The purpose of this activity is to enable the learner to define a basic knowledge of patients with hypertension and diagnostic features.
Course preview
Disclosure Form
At the conclusion of this exercise, the learner will be prepared to:
- Identify the appropriate terms and definitions related to hypertension.
- Consider the impact of hypertension on healthcare in the US and worldwide.
- Formulate an understanding of the pathophysiology of hypertension.
- Identify various risk factors for hypertension methods for prevention.
- Reference appropriate tests and evaluations used to diagnose hypertension.
The leading cause of cardiovascular disease and stroke is hypertension (HTN) and, therefore these are concerns for anyone with elevated blood pressure (BP). HTN is the most common health issue seen in the primary care setting, and if left untreated, stroke, cardiovascular disease, myocardial infarction (MI), kidney failure, and even death can occur (Ignatavicius et al., 2018). The American Heart Association (AHA, 2017) defines HTN as “the silent killer” as people often have no obvious symptoms, yet it is associated with several life-threatening diseases and conditions. This module will explore the current standards of practice and essential patient teaching points for healthcare providers to incorporate into their clinical practice.
Terms and Definitions
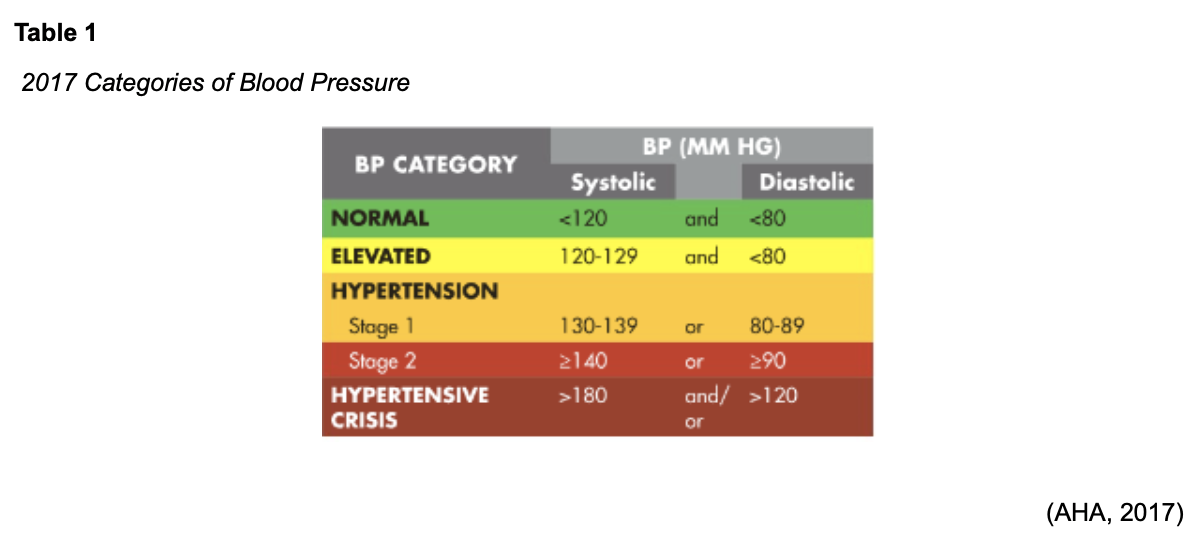
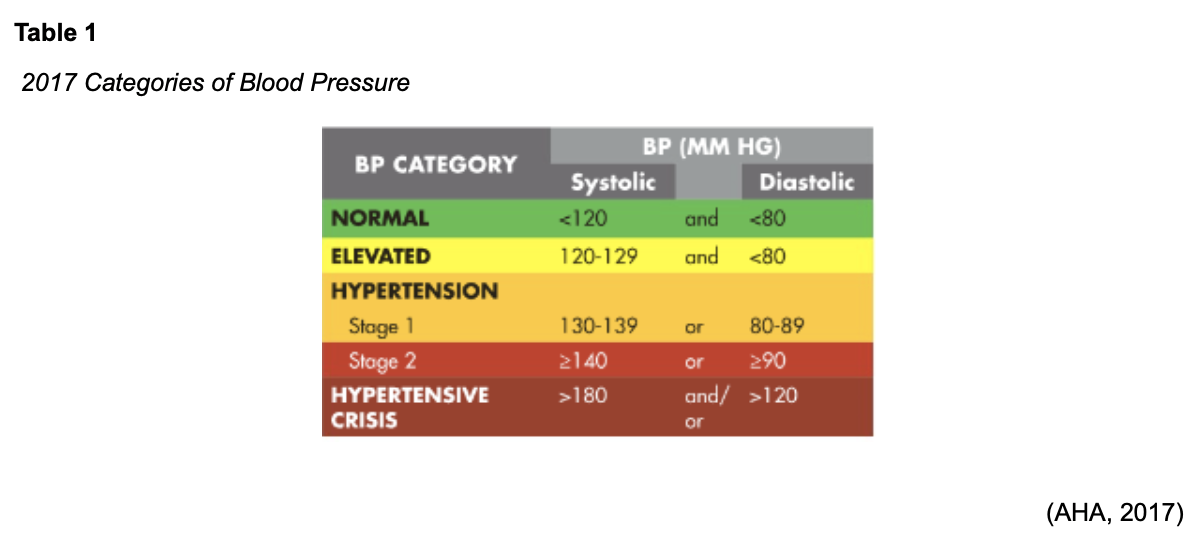
HTN is defined as a systolic BP that is at least 130 mmHg or a diastolic BP of at least 80 mmHg. Further definitions include anyone that is currently taking antihypertensive medications, even with blood pressure readings lower than the above definitions (AHA, 2017).
The most common type of HTN is essential hypertension, which is not caused by a currently existing health problem.
Secondary hypertension is caused by certain disease states or drugs that can increase the BP. A few of these contributing factors include:
- Kidney disease,
- Primary aldosteronism,
- Pheochromocytoma,
- Cushing’s disease
- Coarctation of the aorta,
- Brain tumors,
- Encephalitis,
- Pregnancy,
- Certain drugs, including:
- Estrogens
- Glucocorticoids (i.e., prednisone [Sterapred], dexamethasone[Dexpak])
- Mineralocorticoids (i.e., aldosterone, spironolactone [Aldactone])
- Sympathomimetics (Ignatavicius et al., 2018)
Malignant hypertension or hypertensive crisis refers to a severe form of HTN where the BP elevates rapidly. This condition may present with morning headaches, blurred vision, dyspnea, or symptoms of uremia (the accumulation of urea and nitrogenous waste products in the blood that would normally be eliminated in the urine) (Ignatavicius et al., 2018). These patients are often in their 30s-50s; their systolic BP could be above 200 mmHg. According to the AHA (2017), the defining characteristic is a systolic pressure above 180 mmHg and a diastolic above 120 mmHg. Immediate intervention is required with malignant HTN/hypertensive crisis or it can result in stroke, left ventricular heart failure, or kidney failure (AHA, 2017; Ignatavicius et al., 2018).
Epidemiology
It was noted in 2016 that nearly 1/3 of the US population was impacted by HTN, and nearly 35 million of those affected were uncontrolled. Among the 35 million, as many as 11.5 million were unaware that they had HTN; 7 million recognized they were hypertensive but were not undergoing active treatment for it, and over 16 million were aware they had HTN, were taking treatment, but their HTN was still not properly controlled. This data was based on a diagnostic threshold of a blood pressure above 140/90 mm Hg (Merai et al., 2016). In 2017, the AHA updated their definition of hypertension, which resulted in an updated prevalence of 46% of the adult population. The new categories for BP classification are found in Table 1 (AHA, 2017).
According to a study by Zhang et al. (2017), the national estimate for HTN-related healthcare costs was over $68 billion in 2015, yet this estimate did not include the costs for complications such as stroke or cardiovascular disease. If those aspects are considered, the costs soared to over $130 billion. HTN accounts for more deaths related to atherosclerotic cardiovascular disease (ASCVD) than any other modifiable risk factor (American College of Cardiology [ACC], 2019). While the costs of treating HTN is high, the costs of leaving HTN untreated are higher. The study showed a much higher cost among the elderly (age 65 or older); this could be attributed to their increased risk of hypertension-related health outcomes (i.e., ASCVD, stroke) and an increased proportion of patients requiring antihypertensive medication. Further data identified that women had a higher expenditure on healthcare than men, as they tended to experience more severe HTN-related consequences than men, such as stroke (Zhang et al., 2017).
Demographically, the highest prevalence of HTN is among those 75 or older, female gender, and those who identify as non-Hispanic Blacks. African Americans in the US also seem to develop HTN earlier in life, increasing their risk of death from stroke and heart or kidney disease. Increasing education about this risk can greatly improve patient outcomes among this high-risk population (Ignatavicius et al., 2018). Table 2 shows the distribution of the prevalence of HTN in the US:

Pathophysiology of Hypertension
For an optimal understanding of the pathophysiology of HTN, let's do a quick review of normal BP and how it is maintained. Systemic arterial BP is determined by cardiac output (CO) and the total peripheral vascular resistance (PVR, vessel constriction or dilation). CO is calculated by the stroke volume (SV) multiplied by the heart rate (HR). The autonomic nervous system and circulating hormones, including epinephrine and norepinephrine, control the PVR. Thus, anything that increases the PVR, HR, or SV increases the systemic arterial pressure. By contrast, anything that decreases PVR, HR, or SV also decreases the systemic arterial pressure. However, those factors can also decrease perfusion to the body's tissues. There are mechanisms within the body that stabilize and regulate the systemic arterial pressure to avoid circulatory collapse. Blood pressure is maintained by four major control systems:
- Regulation of body fluid volume,
- Vascular autoregulation,
- The renin-angiotensin-aldosterone system, and
- The arterial baroreceptor system (Ignatavicius et al., 2018).
Systemic arterial pressure is affected by the amount of fluid circulating in the vascular space. If there is an increase in sodium and/or water in the body, BP will rise. If the kidneys are properly functioning, a rise in BP will produce diuresis, and the BP will consequently decline. Various pathologic conditions can change the pressure threshold causing the kidneys to excrete excess sodium and water, thereby altering the BP. Vascular autoregulation is poorly understood, but this process maintains tissue perfusion in the body at a constant rate but is also important in causing HTN. The renin-angiotensin-aldosterone system regulates BP through a complex mechanism of action. The kidneys produce renin, which is an enzyme that acts on angiotensin to produce angiotensin I that is converted to angiotensin II. Angiotensin II causes vasoconstriction of the blood vessels and causes aldosterone to be released. Aldosterone causes the collecting tubes in the kidneys to reabsorb sodium, which causes retention of fluid, further increasing the blood volume and B
...purchase below to continue the course
P. Finally, the arterial baroreceptors are primarily found in the walls of the left ventricle, the aorta, and the carotid sinus. These baroreceptors monitor the level of arterial pressure and work to counteract the rise by vagally mediated cardiac slowing and vasodilation with a decreased sympathetic tone. This action controls the circulation and causes systemic arterial pressure to increase and decrease as needed. The failure of the baroreceptors to control BP in those with HTN is not known (Ignatavicius et al., 2018).
Secondary HTN is caused by disease states or medications that increase BP. Kidney disease is the most common cause of secondary HTN. Renal artery stenosis (RAS) can lead to HTN, which is the narrowing of one or more of the main arteries carrying blood to the kidneys. These patients may benefit from these arteries being dilated through angioplasty and stent placement. Adrenal medulla or cortex dysfunction can cause secondary HTN. Excess aldosterone, cortisol, epinephrine, and norepinephrine can result in adrenal-mediated HTN. Excess aldosterone, caused by primary aldosteronism, can result in HTN and hypokalemia. This usually arises from benign adenomas of the adrenal cortex. Life-threatening HTN can be caused by benign tumors in the adrenal medulla called pheochromocytomas. These tumors secrete excess epinephrine and norepinephrine, or catecholamines. Cushing’s syndrome is an excess of glucocorticoids that can result in HTN and is usually caused by adrenocortical hyperplasia or adrenocortical adenoma. Medications that may cause secondary HTN include estrogens, glucocorticoids, mineralocorticoids, sympathomimetics, cyclosporine, and erythropoietin. Estrogen-containing oral contraceptives are a common cause of secondary HTN in women (Ignatavicius et al., 2018).
The concern with ongoing HTN is damage to vital organs from the hyperplasia (thickening) of the arterioles. With thickened blood vessels, perfusion to tissues is decreased, causing damage to the organs. This can lead to kidney failure, PVD, and MI.
Risk Factors and Methods for Prevention
While essential HTN is not caused by an existing health problem, it can be influenced by risk factors. Risk factors that can contribute to a person’s chance of becoming hypertensive include:
- Kidney disease
- Obstructive sleep apnea (OSA)
- Hyperlipidemia,
- Smoking,
- Excess caffeine or sodium intake,
- Obesity or overweight,
- Lack of physical activity,
- Excess alcohol intake,
- Low magnesium, potassium, or calcium intake
- Excess stress (Ignatavicius et al., 2018)
Many of these factors are modifiable, yet many are relatively fixed, such as age or race. The non-modifiable risk factors include:
- Family history
- African American ethnicity,
- Age- postmenopausal or over 60 years of age,
- Male sex
- Low socioeconomic/educational status (Ignatavicius et al., 2018).
It is important for patients to understand their role in HTN and how their behaviors and actions can change the course of this disease. While many of the risk factors are non-modifiable, many can be avoided. Knowledge is power in changing the outcomes, and educating the person on their risk factors, determining where modifications can take place, and developing a personalized plan of care can provide a foundation toward a healthier BP. Healthcare providers should encourage their patients to monitor their BP at home and use online resources to track their progress, such as the AHA’s Check. Change. Control. Tracker. This resource helps patients self-monitor their BP readings at home to maintain a healthy heart (AHA, 2019).
The US Healthy People 2020 campaign focuses on HTN with several objectives that attempt to decrease cardiovascular mortality and morbidity through prevention. The following objectives focus on HTN and reducing BP:
- HDS-4: Increase the proportion of adults who have had their blood pressure measured within the preceding two years and can state whether their blood pressure was normal or high.
- HDS-5: Reduce the proportion of persons in the population with hypertension.
- HDS-6: Increase the proportion of adults who have had their blood cholesterol checked within the preceding five years.
- HDS-7: Reduce the proportion of adults with high total blood cholesterol levels.
- HDS-8: Reduce the mean total blood cholesterol levels among adults (US Department of Health and Human Services [USHHS], 2014).
Patients should be well educated in their role in reducing their BP. Only a minimal reduction in their numbers can greatly decrease their overall health risks. Figure 1 below shows the benefits of reducing the systolic pressure by only 10 mmHg:

Diagnosis and Testing
The patient evaluation will focus on identifying target organ damage (TOD) and possible secondary causes of HTN to aid in planning an effective treatment regime. The patient history will be considered during this phase of assessment, focusing on potential historical features that may indicate the cause of HTN. See Table 3.

Consideration should be given to patterns of change in BP measurements over time, as this may differentiate primary from secondary HTN. Rises in BP associated with weight gain, change in lifestyle including employment changes, reduction in exercise or physical activity, or advancing age suggest primary HTN. Determine a detailed evaluation of the patient’s dietary habits, physical activity, tobacco or alcohol use, and recommend non-pharmacological interventions as appropriate. Further history should be obtained to rule out or determine potential secondary HTN causes. The most common causes of secondary HTN include:
- OSA
- Kidney disease
- Primary aldosteronism
- Drugs or alcohol-containing caffeine, nicotine, NSAIDs, oral contraceptives, or antacids (AHA, 2017).
Herbals (i.e., ginseng), over-the-counter medications (i.e., pseudoephedrine), and some food substances (i.e., convenience foods high in sodium) can increase BP. Drug-drug interactions can increase the BP or can cause a patient currently taking an antihypertensive to have an increase in their BP. A careful history can identify some of these substances, being certain to elicit information about any changes in over-the-counter drug use, illicit drugs, or herbal products (Whelton et al., 2017).
Healthcare practitioners should determine the patient’s goals and risk tolerance for therapy. Older patients may have multiple or chronic conditions, weakness or frailty and prognosis should be considered. A physical examination should include accurate BP measurements both in the office and in the home. Teaching the patient how to properly self-check their BP is equally important. For accurate BP checks, see Table 4 below.

The use of the appropriately sized cuff is vital to obtaining accurate readings. Table 5 gives directions on the proper cuff size for accurate BP.

For patients who are diagnosed with stage 1 hypertension (SBP 130-139/ DBP 80-90), healthcare providers should determine the patient's 10-year and lifetime risk of ASCVD to develop the most appropriate treatment plan. An ASCVD Risk Calculator is available on the AHA's website which considers the non-modifiable risk factors as well as modifiable risk factors, including cholesterol levels and smoking (AHA, 2013).
The healthcare provider must also consider screening for white-coat HTN or masked HTN. As many as 10% of the population could either be over-treated or under-treated for HTN due to these conditions. White-coat HTN is an increase in the patient’s BP while in the office setting due to fear and anxiety when entering the healthcare environment. Management for white-coat HTN should begin with lifestyle modification for three months. The patient should be counseled to check their BP daily at home, and if it remains above 130/80, continue with lifestyle modifications and initiate antihypertensive drug therapy. If the BP is consistently below 130/80 at home, continue lifestyle modifications with annual BP checks, and diagnose as white coat HTN. Masked HTN is characterized by an SBP between 120-129, and DBP between 75-79 consistently in the office, but higher BP readings elsewhere. Similar to above, masked HTN management should include a three-month trial of lifestyle modification and home BP monitoring. If home BP readings are consistently above 130/80, consider masked HTN and continue with lifestyle modifications and start antihypertensive drug therapy. If the BP is consistently below 130/80 at home, continue with lifestyle modifications with annual BP monitoring and continued home BP monitoring (AHA, 2017). The AHA provides an algorithm on their website for healthcare providers to use in detecting either masked HTN or the white coat HTN (AHA, 2013).
Most primary HTN can be determined through history and physical and home BP monitoring. Initial lab work-up should include cholesterol screening, diabetes screening, potassium and creatinine, and sodium. An EKG should be included in the initial workup, and if the patient has comorbidities such as diabetes or ASCVD, further lab work should be considered (Kaiser Permanente, 2014). However, secondary HTN can require a few more diagnostics. See Table 6 below for diagnostics related to specific conditions.

Uncommon diagnostics that may be considered are plasma thyroid levels for hypo- or hyperthyroidism, 24-hour urine for metanephrines with pheochromocytomas, overnight dexamethasone suppression test for Cushing’s syndrome, echocardiogram for suspected aortic coarctation, serum calcium for suspected primary hyperparathyroidism, or serum growth hormone for suspected acromegaly (Whelton et al., 2017).
For patients that have new-onset or uncontrolled HTN, the algorithm demonstrated in Table 8 can help guide the primary healthcare provider for an appropriate level of care; see the Figure 2 algorithm of secondary or uncontrolled HTN in adults.

The optimal approach to the treatment of HTN is team-based and may require specialty referrals. Physicians, nurses, dieticians, and pharmacists can each contribute their specialty to support the patient in self-care and maintenance of their BP (Whelton et al., 2017).
Special Situations with HTN
HTN during pregnancy can bring unique complications. Not only is the mother’s health compromised, but also the health and wellbeing of the fetus. Hypertension can occur during pregnancy as either chronic HTN, gestational HTN, or preeclampsia. Chronic HTN is defined as elevated BP that is known prior to conception or diagnosed during the first 20 weeks of pregnancy. Gestational HTN is diagnosed after 20 weeks’ gestation without proteinuria. Gestational HTN, sometimes referred to as pregnancy induced hypertension (PIH), can lead to a more serious condition known as preeclampsia. Preeclampsia is a BP above 140/90 with organ damage that occurs after 20 weeks’ gestation. TOD is typically evidenced by proteinuria; thrombocytopenia; elevated BUN, creatinine, or liver transaminases; pulmonary edema; cerebral edema; or visual symptoms. The BP can continue to rise and is considered severe HTN if the SBP rises above 170 mmHg, or DBP rises above 110 mmHg. Studies show that chronic HTN, gestational HTN, or preeclampsia not only have adverse effects on the pregnancy but also are associated with a higher amount of cardiovascular disease later in life. There is a three to six-fold increase in risk for women who had gestational HTN or preeclampsia to develop chronic HTN later in life. There is also a higher risk of type 2 diabetes and hypercholesterolemia later in life. See Table 9 for a HTN screening tool for women related to previous pregnancy risks. This tool was created in 2010 by two cardiologists to determine cardiovascular risks based on a woman's pregnancy history (Gongora, et al., 2018).

For best practices in treatment options, refer to Management of Hypertension at NursingCE.com.
References
American College of Cardiology. (2019). 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease. https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2019/03/07/16/00/2019-acc-aha-guideline-on-primary-prevention-gl-prevention
American Heart Association. (2013). ASCVD risk calculator. https://professional.heart.org/professional/GuidelinesStatements/PreventionGuidelines/UCM_457698_ASCVD-Risk-Calculator.jsp
American Heart Association. (2017). Hypertension guideline toolkit. http://aha-clinical-review.ascendeventmedia.com/books/aha-high-blood-pressure-toolkit/4/
American Heart Association. (2019). Check. change. control. tracker. https://ccctracker.com/
Aronow, W.S. (2015). Blood pressure goals and targets in the elderly. Current Treatment Options in Cardiovascular Medicine, 17(7), 394. https://doi.org/10.1007/s11936-015-0394-x.
Gongora, M.C., Sharma, G., & Yang, E. (2018). Hypertension during pregnancy and after delivery: Management, cardiovascular outcomes and future directions. https://www.acc.org/latest-in-cardiology/articles/2018/09/28/08/08/hypertension-during-pregnancy-and-after-delivery
Ignatavicius, D., Workman, L., & Rebar, C. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care. Elsevier.
Kaiser Permanente. (2014). Hypertension diagnosis and treatment guideline. https://wa.kaiserpermanente.org/static/pdf/public/guidelines/hypertension.pdf
Kaiser Permanente. (2019). Clinical practice guidelines. https://kpcmi.org/files/blood-pressure-clinician-guide-kpcmi.pdf
Merai, R., Siegel, C., Rakotz, M., Basch, P., Wright, J., Wong, B., & Thorpe, P. (2016). CDC grand rounds: A public health approach to detect and control hypertension. Morbidity and Mortality Weekly Report, 65(45), 1261-1264. https://doi.org/10.2307/24859148.
US Department of Health and Human Services (2014). Heart disease and stroke. In Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/heart-disease-and-stroke/objectives
Whelton, P.K., Carey, R.M., Aronow, W.S., Casey, D.E., Colling, K.J., Himmelfarb, C.D., DePalma, S.M., Gidding, S., Jameson, K.A., Jones, D.W., MacLaughlin, E.J., Muntner, P., Ovbiagele, B., Smith, S.C., Spencer, C.C., Stafford, R.S., Taler, S.J., Thomas, R.J., Williams, K.A., Williamson, J.D., & Wright, J.T. (2017). 2017 Clinical practice guideline: ACC/AHA/AAPA/ABC/ACPM/AGS/AphA/ASH/ASPC/MA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. https://doi.org/10.1161/HYP.0000000000000065
Zhang, D., Wang, G., Zhang, P., Fang, J., & Ayala, C. (2017). Medical expenditures associated with hypertension in the US 2000-2013. American Journal of Preventative Medicine, 53(6 Supplement 2), S164-S171. https://doi.org/10.1016/j.amepre.2017.05.014.