortem but has become a topic of interest based on media coverage surrounding professional athletes, mental health, and suicide. Early symptoms may only affect a patient's mood and behavior, but the symptoms worsen over time. Some common changes seen include impulse control problems, aggression, depression, and paranoia. As the disease progresses, some patients may experience issues with thinking and memory, including memory loss, confusion, impaired judgment, and eventually progressive dementia (Evans & Furman, 2021; Ferry & DeCastro, 2022).
Prevention
The acute and chronic morbidity associated with an mTBI has driven various public health initiatives to reduce the incidence of mTBIs. Older adults and individuals participating in contact sports are at increased risk for recurrent head injuries. While there is no one-size-fits-all solution to mTBI prevention, various organizations such as the CDC have focused on preventing TBIs and reducing the chance of disability following a TBI event. The CDC conducts surveillance and research to support data-driven solutions to prevent head injuries, including efforts to prevent falls among older adults, suicide prevention, firearm-related injuries, motor vehicle safety, and assault or other violence (CDC, 2016).
Various prevention strategies can help reduce the incidence of mTBIs across all age groups. HCPs play a critical role in delivering education about preventing head injuries (CDC, 2021d). Key prevention strategies are as follows (AANS, n.d.; CDC, 2021d):
Car and booster seats should be age- and size-appropriate and correctly installed in the vehicle. Infants and toddlers from birth until ages 2 to 4 should be secured in a rear-facing car seat. Toddlers should remain rear-facing for as long as possible until they reach the maximum weight or height limit.
Wear a seatbelt whenever riding in a motor vehicle.
Never drive or operate a vehicle under the influence of drugs or alcohol.
Wear a helmet or headgear whenever riding a bike, motorcycle, snowmobile, scooter, or all-terrain vehicle. In addition, a helmet or headgear should be used when playing contact sports such as football, ice hockey, boxing, skateboarding, riding a horse, and skiing or snowboarding.
Fall prevention for older adults should include reviewing medications with an HCP to see if any increase the risk of dizziness or drowsiness. In addition, undergo a yearly eye exam and make sure eyeglass prescriptions are current. Mobility and strength exercises can help improve balance. Finally, complete a home safety check to look for and remove tripping hazards such as area rugs and electrical cords.
Childproofing homes can prevent falls and other injuries. For example, install window guards and use safety gates for the top and bottom of the stairs.
Keep firearms unloaded and locked in a cabinet or safe, and store ammunition in a separate, secure location.
Sports-related safety tips apply to individuals of all ages. Some specific educational tips can include:
- supervise children at all times
- do not dive into water under 9 feet deep or in above-ground pools
- follow the posted rules at waterparks and pools
- do not wear clothing that can interfere with vision
- do not participate in sports when tired or sick
- obey all traffic signals when road cycling or skateboarding
- discard equipment that is broken
Schools and organizations should have concussion or mTBI policies and protocols for all sports. These protocols should contain educational material for students, parents, coaches, athletic trainers, and anyone involved with sports-related activities. These individuals should be educated on the importance of concussion or mTBI prevention, warning signs of an mTBI, and the importance of disclosure. Tremendous pressure can be placed on athletes and coaches to win at all costs, including ignoring when an athlete has signs or symptoms of a concussion. Research has shown that athletes often attempt to conceal a head injury for fear of being perceived as weak, losing playing time, or letting down their coach, teammates, and parents. However, ignoring signs and symptoms of an mTBI can result in a second head injury and increase the risk of long-term consequences, including death. Return-to-play protocols should be followed to prevent further harm to athletes. The CDC’s HEADS UP program includes educational training and materials for HCPs, coaches, and athletic trainers to raise awareness and inform action to improve prevention, recognition, and responses to mTBIs or other head injuries. The HEADS UP program was designed with the common goal of protecting kids and teens from sustaining severe head injuries. The HEADS UP materials were initially intended for HCPs, but recent initiatives have focused on educating parents, coaches, and school professionals. The HEADS UP materials are available for public use, and distribution is free (CDC, 2016, 2020).
References
American Association of Neurological Surgeons. (n.d.). Concussion. Retrieved February 25, 2022, from https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Concussion
Andrews, M. (2012). Concussion anatomy [Image]. https://commons.wikimedia.org/wiki/File:Concussion_Anatomy.png
Centers for Disease Control and Prevention. (2016). About HEADS UP. https://www.cdc.gov/headsup/about/index.html
Centers for Disease Control and Prevention. (2020). HEADS UP to health care providers. https://www.cdc.gov/headsup/providers/index.html
Centers for Disease Control and Prevention. (2021a). Get the facts about TBI. https://www.cdc.gov/traumaticbraininjury/get_the_facts.html
Centers for Disease Control and Prevention. (2021b). Getting better after a mild TBI or concussion. https://www.cdc.gov/traumaticbraininjury/concussion/getting-better.html
Centers for Disease Control and Prevention. (2021c). Health disparities and TBI. https://www.cdc.gov/traumaticbraininjury/health-disparities-tbi.html
Centers for Disease Control and Prevention. (2021d). Prevention. https://www.cdc.gov/traumaticbraininjury/prevention/index.html
Centers for Disease Control and Prevention. (2021e). Resources for health care providers. https://www.cdc.gov/traumaticbraininjury/providers/index.html
Centers for Disease Control and Prevention. (2021f). Symptoms of mild TBI and concussion. https://www.cdc.gov/traumaticbraininjury/concussion/symptoms.html
Centers for Disease Control and Prevention. (2021g). TBI Data. https://www.cdc.gov/traumaticbraininjury/data/index.html
Centers for Disease Control and Prevention. (2021h). Updated mild traumatic brain injury guideline for adults. https://www.cdc.gov/traumaticbraininjury/mtbi_guideline.html
Corrigan, J. D., Harrison-Felix, C., & Haarbauer-Krupa, J. (2019). Epidemiology of traumatic brain injury. In J. M. Silver, T. W. McAllister, & D. B. Arciniegas (Eds.), Textbook of traumatic brain injury (3rd ed., pp. 3-24). American Psychiatric Association Publishing.
Evans, R. W., & Furman, J. M. (2021). Sequelae of mild traumatic brain injury. UpToDate. Retrieved February 25, 2022, from https://www.uptodate.com/contents/sequelae-of-mild-traumatic-brain-injury
Evans, R. W., & Whitlow, C. T. (2022). Acute mild traumatic brain injury (concussion) in adults. UpToDate. Retrieved February 25, 2022, from https://www.uptodate.com/contents/acute-mild-traumatic-brain-injury-concussion-in-adults?
Ferry, B., & DeCastro, A. (2022). Concussion. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537017/
Hinkle, J. L., & Cheever, K. H. (2018). Textbook of medical-surgical nursing (14th ed.). Wolters Kluwer.
Kapadia, M., Scheid, A., Fine, E., & Zoffness, R. (2019). Review of the management of pediatric post-concussion syndrome: A multidisciplinary, individualized approach. Current Reviews in Musculoskeletal Medicine, 12(1), 57-66. https://doi.org/10.1007/s12178-019-09533-x
Mayo Clinic. (2022). Concussion. https://www.mayoclinic.org/diseases-conditions/concussion/symptoms-causes/syc-20355594
Meehan, W. P., III., & O’Brien, M. J. (2020). Concussion in children and adolescents: Clinical manifestations and diagnosis. UpToDate. Retrieved February 25, 2022, from https://www.uptodate.com/contents/concussion-in-children-and-adolescents-clinical-manifestations-and-diagnosis
Open RN. (n.d.). Glasgow coma scale [Image]. Retrieved February 25, 2022, from https://wtcs.pressbooks.pub/nursingskills/chapter/6-4-assessing-mental-status/
Romeu-Mejia, R., Giza, C. C., & Goldman, J. T. (2019). Concussion pathophysiology and injury biomechanics. Current Reviews in Musculoskeletal Medicine, 12(2), 105-116. https://doi.org/10.1007/s12178-019-09536-8
Sarmiento, K., Thomas, K. E., Daugherty, J., Waltzman, D., Haarbauer-Krupa, J. K., Peterson, A. B., Haileyesus, T., & Breiding, M. J. (2019). Emergency department visits for sports- and recreation-related traumatic brain injuries among children – United States, 2010-2016. Morbidity and Mortality Week Report (MMWR), 68(10), 237-242. https://doi.org/10.15585/mmwr.mm6810a2
Shimoda, K., Yokobori, S., & Bullock, R. (2019). History, overview, and human anatomical
pathology of traumatic brain injury. In K. Wang (Ed.). Neurotrauma, a comprehensive textbook on traumatic brain injury and spinal cord injury (pp. 3-11). Oxford University Press.
Stein, D. M., Feather, C. B., & Napolitano, L. M. (2017). Traumatic brain injury advances. Critical Care Clinics, 33(1), 1-13. https://doi.org/10.1016/j.ccc.2016.08.008.
Sussman, E. S., Penharkar, A. V., Ho, A. L., & Ghajar, J. (2018). Mild traumatic brain injury and concussion: terminology and classification. Handbook of Clinical Neurology, 158, 21-24. https://doi.org/10.1016/B978-0-444-63954-7.00003-3.
Tjong, V. K., Baker, H. P., Cogan, C. J., Montoya, M., Lindley, T. R., & Terry, M. A. (2017). Concussion in NCAA varsity football athletes: A qualitative investigation of player perception and return to sport. Journal of the American Academy of Orthopaedic Surgeons Global Research & Reviews, 1(8), e070. https://doi.org/10.5435/JAAOSGlobal-D-17-00070
US Department of Veterans Affairs and Department of Defense. (2021). Management and rehabilitation of post-acute mild traumatic brain injury. https://www.healthquality.va.gov/guidelines/Rehab/mtbi/