The purpose of this activity is to enable the learner to acquire a basic knowledge of the issues related to the new graduate nurse and role transition.
...purchase below to continue the course
may not be the deciding factor for that position, they may be important in determining the best overall employment package in the event of multiple job offers. In addition, this displays a vested interest in a career and choosing the right fit, instead of just finding a job. During the interview, the new graduate should tell a story about their skills and capabilities. Compassion, empathy, and caring are skills and attitudes that are as important as clinical knowledge. It may be appropriate and helpful to share about instances that have called for these skills and behaviors with patients, co-workers, family members, or in previous employment roles (ANA, n.d.).
A professional appearance is a vital component of an interview, to not only impress the interviewers, but to demonstrate a level of self-respect and seriousness about the position. The ANA (n.d.) suggests wearing a blue or grey suit or a conservative dress. Jewelry, perfume, or cologne should be kept to a minimum, and women should wear low-heeled shoes. During the interview, keep the energy level up; regardless of the number of interviews, each one should be approached with high energy and excitement for the opportunity (ANA, n.d.).
Follow-up is very important after the interview, and candidates are encouraged to send out a thank-you note in either hand-written form or by e-mail. This should not be perceived as bothering the organization, but rather reaching out just to "check-in" about the position as well as any other opportunities that may have become available. Recruiters are very busy with multiple candidates, and following up may help an individual stand out as being responsible and interested in the position (ANA, n.d.).
Where to Work
Nursing students may have heard of the many available opportunities and even heard unrealistic annual salaries quoted. The reality is that an entry-level nurse will likely have to work up to those ideal employment situations. It is important to set career goal. While you may not start out in your ideal position, goals will help you work toward that "perfect" role. For some, it is critical care, pediatrics, or the medical-surgical unit. While it is important to understand salary, be careful about unrealistic salary expectations, and be flexible about shifts, pay, and available units. Most healthcare facilities pay a shift differential that increases the overall salary and will allow for an internal transfer to a more desirable unit within six months of employment. Consider the reputation of a facility before applying, as a well-respected hospital system can further a nurse’s career options in the future (Walsh, 2018).
Transition to Practice
Consider an organization that offers a nurse residency program or has special new graduate nurse fellowships designed to support the transition from student nurse to graduate nurse; these can help promote the growth of clinical skills and perceived support during this transitional time. Most hospitals that offer residency programs are either Magnet-designated facilities or larger teaching hospitals, making these options even more attractive (Walsh, 2018).
Regardless of whether the opportunity to enter a nurse residency program is available or not, the transition from the academic setting to actual practice has implications personally and professionally. Let's look a little more in-depth into nurse residencies (Walsh, 2018). Nurse residencies have proven success in acclimating a new nurse to practice in several areas. In a recent study from Central Florida related to nurse residency programs, the following themes arose from the data as the top categories related to personal and professional growth:teamwork, gratitude, asking questions, the art of nursing, and change (Fowler et al., 2018). These concepts are part of the role development and professional growth of any new nurse and lead to the needed knowledge, skills, and attitude of an expert nurse, which should be the ultimate goal for all nurses (Walsh, 2018).
The first year in practice can be a difficult one. New nurses see the challenges in healthcare and the disparities between the real world and the ideal one that is taught in school and even on the NCLEX exam. It has been noted across the literature that in the early months of transition to practice, new nurses lack confidence in their abilities and are often concerned about their knowledge of medications, equipment, and nursing care, yet are afraid to ask questions for fear of jeopardizing their new employment. Having mentors, preceptors, or other experienced nurses to support the transition can help a new nurse learn to manage time effectively and allow for the competent and safe delivery of care (Murray et al., 2019).
Getting Organized
Time management is a HUGE undertaking for the new graduate nurse. During school, most students are responsible for the care of one to two patients over a clinical day with the support of the assigned nurse on the unit as well as clinical faculty. Occasionally, during the final semester, a student may manage three or four patients on a single day. The reality and responsibility of a full patient load (which may be six or more patients, depending on the unit and facility) without support from another nurse or faculty member may be terrifying for a new nurse. A slow transition into this role should occur, but not all facilities are able to provide that transition time. It is crucial that the new nurse develops time management skills. Many nurses report a lack of time during their shift to complete all the activities or tasks that are required for the care of their patients. They feel pressured to complete the patient care in the manner they were taught during school, providing individualized time for each patient, yet also chart, administer medications, review the records, call primary healthcare providers for further orders, and all the other tasks required to properly manage care in an interdisciplinary fashion. Murray et al. (2019) notes that new graduate nurses report a conflict between time management and patient safety with the fear of making a mistake as their greatest worry. Experiential learning through simulation or actual experiences during the orientation time can allow for the development of priorities and time management skills and lead to improved confidence, knowledge, and attitude for a nurse (Murray et al., 2019).
Seasoned nurses often develop a cheat sheet or to-do list to organize their day. This is simply a way of organizing data and tasks. Here are just a few ideas:
1. Make a list of patients, ordered by their room number or the time of their clinical visit.
2. Cluster tasks based on the time of day, such as all 8 a.m. tasks listed in a group. High-acuity patients or time-sensitive tasks should be prioritized.
3. Organize patients based on their healthcare provider(s), so that all the data for each physician, NP, or PA is grouped together and prepared for providing updates on the patients as efficiently as possible.
4. Create task lists for recurring events such as fluid intake and output, vital signs, or assessments.
5. Make a list of important phone numbers and codes to ensure they are available in an emergency (Trivedi-Mair, 2016).
These are just a few ideas, but each nurse must find what works for them. New nurses should feel comfortable asking other nurses in the unit what works for them and adjusting to meet their own needs and the needs of their patient population.
Providing and receiving report as nurses come and go from a shift is a vital skill. Patient errors can occur from omissions or miscommunications during change-of-shift reporting. There are methods to improve efficiency and accuracy while reporting, such as recording the information in the same order each time. For instance, listing the patient’s name, room number, diagnosis, a review of their condition prior to the shift, then any changes that occurred during the shift, along with medication or treatment administration is one method. Other ideas include writing down the report from the previous shift in one color ink and adding information from the current shift in another color ink. Since most charting is now done online, some hospitals are using online reporting as well. It may still be a good idea to verbally point out the main concerns and interventions related to a patient each shift. Other hospitals use bedside reporting as a hand-off tool. This can be a great way to include the patient as part of the hand-off and has been shown to be both effective and safe (Trivedi-Mair, 2016).
Charting can either help a nurse stay organized and on task or become a source of disorganization and stress if not consistently maintained. It is very easy to forget actions taken on patients such as PRN medications, complaints, or interventions if not charted immediately. EMRs typically require that nurses chart at the bedside, or at the nursing station on a computer as the shift unfolds. Getting behind on charting can be of detriment to any nurse and can leave the nurse charting for extended periods long after their shift has ended. Charting consistently throughout the shift is the most effective and safe method (Trivedi-Mair, 2016).
When feeling overwhelmed with all the tasks that need to happen in a short period of time, a new nurse should be coached to slow down and make a priority list. They should create a timetable and determine what tasks may require help. It is always a good idea for a nurse to team up with other nurses that can work collectively to help each other in times of trouble when they get behind. The nurse should avoid letting the nursing unit control them, but rather take charge of the environment that they are responsible for (Trivedi-Mair, 2016).
Caring for Patients
The World Health Organization's (WHO, 2018) definition of patient safety is to do no harm. Specifically, it is "the absence of preventable harm to a patient during the process of healthcare and reduction of risk of unnecessary harm associated with health care to an acceptable minimum" (para. 3). Considering the focus on safety and the realization of responsibility, new nurses have to manage patient care, provide advocacy to their patients, and drive interprofessional and evidence-based care for their patients. This role can be somewhat overwhelming. The landmark publication in 2000 by the IOM with a focus on safety, To err is human: Building a safer health system, identified the need for safety within healthcare systems worldwide. This prompted many healthcare leaders as well as nursing academics to focus on safety and envision how that can be incorporated throughout the nursing curriculum and into the transition to practice (Murray et al., 2019). Thus, it is well-documented and well-known that patient safety and positive outcomes are at the forefront of the new graduate's mind, as well as the organizations that hire them. Finding the best ways to foster the growth and transition from novice to expert as a nurse can be the challenge. Up to 55% of nurses with under five years of experience report having made a medication error. The errors stem from nursing inexperience, being rushed, technology, high patient acuity levels, or understaffing on the unit (Treiber & Jones, 2018). Errors not only lead to poor patient outcomes, including potential harm to the patient, but also induce distress to the nurse who has made the error. Specific themes rose out of the root cause analysis of these errors, including failure to follow hospital policies, working within the nurse's scope of practice, knowledge of medications, and prioritization. Knowing the areas of concern leads to opportunities to focus on education, experiential learning, and development of expertise for the new nurse entering practice (Murray et al., 2019).
Safe Medication Administration
Medication errors can occur in any healthcare setting, as well as within the home. These errors may result from errors in prescribing, transcribing, communication, packaging and labeling, distribution, and other practices (The Agency for Healthcare Research and Quality [AHRQ], 2017).
Nurses have a pivotal role in optimizing individual performance and controlling environmental factors to reduce medication errors. Medication management is an important responsibility that has been said to involve approximately 40% of a nurse’s time. It not only involves the nurse preparing, calculating, checking; and administering medications, but also updating their knowledge about medications, monitoring the effectiveness of the treatment, observing for any drug reactions, interactions or adverse events that might occur, and educating patients about their medications (AHRQ, 2017).
There are three medication safety issues identified by the Joint Commission, National Patient Safety Goals as a concern: labeling of medications, anticoagulant therapy, and medication reconciliation (The Institute for Safe Medication Practices [ISMP], 2014).
The way medications are labeled and packaged can lead to medication errors. Labels may cause confusion leading to errors when the following situations occur: (a) marketing distractions, (b) labels or drug names look alike, (c) drug names are the same, but the drugs have different purposes, (d) information on the label may be difficult to find, and (e) warning information may be hidden. A manufacturer may want to draw attention to its product by using eye-catching adjectives or phrases, causing distractions for the consumer. Drugs may come in different forms (i.e., capsules, gel tabs) and in different strengths; however, the drug companies often package them in containers that look alike. Drug companies that have a well-known brand name for one product may introduce a new product under the same/similar name. The two products may treat different medical conditions (i.e., a stool softener versus a laxative). Important information about a drug may be located underneath the label. The label reads “peel back” causing individuals to miss the instructions or to assume that they cannot peel back the label without buying the drug. Warning information regarding a drug, such as allergic ingredients, might be located in a less obvious place on the medication container leading individuals to miss the information or become confused (ISMP, 2014).
Anticoagulant drugs (i.e., dabigatran etexilate [Pradaxa], rivaroxaban [Xarelto], apixaban [Eliquis], and warfarin [Coumadin]) are widely used for both the treatment and prophylaxis of venous thromboembolism; these drugs frequently cause adverse medication incidents in hospitals. Admission, discharge, and surgery were found to be the times adverse incidents most frequently occurred. During admission and surgery, studies indicate that prescribing excess anticoagulant was the most frequent problem. During discharge, prescribing insufficient anticoagulant was the most frequent problem. Management of anticoagulant therapy involves being aware and observant for the signs and symptoms associated with bleeding caused by over-dosing and clotting caused by under-dosing of anticoagulants, as both conditions can be fatal (Henriksen et al., 2017; The Joint Commission, 2020b).
Medication reconciliation is the process of creating an accurate list of all mediations a patient is taking to avoid errors. The medication list should include the drug name, dosage, frequency, and administration route. To ensure the correct medications are administered, the medication list should be compared to the physician's orders at the time of admission, when transferred from one hospital unit to another, and at the time of discharge. Errors that have the potential of occurring during medication reconciliation include omitting a particular medication, listing the medication more than once, listing an incorrect dose, and/or a drug interaction (Institute for Healthcare Improvement [IHI], 2017).
Prevention of Medication Errors
Medications are chemicals that affect the body. Every medication has the potential to cause adverse effects. These are undesired, inadvertent, and harmful effects of the medication. Adverse effects can range from mild to severe, and some can be life-threatening. With concurrent use of medications, there is a potential for an interaction. Medications can also interact with foods and dietary supplements. Contraindications and precautions for specific medications are conditions (i.e., diseases, age, pregnancy, lactation) that make it risky or unsafe for patients to use that medication at that time (Potter et al., 2017). In order to prevent medication errors, the nurse’s responsibilities include:
Having knowledge of federal, state (nurse practice acts), and local laws, and facilities’ policies that govern the prescribing, dispensing, and administration of medications.
Preparing, administering, and evaluating patients’ responses to medications.
Developing and maintaining an up-to-date knowledge base of medications they administer, including uses, mechanisms of action, routes of administration, safe dosage range, adverse and side effects, precautions, contraindications, and interactions.
Maintaining knowledge of acceptable practice and skills competency.
Determining the accuracy of medication prescription
Reporting all medication errors.
Safeguarding and storing medications appropriately (Potter et al., 2017).
The anticipation of adverse effects, interactions, contraindications, and precautions is an important component of patient education. Both the nurse and the patient or caregiver should know the major adverse effects a medication may cause. Early identification of adverse effects allows for timely intervention to minimize harm. Students in nursing school used to be taught the five rights of medication administration, yet those five rights have morphed into a minimum of ten rights, and some literature sources suggest even more rights. This educational training will employ The 10 Rights of Safe Medication Administration, as these have been noted to facilitate the prevention of medication errors (Jones & Treiber, 2018).
1. The right patient- A patients' identification should be verified before each medication administration. The Joint Commission requires two patient identifiers. Acceptable identifiers include the patient's name, facility-assigned identification number, telephone number, birth date, or other people-specific identifiers, such as a photo identification card. Nurses also use barcode scanners to identify patients. The nurse should check for allergies by asking patients, checking for an allergy bracelet or medal, and checking the MAR.
2. The right medication-The nurse should verify the completeness and clarity of all medication prescriptions. Medication labels should be read and compared with the MAR three times: before removing the container from the pharmacy dispenser, when removing the amount of medication from the container, and in the presence of the patient before administering the medication. Leave unitdose medication in its package until administration. See Table 1 below for examples of commonly confused medication names.
Table 1
Commonly Confused Medications

(ISMP, 2016)
3. The right dose-A unit-dose system should be used to decrease errors. A unit dose can be packaged in a vial, a blister pack, or a pre-filled syringe. Many hospitals and health care facilities use unit dose packaging to reduce the risk of medication errors. If not available, calculate the correct medication dose and check a drug reference guide to make sure the dose is within the usual range. Another nurse should verify the dose if the primary nurse is uncertain of the calculation. Prepare medication dosages using standard measurement devices, such as graduated cups or syringes. Some medication dosages require a second verifier or witness, such as some cytotoxic medications. Automated medication dispensing systems use a machine to control the dispensing of medications.
4. The right time-Administer medication on time to maintain a consistent therapeutic blood level. It is generally acceptable to administer a medication 30 min before or after the scheduled time. Refer to the drug reference or the facility’s policy for exceptions.
5. The right route-The most common routes of administration are oral, topical, subcutaneous, intramuscular (IM), and intravenous (IV). Additional administration routes include sublingual, buccal, intradermal, transdermal, epidural, inhalation, nasal, ophthalmic, otic, rectal, vaginal, intraosseous, and via enteral tube. Select the correct preparation for the prescribed route (otic vs. ophthalmic topical ointment/drops).
6. The right documentation-The nurse should immediately record pertinent information and include the patient’s response to the medication after administration, not before.
7. The right patient education-A nurse should inform patients about their medications: their purpose, what to expect, how to take them, and what to report. To individualize the teaching, the nurse can first determine what the patient already knows about their medication to establish what they need/want to know about their medication.
8. The right to refuse-Patients have the legal right to refuse any medication. The nurse should attempt to explain the consequences, inform the provider, and carefully document the refusal.
9. The right assessment-Nurses should diligently collect any essential data before and after administering any medication. For example, measure the apical heart rate before giving digoxin (Lanoxin).
10. The right evaluation-The nurse should follow up with patients after administration to verify therapeutic effects as well as side and adverse effects (Jones & Treiber, 2018).
Nurses should wear gloves when administering medications, practice hand hygiene before and after each patient interaction, and dispose of all supplies appropriately, using sharps containers and correct waste containers. For anything contaminated with blood or body fluids, biohazard waste containers should be utilized (Potter et al., 2017).
Additionally, it should be noted that the nurse has the right to deliver medications safely. The concept of nurses’ rights is covered in the ANA Nurses’ Bill of Rights regarding a safe working environment. The Nurses’ Bill of Rights was created to support nurses in workplace issues, including staffing concerns, mandatory overtime, and health or safety issues. In addition to the ANA Nurses' Bill of Rights, Jones and Treiber (2018) identified the rights of the nurse to deliver safe medication, including:
1. The right to sufficient time to administer medications.
2. The right workload that allows for safe administration.
3. The right environment with minimal distractions.
4. The right to properly functioning equipment and technology.
5. The right to time to document all aspects of medication administration.
6. The right to call for help without repercussions or negative attitudes.
7. The right to have a voice about decisions that go into workload and the work environment (Jones & Treiber, 2018).
Medication errors can be significantly reduced by following the foundational five rights, the additional five rights of medication administration, along with an environment and culture that allows for the nurses' seven rights to administer medications safely (Jones & Treiber, 2018).
Not only associated with medications, but also with documentation is the following list of abbreviations. It is generally recognized to avoid these abbreviations. See Table 2 below:
Table 2
Error-Prone Abbreviation List

(Potter et al., 2017)
Infection Control
New nurses should be well-equipped to practice infection control to protect themselves, their patients, and their families from the dangers of infectious organisms within the healthcare environment. Basic concepts of hand hygiene before and after all patient care, including during medication administration, are often overlooked. Healthcare-associated infections (HAIs) are a significant cause of morbidity across all types of healthcare institutions; considered to be the most common complication of hospitalization. HAI is an infection that a patient acquires while receiving treatment for another medical or surgical condition. HAIs are associated with increased health care costs, extended hospital stays, medical complications, and poor patient outcomes, including death. Several organizations, such as the Centers for Disease Control and Prevention (CDC) and the Joint Commission have made significant progress in preventing specific HAIs through policy changes and developing benchmarks for standard of care practices. Catheter-associated urinary tract infections (CAUTIs), surgical site infections (SSIs), and multidrug-resistant organisms (MDROs) are three common types of HAIs (CDC, 2015; The Joint Commission, 2020a).
According to the CDC (2015), urinary tract infections are the most common type of HAI. A CAUTI can occur in any part of the urinary system, such as the urethra, bladder, ureters, or kidney. The most important risk factor for developing a CAUTI is the prolonged use of an indwelling urinary catheter. There are a number of ways an infection can occur. Some of the most common causes include contamination of the catheter upon insertion, improper or incomplete emptying of the drainage bag, or bacteria from a bowel movement may enter the catheter from poor hygiene practices or through fecal incontinence. The risk of infection can be reduced by using urinary catheters only when needed and by removing them as soon as possible. Proper aseptic technique should be routinely employed when inserting catheters, and the closed sterile drainage system should be consistently maintained (CDC, 2015; The Joint Commission, 2020a).
SSIs occur at the site of surgery. The CDC (2020) has identified 3 types of SSIs: (a) superficial incisional infections, which occur just in the area where the incision was made; (b) deep incisional infections, which occur in the muscle and the tissues surrounding the incision; (c) organ infections, which occur in any area of the body, a body organ, or a space between organs. Infections following surgery are most commonly caused by bacteria. Bacteria can infect a surgical site through a contaminated caregiver, surgical instruments, and/or bacteria already on the patient’s body (CDC, 2020).
MDROs are bacteria that are resistant to more than one antibiotic. This makes certain HAIs difficult to treat. This phenomenon occurs when antibiotics are taken for a long period of time or when an individual takes an antibiotic that is not necessary. MDROs can be spread by skin- to-skin contact or contact with contaminated equipment or surfaces. Infections occur most frequently in patients that are older, have a compromised immune system, have repeated hospitalizations, or have recently had surgery. Although treatment with antibiotics is difficult, they can be treated with specific antibiotics once the type of MDRO is identified (CDC, 2015; Office of Disease Prevention & Health Promotion, 2020).
Prevention
One of the most important ways to prevent HAIs is by adherence to responsible hand hygiene practices by all healthcare providers regardless of the healthcare setting. The National Patient Safety Goals require compliance with either the CDC (2020) or the WHO (2020) hand hygiene guidelines. See Table 3 for a description of the chain of events that must occur for pathogens to be transmitted from one patient to another via the hands of the healthcare worker.
Table 3
Chain of Events by the Healthcare Worker for Infection to Occur

The nurse has multiple opportunities to break the chain described above. Hand hygiene is the single most effective way to avoid infections in the healthcare environment. Hand hygiene applies to handwashing with soap and water, antiseptic hand rubs, or surgical hand antisepsis. Soaps (non-antimicrobial agents) are considered suitable for routine cleansing and removal of most transient microorganisms. When the risk for infection is high, alcohol- based hand rubs (antimicrobial agents) more effectively reduce bacteria. When the healthcare worker's hands are minimally soiled, alcohol-based hand rubs are considered suitable to use. If the healthcare worker's hands are visibly soiled, particularly with body fluids, soap and water should be used for handwashing (CDC, 2020; WHO, 2020).
Self-Care
Both new and seasoned nurses should practice self-care. Nurses spend their day providing care to others to promote the best patient outcomes; however, many neglect to care for themselves. It is well-known that one cannot give to others when their own cup is empty, which is why airlines always advise passengers to put on their oxygen mask before helping others. Self-care is a deliberate activity that one practices promoting mental, physical, and spiritual well-being. Halm (2017) noted that nurses are socialized to put themselves as a second priority behind their patients, yet the constant and overwhelming stress can lead to compassion fatigue and provider burnout. Many hospitals and healthcare organizations recognize the need for self-care and work to develop an environment that supports person- centric principles for nursing staff and other inter-professional teams. Self-care supports resiliency. Self-care may be as simple as getting enough rest, or may include practicing yoga, meditation/mindfulness, massage, or walking around the block. Proper nutrition, avoiding substances such as tobacco or alcohol, exercise, and adequate rest are basic building blocks for self-care. Nurses are often guilty of eating on the run, rarely engaging in exercise or going to the gym, and may delve into smoking or drinking to relieve stress. These poor health habits will lead to poor outcomes, which will in turn impact patient care negatively (Halm, 2017).
Despite the knowledge surrounding the dangerous repercussions of obesity, such as cardiovascular disease and type 2 diabetes, the prevalence of obesity among US nurses is estimated to be between 23% and 61%. Commonly, obesity is related to poor nutrition, a lack of cardiovascular exercise, or neglecting to practice stress-reducing activities. These health behaviors are destructive and can lead to chronic disease, absenteeism at work, turnover, and burnout. Nurses who do not practice healthy behaviors are less likely to encourage healthy behaviors in their patients. Even if they attempt to teach their patients about the value of healthy diets and exercise, there may be little influence on the patient if the nurse is not practicing what they preach. Nursing is a physically demanding job, and overweight, obese, and physically inactive nurses are more likely to experience low back pain and endure musculoskeletal injuries associated with patient care. Nurses who do not practice healthy lifestyle behaviors often cite a lack of time, overwhelming schedules that do not allow time to cook healthy meals, a lack of sleep, prioritization of outside commitments with family, and unhealthy food culture both at work and home. Being aware of the benefits and potential pitfalls for self and patients can help improve self-care and healthy lifestyle choices (Ross et al., 2019).
Mindfulness has been proven successful among patients and nurses to improve clinical outcomes, even among healthy individuals. Mindfulness is described as “what arises when you pay attention, on purpose, in the present moment, non-judgmentally….and what arises is nothing more than the awareness itself” (Halm, 2017, p. 344). Mindfulness involves developing an open and accepting awareness that is intentional and allows a person to respond to situations rather than to react to them. A study of 38 pediatric intensive care unit nurses notes that stress is reduced significantly at one and two months after incorporating mindfulness into their daily nursing practice. By taking 10 minutes to process or think about an event rather than immediately reacting to the event, these nurses report reduced stress levels and increased resiliency. Mindfulness is reported to improve a nurse's ability to quiet their inner voice and understand their personal needs, as well as those of their patients. Mindfulness is noted in the same study to decrease patient errors and improve patient satisfaction (Helm, 2017).
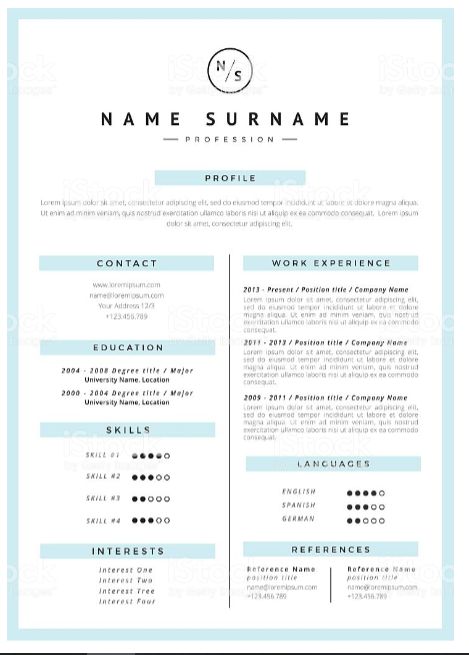
Developing a Brand
Most nurses do not think of themselves as a brand. Branding typically refers to a logo or a type of product, and many can immediately recognize a brand by the color, shape, or location of the product. A nurse's brand is about developing a positive and powerful persona and is very important in today's competitive market. What do others say or think about when that nurse enters the room? Is their brand one of energy and positivity, or are they the one that brings everyone else down? A brand should identify who someone is as a nurse. Do they have a LinkedIn profile? If so, does the picture represent a professional? Does a recruiter, manager, peer, or another individual who may be interested in their work see someone that has taken the time and effort to project professionalism? Just as a resume tells the story of who someone is and how they became a nurse, their brand should reinforce this image. A brand, much like a personality, is how someone conducts themselves, their body language, communication style, and how they make others feel when they are around. Someone may invoke very positive feelings, or very negative ones. Each nurse should examine their brand through the eyes of others to reflect on their image and make changes as necessary. One way to accomplish this is by asking students, colleagues, coworkers, supervisors, and peers for feedback. Obtaining constructive criticism can lead to heightened awareness and aid in professional development. Additionally, brand development can occur through advancing education, obtaining advanced certificates or certifications, as well as through other academically focused improvements. Nurses should remain mindful that their brand is basically everything that represents them in the world, including social media, references, business cards, resume, former employers, and, most importantly, how they show up each day to work (Carlson, 2017).
Conclusion
New graduate nurses have just embarked on a very rewarding journey. While it may be easy to become disillusioned by some aspects of nursing, and it is a challenging career, it is one that offers large quantities of personal, financial, and professional rewards. The first few months or years are often the most challenging as a nurse; it takes both time and intentional effort to develop the knowledge, skills, and attitude needed for success. New graduates should take it one day at a time and strive to maintain a positive outlook. Nurses must stay organized, and avoid being afraid to ask for assistance. A wise new graduate will team up with a mentor that values their nursing experience and wants to share their knowledge with the next generation of caregivers. A new nurse must strive for the confidence to apply for, obtain, and excel at that new job. Finally, as nurses we must show up for each shift with the intention to provide the highest quality, patient-centered care to all that are entrusted to us.
References
The Agency for Healthcare Research and Quality (2017). 20 tips to help prevent medical errors: Patient fact sheet. https://www.ahrq.gov/patients-consumers/care-planning/errors/20tips/index.html
American Nurses Association. (n.d.). Welcome to the profession kit. Retrieved on January 16, 2020 from https://www.nursingworld.org/resources/individual/welcome-to-the-profession/Welcome-to-the-Profession-Kit/
American Nurses Association. (2015). Anatomy of an excellent nursing resume. https://www.nursingworld.org/education-events/career-center/nursing-career-resources/
Carlson, K. (2017). Developing your personal brand. https://www.healthecareers.com/article/career/developing-your-personal-nursing-brand
The Centers for Disease Control and Prevention. (2015). Epidemiology of MDROs: Management of multidrug-resistant organisms in healthcare settings. https://www.cdc.gov/infectioncontrol/guidelines/mdro/epidemiology.html
The Centers for Disease Control and Prevention. (2020). Hand hygiene in healthcare settings. https://www.cdc.gov/handhygiene/index.html
Fowler, S. B., Lind, S. C., Johnson, P. R., & Lewis, J. (2018). Qualitative description of new graduate nurses’ experiences in a nurse residency program. Journal for Nurses in Professional Development, 34(6), 319-324. https://doi.org/10.1097/NND.0000000000000496.
Henriksen, J. N, Nielsen, L. P., Hellebek, A. & Poulsen, B. K. (2017). Medication errors involving anticoagulants: Data from the Danish patient safety database. Pharmacology Research & Perspectives, 5(3), 91-8. https://doi.org/ 10.1002/prp2.307.
Institute for Healthcare Improvement. (2017). Medication reconciliation to prevent adverse drug events. http://www.ihi.org/Topics/ADEsMedicationReconciliation/Pages/default.aspx
Institute for Safe Medication Practices. (2014). How labels, packages, and medicine names can cause confusion and error. https://www.consumermedsafety.org/safety-tips-about-medicine-labels-packages/all-is-not-as-it-seems-how-labels-packages-and-names-can-cause-confusion-and-errors
Institute for Safe Medication Practices. (2016). FDA and ISMP lists of look-alike drug names with recommended tall man letters. https://www.ismp.org/sites/default/files/attachments/2017-11/tallmanletters.pdf
IStock. (2016). Resume template [Image]. https://www.istockphoto.com/vector/resume-template-gm579254928-99624025
The Joint Commission. (2020a). Infection prevention and control. https://www.jointcommission.org/resources/patient-safety-topics/infection-prevention-and-control/
The Joint Commission. (2020b). Sentinel event alert 61: Managing the risks of direct oral anticoagulants. https://www.jointcommission.org/resources/patient-safety-topics/sentinel-event/sentinel-event-alert-newsletters/sentinel-event-alert-61-managing-the-risks-of-direct-oral-anticoagulants/
Jones, J. H. & Treiber, L. A. (2018). Nurses’ rights of medication administration: Including authority with accountability and responsibility. Nursing Forum, 53(3), 299-303. https://doi.org/10.1111/nuf.12252
McKay, D.R. (2019). Professionalism in the workplace. https://www.thebalancecareers.com/professionalism-526248
Merriam-Webster. (n.d.). Professionalism. Retrieved on January 20, 2020 from https://www.merriam-webster.com/dictionary/professionalism
Murray, M., Sundin, D., & Cope, V. (2019). New graduate nurses’ understanding and attitudes about patient safety upon transition to practice. JCN Journal of Clinical Nursing, 28(13-14), 2543-2552.
The Office of Disease Prevention and Health Promotion. (2020). Health care-associated infections. https://health.gov/hcq/prevent-hai.asp
Potter, P. A., Perry, A. G., Stockert, P., & Hall, A. (2017). Fundamentals of nursing (9th ed.). Elsevier.
ResumeOK. (n.d.). New grad nursing resume sample. Retrieved on January 16, 2020 from https://www.resumeok.com/new-grad-nursing-resume-sample/
Ross, A., Touchton-Leonard, K., Perez, A., Wehrlen, L., Kazmi, N. & Gibbons, S. (2019). Factors that influence health-promoting self-care in registered nurses: barriers and facilitators. Advances in Nursing Science, 42(4), 358-373. https://doi.org/10.1097/ANS.0000000000000274
Treiber, L., & Jones, J. (2018). After the medication error: Recent nursing graduates' reflections on adequacy of education. Journal of Nursing Education, 57(5), 275–280. https://doi.org/10.3928/01484834-20180420-04
Trivedi-Mair, D. (2016). Survival guide for new nurses. CreateSpace Independent Publishing.
Walsh, A.L. (2018). Nurse residency programs and the benefits for new graduate nurses. Pediatric Nursing, 44(6), 275-278.
The World Health Organization. (2018). Patient safety: A global health priority. https://www.who.int/patientsafety/en/
The World Health Organization. (2020). Save lives: Clean your hands: WHO’s global annual call to action for health workers. https://www.who.int/infection-prevention/campaigns/clean-hands/en/