The purpose of this module is to provide the user with an overview of the anatomy and physiology of the endocrine system and all of its hormones.
Course preview
Disclosure Form
Objectives: Upon completion of this CE activity, the learner will be able to do the following
- review the anatomical features of the endocrine system
- elucidate the various hormones produced and regulated by the endocrine system
- discuss the normal physiology of the endocrine system
The Endocrine System
The endocrine system is a complex system that works in tandem with the nervous system to maintain the delicate balance of homeostasis. Nurses need to understand both the function of the endocrine system and alterations in function that can lead to the several pathologies discussed within this module. Disorders of the endocrine system contribute significantly to health care expenses each year. Dieleman and colleagues (2016) identified that more than 224.5 billion US dollars were spent in 2013 on endocrine disorders. Aside from the monetary costs, the loss of work, impaired quality of life, and ongoing personal disparities caused by endocrine disorders pose a significant burden to patients and their families. It is estimated that the prevalence of endocrine disorders is over 5% of the adult population in the US for each of the major diseases, including diabetes mellitus (DM), obesity, metabolic syndrome, osteoporosis, erectile dysfunction, dyslipidemia, and thyroiditis. Thyroid disorders and osteoporosis are the most common endocrine disorders in females, while erectile dysfunction and osteopenia are the most common disorders in males. DM occurs most often among patients who identify as an ethnic minority (Lonnemann, n.d.).
The complex and interconnected nature of the endocrine system can result in a variety of conditions, including but not limited to:
- hypothalamus/pituitary disorders
- hypopituitarism
- growth hormone (GH) deficiency
- diabetes insipidus (DI)
- central hypothyroidism
- secondary hypogonadism, including secondary amenorrhea, functional hypothalamic amenorrhea (FHA), or delayed puberty/primary amenorrhea
- acromegaly and gigantism
- hyperprolactinemia
- syndrome of inappropriate antidiuretic hormone secretion (SIADH)
- thyroid disorders
- primary hypothyroidism
- primary hyperthyroidism
- osteoporosis
- adrenal dysfunction
- adrenal insufficiency
- hypercortisolism (Cushing’s syndrome)
- parathyroid dysfunction
- hyperparathyroidism/hypoparathyroidism
- ovarian dysfunction
- polycystic ovary syndrome (PCOS)
- primary ovarian insufficiency (POI)
- testicular dysfunction
- islet cells of the pancreas
- DM
- type 1 (T1DM)
- type 2 (T2DM)
- multiple endocrine neoplasia type 1 (MEN1; Lonnemann, n.d.; Pituitary Foundation, n.d.)
****DM, thyroid dysfunction, and osteoporosis are common disorders of the endocrine system and are discussed in depth in the NursingCE educational modules Diabetes, Thyroid Dysfunction, and Osteoporosis and Bone Health. They will not be explored in detail in this educational offering.
Anatomy and Physiology of the Endocrine System
The endocrine system consists of glands that produce and secrete hormones to regulate cell and organ activity as well as the body's growth, metabolism, sexual function, and development. These hormones serve as the body's chemical messengers, which transfer information from one organ to another, coordinating functions between various parts of the body. The integral parts of the endocrine system include the hypothalamus, pituitary, thyroid, adrenals, pancreas, parathyroids, pineal body, and ovaries/testes. Each gland secretes a set of hormones that help regulate the body's functions, much like a thermostat regulates the temperature in a building. The system regulates itself based on a feedback system that involves stimulating hormones and releasing hormones; it is responsible for maintaining a balance of hormone levels within the bloodstream. Releasing hormones are sent to the pituitary from the hypothalamus, prompting the pituitary to secrete various stimulating hormones. The stimulating hormones then signal the target glands to release hormones into the circulation. As the circulating level of the desired hormone from the target gland increases, the hypothalamus secretes less of the releasing hormone and/or the pituitary gland decreases the secretion of the stimulating hormone. This process signals the target gland to decelerate its secretion (Kemp, 2019). Figure 1 illustrates the endocrine system and its glands.

As shown in Figure 1, the thymus is positioned beneath the sternum and contains lymphatic tissue. It reaches its maximum size during puberty and then slowly atrophies. The thymus secretes the hormones thymopoietin and thymosin, which promote peripheral lymphoid tissue growth. The thymus's primary role is to produce T lymphocytes (T-cells), which are crucial for cell-mediated immunity (Ignatavicius et al., 2018).
The hypothalamus appears within the lower central part of the brain and is positioned above the pituitary gland and brain stem (see Figures 1 and 2). It is comparable to the size of an almond and is fundamental for regulating body temperature, metabolism, and satiety. It receives signals from systemic hormone levels and parts of the nervous system to regulate the pituitary's function (Ignatavicius et al., 2018).

The primary hormones produced by the hypothalamus include the following:
- antidiuretic hormone (ADH, or vasopressin),
- corticotropin-releasing hormone (CRH),
- gonadotropin-releasing hormone (GnRH),
- growth hormone-releasing hormone (GHRH),
- growth hormone-inhibiting hormone (GHIH, or somatostatin),
- oxytocin,
- prolactin-releasing hormone (PRH),
- prolactin-inhibiting hormone (PIH, or dopamine), and
- thyrotropin-releasing hormone (TRH; Sargis, 2015; Shahid et al., 2020; Welt, 2019).
The hypothalamus acts as a central coordinator for the entire endocrine system. Hypothalamic dysfunction can result from tumors, infection, or head injuries, as well as iatrogenic factors such as surgery, medications, or radiation therapy. Dysfunction of this gland can lead to disturbances in appetite, sleep, thirst, mood, sexual function, growth, excretion, breastfeeding, and labor. Although the hypothalamus generates oxytocin and ADH, they are both transferred to the posterior pituitary for excretion. The hypothalamus also directly affects appetite through the secretion of orexin and ghrelin—both appetite stimulants—and receives feedback from adipose tissue via the hormone leptin, which is an appetite suppressant (Sargis, 2015; Shahid et al., 2020; Welt, 2019).
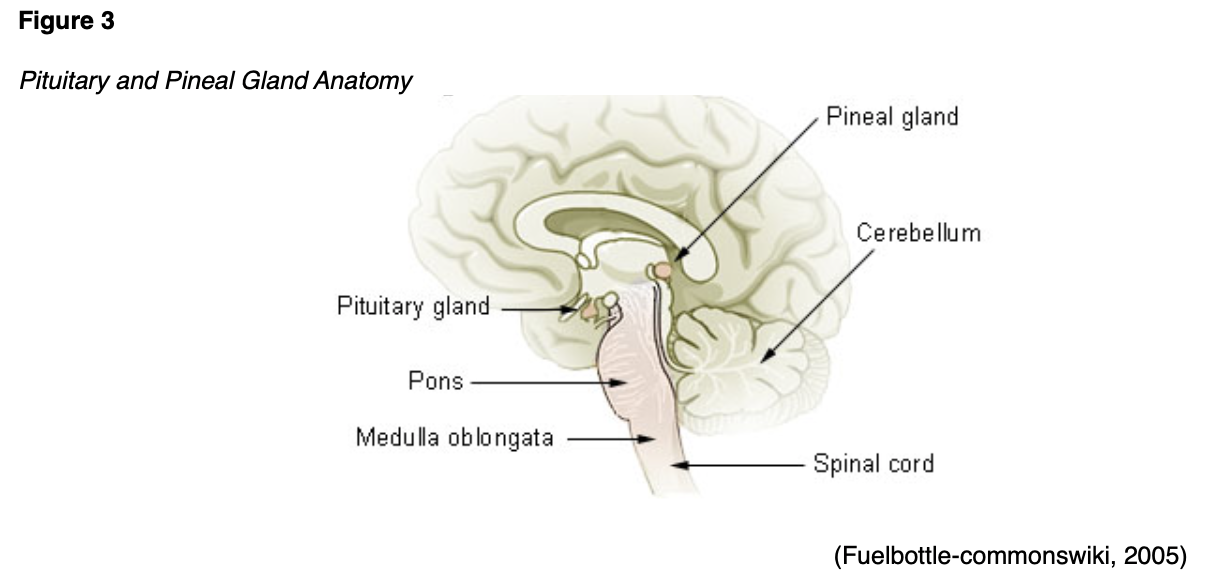
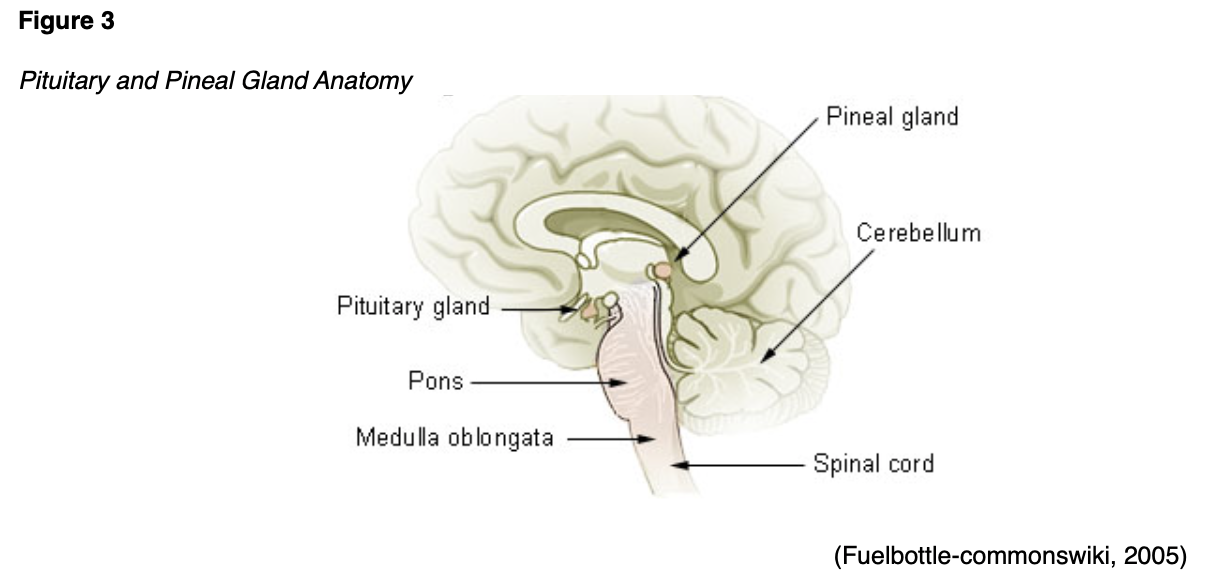
As shown in Figure 3, the pituitary is about the size of a pea and located beneath the hypothalamus.
Based on input from the hypothalamus and continuous monitoring of circulating hormone levels, the pituitary produces hormones that control the function of the other endocrine glands. Hypopituitarism occurs if the pituit
...purchase below to continue the course
ary does not produce a hormone or if it produces an insufficient amount. In contrast, hyperpituitarism occurs when the pituitary produces excess hormones (Kemp, 2019). Examples of the hormones regulated by the hypothalamic/pituitary system are listed in Table 1.

The pituitary gland contains two parts, the anterior and posterior lobes, which produce several hormones (Kemp, 2019). See Table 2 for the hormones produced in each area and their function.

The pineal gland—sometimes called the pineal body—is found in the middle of the brain (see Figures 1 and 3). This gland secretes melatonin in response to signals from the retinal ganglion cells to regulate the sleep-wake cycle (Aulinas, 2019; Kemp, 2019). The thyroid gland is located at the anterior of the neck and produces hormones that regulate metabolism (see Figures 1 and 4).

In children, the thyroid supports bone growth, brain development, and nervous system development. In adults, it also helps maintain normal blood pressure (BP), heart rate (HR), muscle tone, and reproductive functions. The thyroid gland also regulates body temperature, metabolism, and calcitonin, as well as impacting the way tissues outside the thyroid function. There are two primary hormones generated by the thyroid gland: thyroxine (T4) and triiodothyronine (T3). As demonstrated in Figure 5, the release rate of T3 and T4 is controlled by the anterior pituitary gland and hypothalamus, which acts as a sensory controller. The process is initiated by the hypothalamus, which emits thyrotropin-releasing hormone (TRH). TRH prompts the release of thyroid-stimulating hormone (TSH) from the anterior pituitary gland. TSH is critical for modulating the release of the T4 by the thyroid, which is then converted to T3. The amount of TSH that the pituitary releases into the bloodstream depends on the amount of T4 that the pituitary perceives, as it functions on a negative feedback system. The pituitary is constantly measuring the amount of T3/4 and responding to changes to maintain an appropriate balance. If the pituitary senses insufficient T4, it will boost TSH production, signaling the thyroid gland to produce more T4. Once T4 reaches an acceptable level within the blood, TSH production decreases (American Thyroid Association, n.d.).

The parathyroid glands are embedded in the thyroid gland's surface, as shown in Figures 1 and 4. The two pairs of parathyroid glands release parathyroid hormone (PTH), which regulates serum (blood) calcium and phosphorus as well as bone metabolism. PTH extracts calcium from bones to increase serum calcium levels when they are too low and reduces calcium excretion through the kidneys. It also increases the production of calcitriol by converting calcidiol to calcitriol in the kidneys, which helps increase calcium absorption through the digestive system (Kemp, 2019; National Institute of Diabetes and Digestive and Kidney Diseases, 2019).
The adrenal glands are located superior to the kidneys and are comprised of two parts: the medulla and cortex (see Figures 1 and 6).

The adrenal cortex—the outermost portion of the adrenal gland—produces corticosteroids that play a vital role in regulating metabolism, salt and water balance, the immune system, and sexual function (Kemp, 2019). ACTH is responsible for stimulating the adrenocortical cells to secrete cortisol, a glucocorticoid, in varying amounts depending on nervous system signals conveyed to the hypothalamus, which secretes corticotropin-releasing hormone (CRH; El Sayed et al., 2020). The adrenal gland also secretes the mineralocorticoid aldosterone (Welt, 2019). The medulla—the inner part of the adrenal gland—produces catecholamines, including epinephrine (adrenaline) and norepinephrine (fight or flight hormones). Catecholamines help the body deal with emotional or physical stress by increasing HR and BP (Kemp, 2019).
The adrenal cortex makes three types of steroids: mineralocorticoids, glucocorticoids, and sex hormones. These hormones regulate metabolism, immune system, BP, and responses to stress or other essential functions. When the adrenal glands do not produce enough hormones, adrenal insufficiency, or Addison's disease, can result (Johns Hopkins Medicine, n.d.). The adrenal gland is regulated by a negative feedback system involving the hypothalamus, which secretes CRH, triggering the corticotrophs in the anterior pituitary to secrete ACTH. Increasing levels of adrenal hormones in the circulation inhibit the secretion of both CRH and ACTH, completing the hypothalamus-pituitary-adrenal (HPA) axis (El Sayed et al., 2020). Understanding normal cortisol physiology is important to understand adrenal dysfunction. Cortisol is among the key hormones produced by the cortex, which helps control the body's use of fats, proteins, and carbohydrates; suppresses inflammation; regulates BP via vascular tone (a decrease in cortisol production is associated with a decrease in BP); increases blood glucose (BG); and may decrease the formation of bone tissue. Cortisol impacts the body’s response to stress and stressful situations (cortisol is a fight or flight hormone). Increased cortisol is needed to cope with acutely stressful situations such as surgery. An inadequate release of cortisol in these situations can be fatal. Cortisol also regulates the sleep/wake cycle and provides a boost of energy during periods of increased stress. Varying amounts of cortisol are secreted throughout the day: the lowest levels occur at midnight, and the highest levels happen early in the morning. Aldosterone is a mineralocorticoid hormone that regulates BP as well as sodium and potassium levels. Aldosterone signals the kidneys to retain more sodium and excrete potassium into the urine, also helping regulate the pH of blood. Dehydroepiandrosterone (DHEA) and androgenic steroids are precursor hormones that are produced by the cortex and converted in the ovaries of females to estrogens and in the testes of males to androgens (Johns Hopkins Medicine, n.d.; University of California Los Angeles Health, n.d.).
The gonads—testes and ovaries (see Figures 1 and 7)—are the reproductive glands and the main source of sex hormones. They are controlled by the hypothalamus-pituitary-gonadal (HPG) axis via the secretion of GnRH, LH, and FSH. The hormones primarily produced by the testes are called androgens; the most important of these is testosterone, which controls facial hair, pubic hair, and sexual development. In males, testosterone helps regulate spermatogenesis and libido (sexual desire), as well as muscle/bone mass in both sexes. In females, the ovaries produce both progesterone and estrogen along with testosterone. These hormones control the development of secondary sexual characteristics such as breasts, pubic hair, menstruation, libido, and ovulation. Estrogen also has an impact on libido, muscle/lipid mass, and fertility in males. These androgens and estrogen are excreted in smaller quantities by the adrenal gland (Hormone Health Network [HHN], 2018, 2020; Kemp, 2019). To function properly, affect the gonads, and promote hair growth, testosterone must first be converted to estradiol by aromatase; it must be converted to dihydrotestosterone by the enzyme 5-alpha-reductase to act on bone tissue (Snyder, 2020).

The physiologic functioning of the reproductive system relies heavily on the appropriate secretion of numerous hormones. The HPG axis is central to this action, which involves the production of GnRH by the hypothalamus, followed by the secretion of LH and FSH by the anterior pituitary. LH and FSH bind to G protein-coupled receptors and trigger the secretion of androgens by the testes and estrogen and progesterone by the ovaries (as well as some estrogen secretion by the adrenal gland). LH is responsible for triggering the secretion of progesterone and testosterone by the ovaries. In premenopausal adolescent and adult females, a surge in LH also prompts ovulation. FSH triggers the secretion of estrogen and the process of ovum development. Estrogen levels are higher around ovulation and decrease during menstruation (El Sayed et al., 2020; HHN, 2018, 2019, 2020; Shahid et al., 2020).
In males, LH triggers the secretion of testosterone by the testes, and FSH facilitates spermatogenesis. Testosterone is crucial for the development of secondary sexual characteristics during puberty, including penile/testicular enlargement, hair growth, voice deepening, increase in bone and muscle mass, and an increase in skeletal height. Beyond puberty, testosterone production facilitates spermatogenesis, libido, and the maintenance of bone and muscle mass (El Sayed et al., 2020; HHN, 2018, 2019, 2020; Shahid et al., 2020).
The pancreas (see Figures 1 and 8) is located behind the stomach in the posterior portion of the abdomen. It has both digestive and hormonal functions that are termed endocrine (insulin) and exocrine (digestive enzymes). Insulin and glucagon are the two hormones secreted by the pancreas that aid in regulating BG. Dysfunction within the pancreas can lead to DM (Kemp, 2019).

Hormonal Release Mechanisms
The hypothalamus and pituitary glands monitor target hormone levels continuously. When these levels decline, the hypothalamus secretes releasing hormone, which triggers the pituitary gland to secrete stimulating or pituitary hormones. As listed in Table 2, the pituitary hormones have numerous and varied effects on the human body. These trophic hormones trigger their target glands to increase hormone production. When target gland hormone levels increase, releasing and stimulating hormone secretion decreases. This process is known as the hypothalamus-pituitary axis. This mechanism can be somewhat complicated, as many of these hormones also exhibit secondary effects. For example, PRL affects the hypothalamus-pituitary-gonadal axis, as increased circulating levels of PRL inhibit the hypothalamic secretion of GnRH, leading to the reduced secretion of LH/FSH by the pituitary and the various sex hormones (estrogen, progesterone, and androgens) by the target glands. TRH, which is primarily responsible for triggering the secretion of TSH by the anterior pituitary, also appears to facilitate the production of PRL (El Sayed et al., 2020; Shahid et al., 2020; Welt, 2019; Willis, 2018).
Chemical regulation occurs when endocrine glands that are not regulated by the pituitary gland are controlled by other substances that stimulate gland secretion. Examples include BG levels that regulate the release of glucagon and insulin by the pancreas and serum calcium levels, which affect the release of PTH by the parathyroid glands. The third method for hormonal control involves the central nervous system, which may provide sensory input through the hypothalamus or directly to one of the glands of the endocrine system, such as the regulation of melatonin production by the pineal gland in response to ambient light or the release of catecholamines by the adrenal gland in response to stress (El Sayed et al., 2020; Shahid et al., 2020; Welt, 2019; Willis, 2018).
Older adults usually experience changes to their endocrine system function as part of the aging process. Some of the most common age-related changes include:
- declining sex hormones;
- decreasing aldosterone levels, which can contribute to orthostatic hypotension;
- increasing PTH, which may lead to osteoporosis;
- rising FSH, LH, and norepinephrine levels; and
- changing glucose metabolism, such as increased BG when faced with physical or mental stress (Willis, 2018).
For learners who are eager to access additional content related to the endocrine system and endocrine disorders, please see the following NursingCE courses:
- Endocrine and Hormonal Disorders Part 1: Anatomy and Physiology
- Endocrine and Hormonal Disorders Part 2: Hypopituitarism and Other Hormone Deficiencies
- Endocrine and Hormonal Disorders Part 3: Syndromes of Excessive Hormone Secretion
- Endocrine and Hormonal Disorders Part 4: Adrenal Gland Disorders
- Diabetes
- Osteoporosis
- Thyroid Dysfunction
- Sexual Dysfunction
References
American Thyroid Association. (n.d.). Thyroid function tests. Retrieved May 29, 2020, from https://www.thyroid.org/thyroid-function-tests/
Aulinas, A. (2019). Physiology of the pineal gland and melatonin. In: Feingold K. R., Anawalt, B., & Boyce, A., et al. (Eds.). Endotext [Internet]. MDText.com, Inc. https://www.ncbi.nlm.nih.gov/books/NBK550972/
CFCF. (2013). Exocrine and endocrine pancreas. [Image]. https://commons.wikimedia.org/wiki/File:2424_Exocrine_and_Endocrine_Pancreas.jpg
CFCF. (2014). Thyroid and parathyroid. [Image]. https://commons.wikimedia.org/wiki/File:Illu_thyroid_parathyroid.jpg
Chapman, I. M. (2019). Gigantism and acromegaly. In Merck Manual of diagnosis and therapy. Merck Sharp & Dohme. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/pituitary-disorders/gigantism-and-acromegaly.
Dieleman, J. L., Baral, R., Birger, M., Bui, A. L., Bulchis, A., Chapin, A., Hamavid, H., Horst, C., Johnson, E. K., Joseph, J., Lavado, R., Lomsadze, L., Reynolds, A., Squires, E., Campbell, M., DeCenso, B., Dicker, D., Flaxman, A. D., Gabeert, R,. . . . Murray, C. J. L. (2016). US spending on personal health care and public health., 1996-2013. JAMA, 316(24), 2627-2646. https://doi.org/10.1001/jama.2016.16885
El Sayed, S. A., Fahmy, M. W., & Schwartz, J. (2020). Physiology, pituitary gland. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK459247/
Evrik. (2014). Adrenal glands. [Image]. https://commons.wikimedia.org/wiki/File:Illu_adrenal_gland.jpg
Fuelbottle-commonswiki. (2005). Pituitary and pineal glands. [Image]. https://commons.wikimedia.org/wiki/File:Illu_pituitary_pineal_glands.jpg
Häggström, M. (2009). Thyroid hormones [image]. https://commons.wikimedia.org/wiki/File:Thyroid_system.svg
Hormone Health Network. (2018). Estrogen. https://www.hormone.org/your-health-and-hormones/glands-and-hormones-a-to-z/hormones/estrogen
Hormone Health Network. (2019). Pituitary gland. https://www.hormone.org/your-health-and-hormones/glands-and-hormones-a-to-z/glands/pituitary-gland
Hormone Health Network. (2020). Testosterone and androgens. https://www.hormone.org/your-health-and-hormones/glands-and-hormones-a-to-z/hormones/testosterone
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2018). Medical-surgical nursing concepts for interprofessional collaborative care (9th ed.). Elsevier.
Johns Hopkins Medicine. (n.d.). Adrenal glands. Retrieved July 18, 2020, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/adrenal-glands
Kemp, S. (2019). Anatomy of the endocrine system. https://www.emedicinehealth.com/anatomy_of_the_endocrine_system/article_em.htm
LadyofHats. (2010). Endocrine reproductive system. [Image]. https://commons.wikimedia.org/wiki/File:Endocrine_reproductive_system_en.svg
Lonnemann, E. (n.d.). Metabolic/endocrine disorders. Retrieved July 16, 2020, from https://www.physio-pedia.com/Metabolic/Endocrine_Disorders
National Institute of Diabetes and Digestive and Kidney Diseases. (2019). Primary hyperparathyroidism. https://www.niddk.nih.gov/health-information/endocrine-diseases/primary-hyperparathyroidism
OpenStax College. (2013). The endocrine system. [Image]. https://commons.wikimedia.org/wiki/File:1801_The_Endocrine_System.jpg
Pituitary Foundation. (n.d.). Pituitary conditions. Retrieved July 15, 2020, from https://www.pituitary.org.uk/information/pituitary-conditions/
Sargis, R. M. (2015). An overview of the hypothalamus. https://www.endocrineweb.com/endocrinology/overview-hypothalamus
Shahid, Z., Asuka, E., & Singh, G. (2020). Physiology, hypothalamus. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK535380/
Snyder, P. J. (2020). Testosterone treatment of male hypogonadism. UpToDate. https://www.uptodate.com/contents/testosterone-treatment-of-male-hypogonadism
University of California Los Angeles Health. (n.d.). Cushing's disease. Retrieved July 18, 2020, from http://pituitary.ucla.edu/cushings-disease#:~:text=Cushing's%20disease%20is%20a%20serious,by%20the%20normal%20pituitary%20gland
Was a bee. (2009). Hypothalamus. [Image]. https://commons.wikimedia.org/wiki/File:Hypothalamus.gif
Welt, C. K. (2019). Hypothalamic-pituitary axis. UpToDate. https://www.uptodate.com/contents/hypothalamic-pituitary-axis
Willis, L. M. (2018). Anatomy & physiology made incredibly easy (5th ed.). Lippincott, Williams, & Wilkins.