About this course:
This course reviews the fundamental aspects of nutritional support for patients with critical illness, including the components of a nutrition assessment, types of enteral and parenteral nutrition access routes, nursing care of nutritional access devices, and clinical considerations to enhance nursing practice and improve patient outcomes.
Course preview
This course reviews the fundamental aspects of nutritional support in patients with critical illness, including the components of a nutritional assessment, types of enteral and parenteral nutrition access routes, nursing care of nutritional access devices, and clinical considerations to enhance nursing practice and improve patient outcomes.
By the completion of this course, the nurse should be able to:
- discuss the vital role of nutrition in patients with critical illness and the components of a nutrition assessment
- provide an overview of enteral nutrition (EN), indications, access routes, benefits, nursing care, and common complications
- provide an overview of parenteral nutrition (PN), indications, access routes, benefits, nursing care, and common complications
- discuss the most common complications associated with short-term and long-term use of EN and PN
- understand ethical issues and considerations related to supporting critically ill patients nutritionally
Nutrition is a crucial aspect of health and is of paramount significance in patients with critical illness, especially in an intensive care unit (ICU). Critical conditions, such as sepsis, trauma, or burns, are typically accompanied by a metabolic stress response generated by the body’s survival mechanisms. Activation of this stress response is often accompanied by a systemic inflammatory response that threatens intestinal integrity and immune function, leading to complications such as infection, multiple organ dysfunction (or failure), prolonged hospitalization, and death. These processes induce complex metabolic and physiologic adaptations in energy production and metabolism, leading to alterations in body composition and heightening malnutrition risk. Advancements in ICU care and life-sustaining support measures have improved survival rates for previously fatal ICU insults. While nutritional support was historically regarded as an adjunctive measure to preserve lean body mass and support a critically ill patient throughout the stress response, this understanding has evolved over the last few decades with advances in science and technology. These innovations have led to a more comprehensive understanding of how adequate nutritional support during the acute phase of illness promotes long-term recovery (Lambell et al., 2020; Seres et al., 2021; van Zanten et al., 2019).
According to the Society of Critical Care Medicine (SCCM) and the American Society for Parenteral and Enteral Nutrition (ASPEN) guidelines (SCCM/ASPEN; McClave et al., 2016), feeding helps “attenuate the metabolic response to stress, prevent oxidative cellular injury, and favorably modulate immune responses” (p. 161). As cited in the guidelines, the early initiation of nutritional therapy—primarily by the enteral route—favorably impacts patient outcomes. Adequate nutritional support initiated during the acute phase of critical illness is a proactive therapeutic strategy that can diminish metabolic deterioration, reduce infection rates, decrease the length of stay in the ICU, and improve clinical outcomes. While nutritional support should begin during the acute phase of illness in the ICU, it often extends beyond hospital discharge through long-term recovery. Healthcare systems are increasingly offering dedicated dietary services (i.e., registered dieticians [RD], clinical nutritionists, and dietary aides) to care for patients with nutritional deficits. Nurses must be equipped with the appropriate skills to care for critically ill patients with nutritional deficiencies and malnutrition requiring nutritional support. Nurses are an integral part of the medical team and collaborate with dietary professionals, providers, and other multidisciplinary team members to ensure the patient’s nutritional needs are met throughout the trajectory of illness (Lambell et al., 2020; McClave et al., 2016; Mueller et al., 2017; van Zantan et al., 2019).
Metabolic Responses in Critical Illness
Metabolism during critical illness is associated with a significant increase in energy expenditure, ranging between 20% and 60% above basal (baseline) energy requirements. These increased energy requirements are associated with amplified carbohydrate and protein metabolism and impaired lipid metabolism. An overview of each metabolic adaptation will be described in this section (McClave et al., 2016; Mueller et al., 2017).
Carbohydrate Metabolism
In critically ill patients, stress hyperglycemia results from alterations in glucose production, decreased glucose uptake by tissues, and insulin resistance (i.e., muscles, fat, and liver don’t respond as well to insulin and can’t easily absorb and metabolize glucose from the blood). Proinflammatory cytokines potentiate the release of catabolic hormones (i.e., glucagon, catecholamines, and cortisol). These hormones stimulate glycogenolysis and gluconeogenesis to mobilize glucose. Through glycogenolysis, glycogen (the primary carbohydrate stored in the liver and muscle) is broken down into glucose to provide immediate energy and maintain blood glucose levels during periods of low glucose (i.e., fasting, hypoglycemia) or increased glucose utilization (i.e., critical illness). Gluconeogenesis involves glucose synthesis via metabolic pathways, primarily occurring in the liver to meet the body’s needs during catabolic stress periods. Moderate or severe infections are associated with a 200% increase in glucose production rate, leading to elevated circulating glucose levels (i.e., hyperglycemia). Once glycogen stores are depleted (often within hours), lipid and protein become the primary sources of energy for survival (McClave et al., 2016; Mueller et al., 2017).
Protein Metabolism
The catabolic response to critical illness is primarily characterized by whole-body protein loss, although both protein metabolism and breakdown occur at accelerated rates. Since humans do not have protein stores, any protein utilized comes at the expense of other tissues that are more labile. Most notably, there is an accelerated breakdown of peripheral muscle proteins, accompanied by decreased amino acid uptake by muscles and increased uptake in the liver. Correspondingly, the synthesis of creatinine, uric acid, and ammonia is accelerated and excreted in increased amounts in the urine. Excess amino acids pool in the skeletal muscles, connective tissues, and gut, leading to a process known as hepatic reprioritization. Increased hepatic uptake of amino acids augments hepatic protein synthesis, fueling gluconeogenesis and producing positive acute-phase proteins (i.e., haptoglobin and c-reactive protein [CRP]). In response, there is a corresponding decline in negative-phase proteins (i.e., albumin and prealbumin). Patients who receive adequate exogenous amino acids to maintain acute-phase protein production are more likely to survive critical illness than those who do not. In unfed, stressed, critically ill patients, up to 250 g of lean body mass is broken down every 24 hours (McClave et al., 2016; Mueller et al., 2017).
Lipid Metabolism
Three catabolic hormones (i.e., epinephrine, norepinephrine, and glucagon) serve a vital role in stimulating lipolysis (the breakdown of stored triglycerides) into glycerol and free fatty acids (FFAs) for energy. However, the intracellular transport of FFAs is impaired, causing FFA to accumulate within the cell. This impairment prompts intracellular acidosis and the accumulation of lactate and pyruvate. Poor FFA utilization leads to decreased aerobic respiration and impairs the cells’ ability to use the Krebs cycle for efficient energy production. It also limits ketogenesis (the formation of keto acids), a vital source of oxidative fuel for organs during starvation. Ultimately, impaired lipid metabolism leads to hyperlipidemia, hyperglycemia, and hyperlactatemia, often affec
...purchase below to continue the course
Pathophysiology of the Digestive System
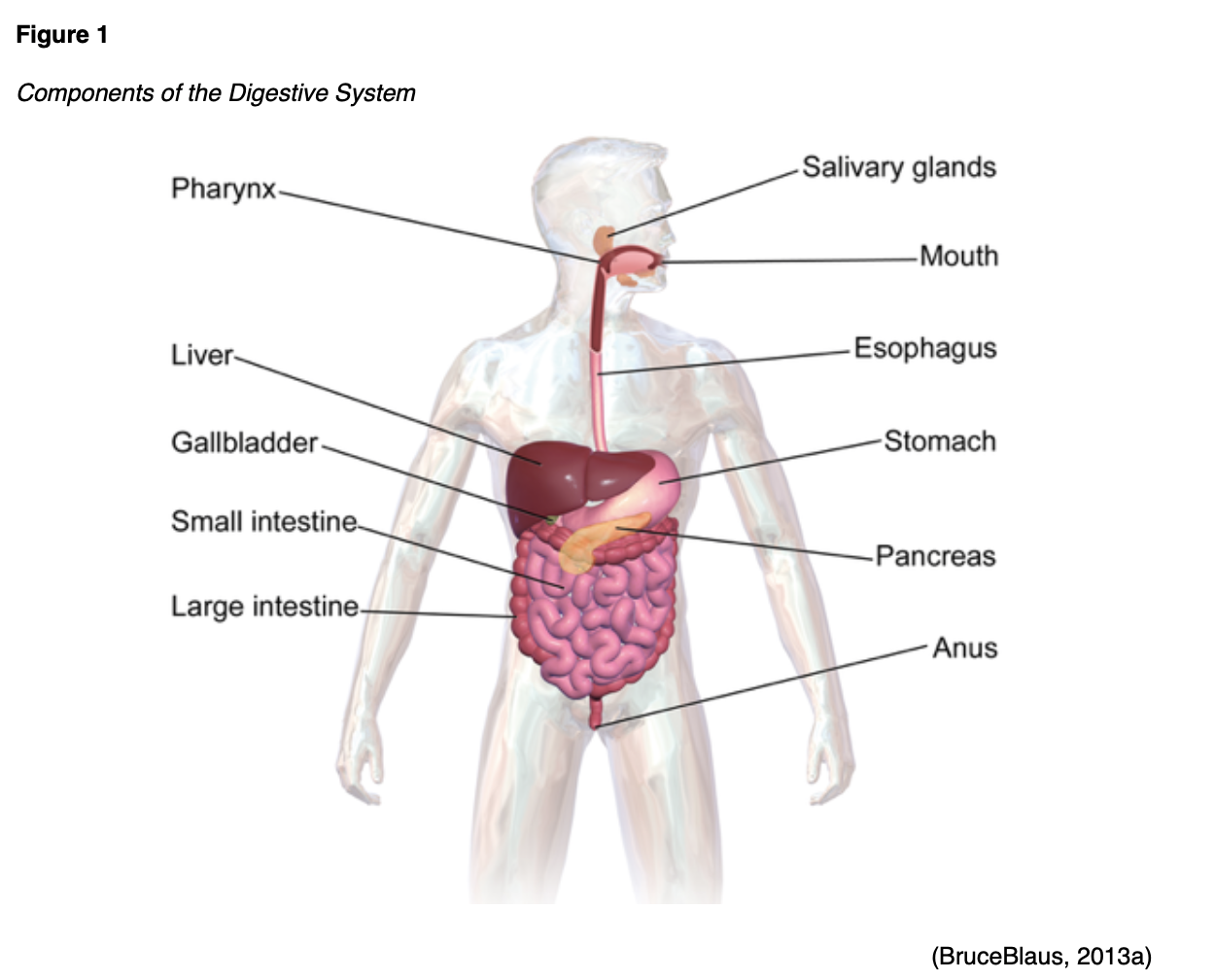
A fundamental understanding of the digestive tract helps HCPs appreciate nutritional support’s core components. The gastrointestinal (GI) tract extends from the mouth to the anus. This organ system is responsible for nutrient intake, digestion, absorption, and excretion (see Figure 1). It carries out various digestive processes to break down food to assimilate nutrients and eliminate waste (McCance & Heuther, 2019).
Food is processed and mixed with salivary amylase enzyme in the mouth before being propelled by the esophagus into the stomach. The stomach is a muscular, J-shaped organ that connects to the esophagus at the gastroesophageal junction. The uppermost part of the stomach—the cardia—contains the cardiac sphincter (see Figure 2). This thin ring of muscles helps prevent acidic stomach contents from backflowing into the esophagus. The fundus is the rounded region that facilitates the stomach’s expansion and contraction in response to food volume. The body (middle), the largest portion of the stomach, is where food is broken down and combined with enzymes, mucus, gastric acids, and other secretions (Lippincott, 2019; McCance & Heuther, 2019).
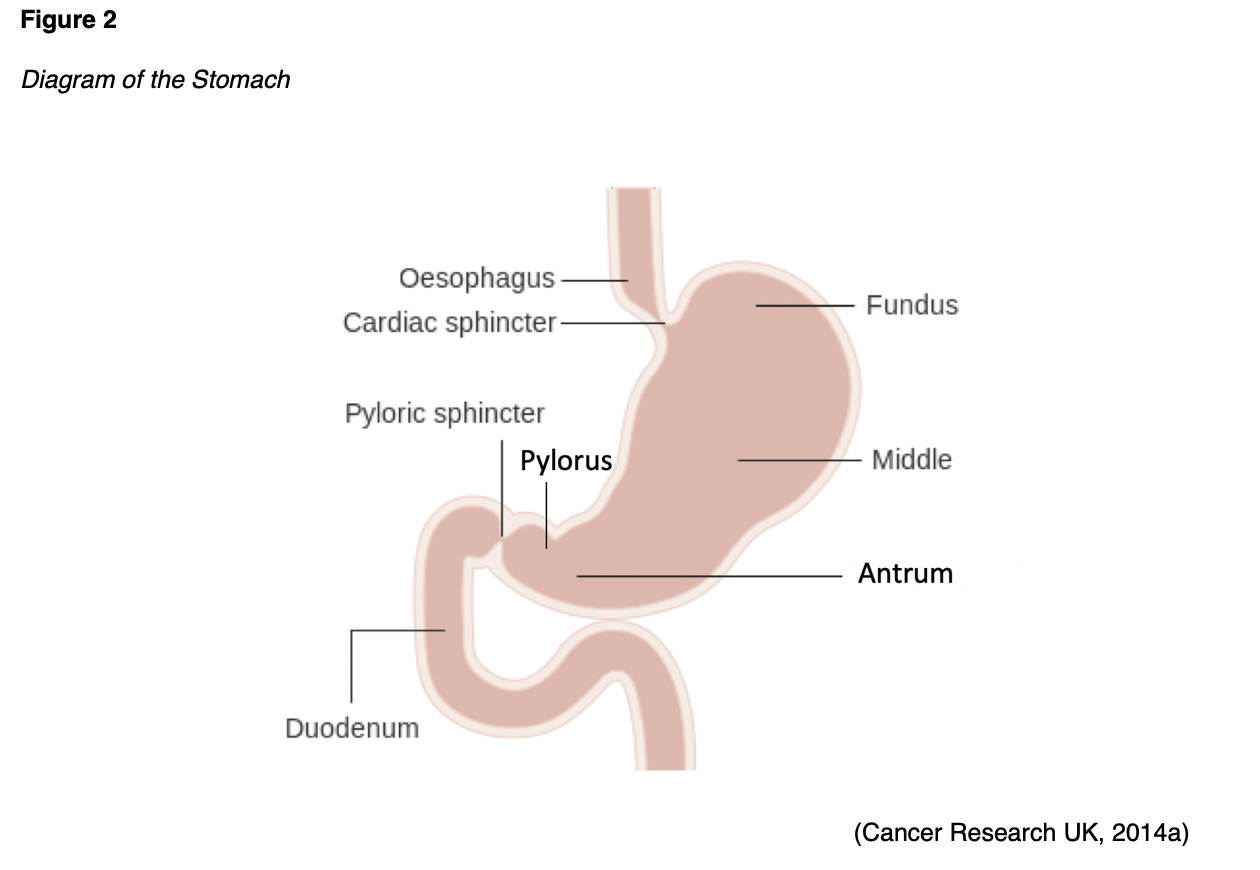
The food is stored in the stomach’s antrum until phasic contractions propel it into the small intestine, where most nutrient absorption occurs. The pylorus is the part of the stomach that connects to the small intestine and includes the pyloric sphincter, a thick ring of muscle that functions as a valve to control the stomach contents as they empty into the duodenum (the first part of the small intestine). Here, biochemicals and enzymes secreted by the pancreas and liver break down the food particles into smaller, absorbable nutrients. The nutrients pass through the small intestine walls into blood vessels and lymphatics before reaching the large intestine, where fluid absorption continues. Liquid waste is transported to the kidneys, where it is excreted from the body in urine. Solid waste travels into the rectum and is eliminated through the anus. The large intestine is the final passageway of undigested food particles and, as shown in Figure 3, is subdivided into four regions: the cecum, colon, rectum, and anus. Its primary function is to complete the absorption of any residual nutrients and water, synthesize specific vitamins, form feces (waste), and eliminate it (McCance & Heuther, 2019).
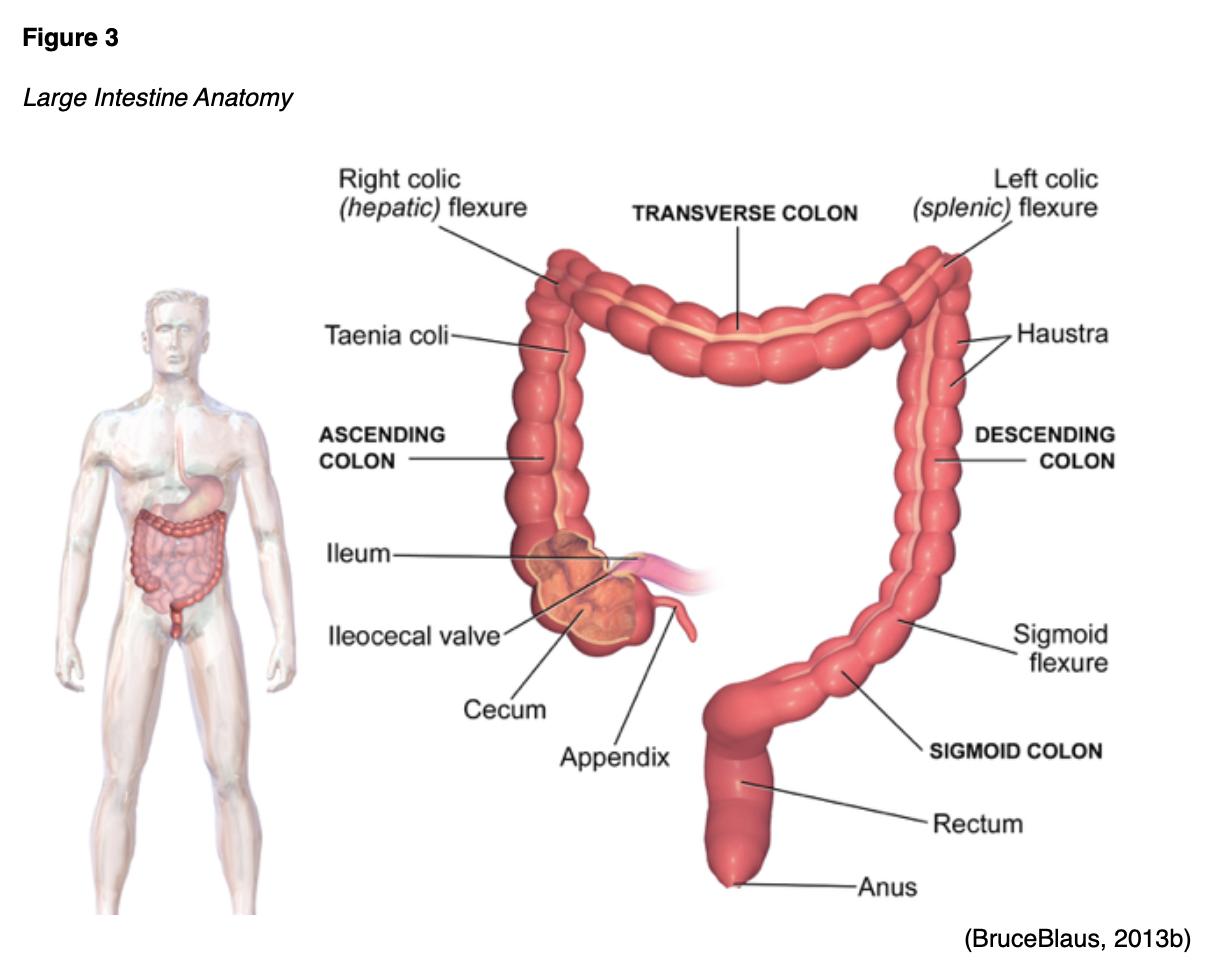
The cecum is the cul-de-sac or small pouch at the beginning of the large intestine. It receives partially digested food (known as chyme) from the small intestine, mixes it with bacteria to continue digestion, and forms feces before transporting it into the colon. The colon is about 5 feet in length and consists of 4 connecting regions: the ascending colon, transverse colon, descending colon, and sigmoid colon. The ascending colon receives feces from the cecum. Then, bacteria digest the waste, and it is transported to the transverse colon. The splenic flexure connects the transverse colon and the descending colon, forming a sharp, right-angle bend on the abdomen’s left side. The descending colon walls absorb water and any remaining nutrients from feces, dehydrating the stool in preparation for elimination. The sigmoid colon is the curved, S-shaped section of the colon that transports and stores the residual fecal matter until it is transported to the rectum. The rectum is the final straight portion of the large intestine; it stores fecal matter until the body is ready to eliminate the waste through defecation. The rectum connects the colon to the anus, the GI tract’s final segment. The anus is a short tube at the end of the rectum that allows feces to pass outside the body during defecation (Innerbody Research, 2017; McCance & Heuther, 2019).
Defining Malnutrition
Defining malnutrition is not straightforward, as definitions vary in their terminology and often lack a set of clear diagnostic criteria. Malnutrition is most simply defined as a physical state of unbalanced nutrition. ASPEN broadly defines malnutrition as “an inadequacy of nutrients to maintain a person’s health that is caused by one or more of the following factors: insufficient intake, impaired absorption, increased nutrient requirements, and altered nutrient transport and utilization” (Mueller et al., 2017, p. 187). The Academy of Nutrition and Dietetics (AND, 2017) compares the patient’s recent nutrient intake with estimated requirements as the primary criterion for defining malnutrition. Specifically, they define malnutrition as “the inadequate intake of nutrients, particularly protein over time, [that] may contribute to, chronic illness, and acute disease or illness and infection” (AND, 2017, p. 3). Regardless of the variable definitions, malnutrition is an independent risk factor that negatively influences a person’s quality of life, autonomy, and clinical outcomes across all illness phases. Malnutrition often develops gradually and is associated with several metabolic and physiologic consequences, including immunosuppression, infection, impaired wound healing, and increased mortality. Patients who are malnourished while in the hospital have an increased risk of complications, longer lengths of stay, higher readmission rates, and increased cost burden (Keller, 2019; Mueller et al., 2017).
Nutritional Support and Screening
Nutritional support refers to the enteral or parenteral provision of calories, protein, vitamins, minerals, electrolytes, and fluids. The body’s primary fuel is generated from the intake of carbohydrates, protein, and lipids. The acquisition and transformation of energy from the environment are essential for life. Energy transformation involves a series of complex biochemical processes through which the body converts energy into the necessary components to power cellular functions and sustain homeostasis. Nutrition screening is the process of identifying patients who may be malnourished or at risk for malnutrition who would benefit from a comprehensive nutrition assessment. Early identification of at-risk patients is crucial for the timely intervention of adequate nutritional support. Screening for the risk of malnutrition in care settings supports early and effective interventions (Mueller et al., 2017; Seres et al., 2021). Evidence-based practice guidelines collectively recommend nutrition screening for all hospitalized patients within 24 hours of hospital admission using a validated screening tool(McClave et al., 2016). Furthermore, nutrition screening and rescreening should occur in response to a clinical concern for nutritional deficits or malnutrition risk. According to The Joint Commission (TJC, 2020), a nutrition screening should be performed if warranted by the patient’s needs or condition. When appropriate for the patient’s condition, screenings must be completed within 24 hours of hospital admission. Under TJC standards, the hospital is permitted to determine who may conduct the screening and complete the documentation based upon the individual’s education, training, and scope of practice (TJC, 2020).
Subjective Global Assessment (SGA)
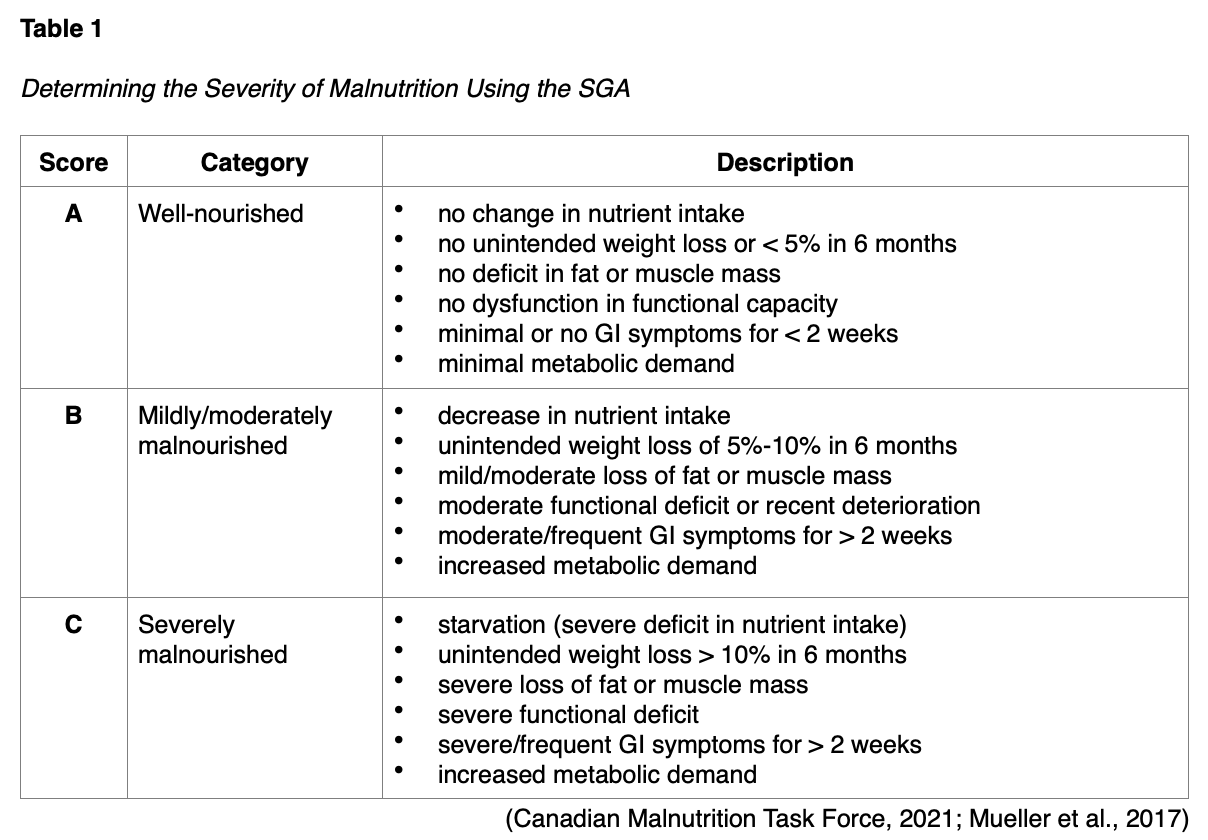
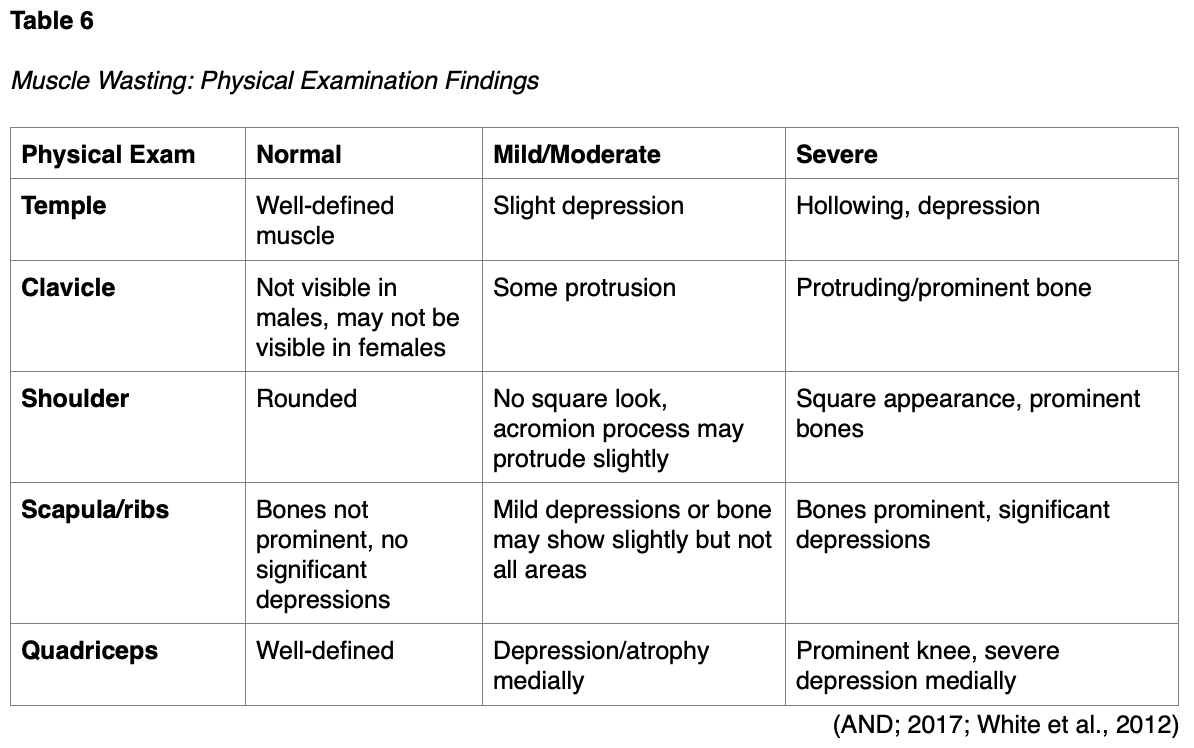
While there are numerous nutrition screening tools, ASPEN endorses the use of the SGA when assessing for nutrition deficits in hospitalized patients. The SGA emerged in 1982 for preoperative patients. Over the last 3 decades, it has become a well-cited and universally recognized tool for diagnosing malnutrition. The Canadian Malnutrition Task Force (2021) designated the SGA as the gold standard for diagnosing malnutrition. The SGA evaluates whether a patient is appropriately nourished (i.e., whether nutrient intake and absorption meet an individual’s requirements) to determine whether nutrition deficits relate to their illness and if nutritional support is warranted. The SGA is a quick, simple, validated, and reliable tool across diverse patient populations. It is highly predictive of the outcome (i.e., provides an accurate diagnosis of malnutrition). This simple bedside tool takes under 10 minutes to complete and can be administered by dieticians, clinicians, and other trained professionals. The SGA includes assessing recent food and fluid intake, weight changes, GI symptoms, other reasons for low intake, and a focused physical evaluation (i.e., evaluating muscle wasting and body fat). It does not require additional laboratory testing and strongly correlates with other subjective and objective measures of nutrition. As demonstrated in Table 1, the SGA classifies patients into three categories: well-nourished, mildly/moderately malnourished, and severely malnourished. Correcting nutritional abnormalities to help normalize muscle and fat stores is a gradual process(Canadian Malnutrition Task Force, 2021; Mueller et al., 2017).
Nutritional Risk Screening (NRS-2002)
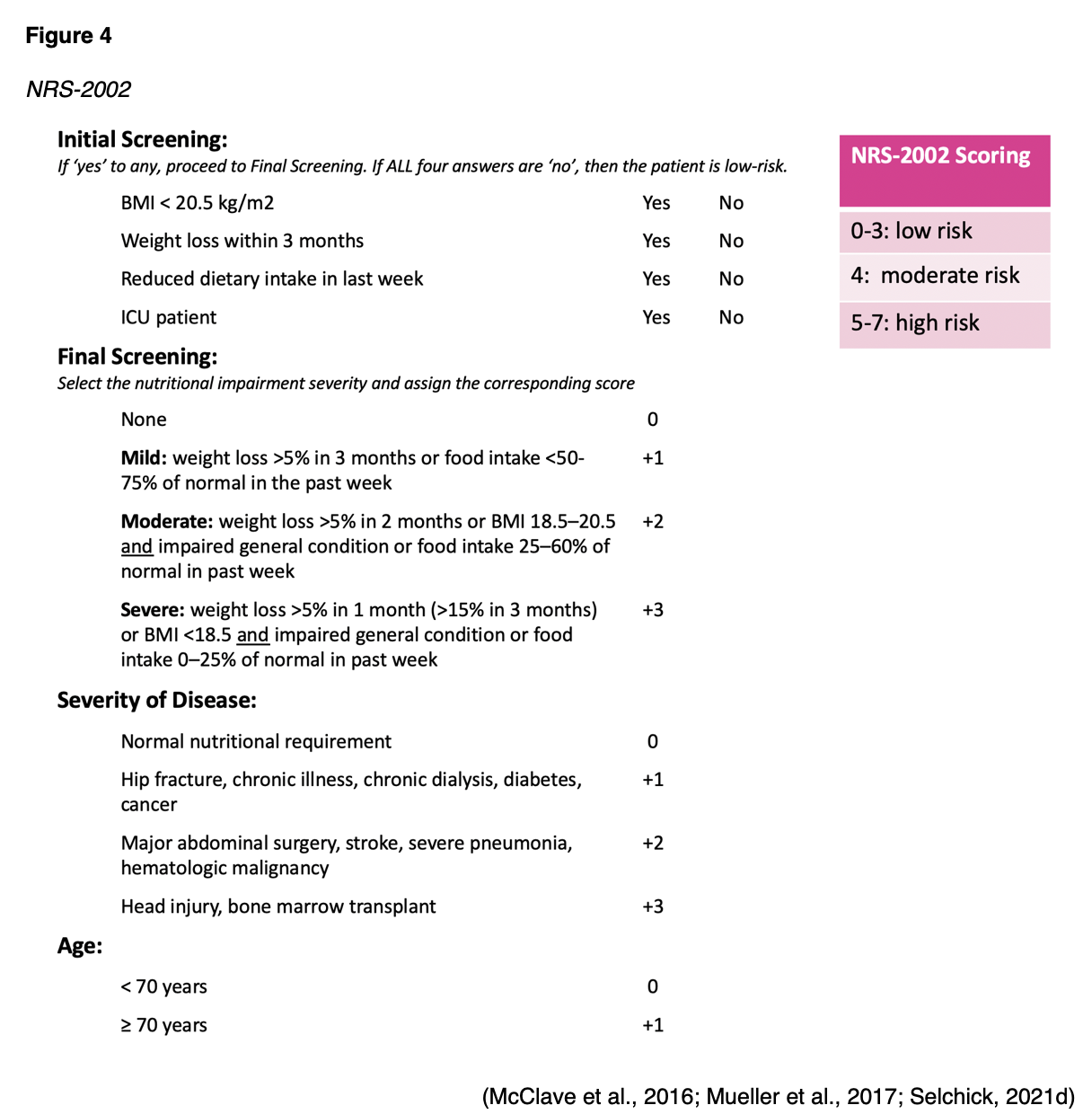
The SCCM/ASPEN guidelines also endorse the NRS-2002 for patients admitted to the ICU. The NRS-2002 is more complex than the SGA, but it helps determine a patient’s nutritional impairment (mild, moderate, or severe) and the severity of the disease. The NRS lists four initial “yes or no” screening questions, as demonstrated in Figure 4. If all four screening questions are answered “no,” then the patient is low risk. Any “yes” responses require the user to proceed to the final screening. The risk level is calculated by tallying the total score. An NRS-2002 score of > 3 defines patients at risk, and those at high risk have a score of ≥ 5 (McClave et al., 2016).
Malnutrition Screening Tool (MST)
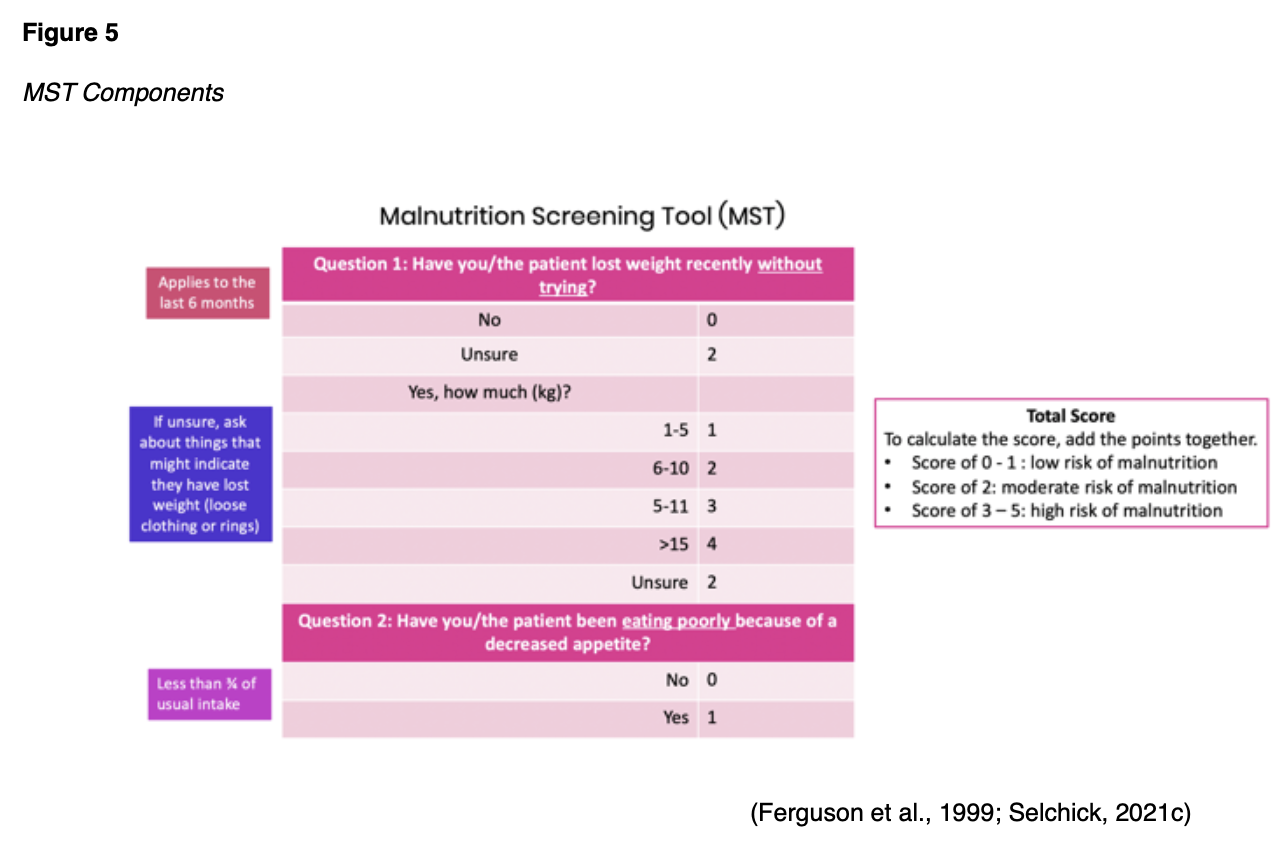
The AND endorses the use of the MST to screen adults for malnutrition regardless of their age, medical history, or setting. Ferguson and colleagues developed the MST in 1999 to detect malnutrition risks and manifestations. Since then, the MST has been validated across acute, long-term, rehabilitation, and ambulatory care settings in several countries. In 2020, the AND released an updated position statement endorsing the use of the MST “to screen all adults for malnutrition, regardless of their age, medical history, or setting” (Skipper et al., 2020, p. 709). The MST is supported by Grade I evidence (i.e., strong evidence with good generalizability). Compared to other screening tools, the MST ranked the highest in its degree of validity and inter-rater reliability in identifying malnutrition risk in adults. The malnutrition screening tool is a 2-question metric that gives a score out of 5 to indicate a patient’s level of malnutrition risk, as outlined in Figure 5 (Mueller et al., 2017; Skipper et al., 2020).
Regardless of the screening tool used, any patient with an identified nutritional risk should subsequently undergo a thorough nutrition assessment to identify and quantify the specifics of their nutritional problems (Mueller et al., 2017).
Comprehensive Nutrition Assessment
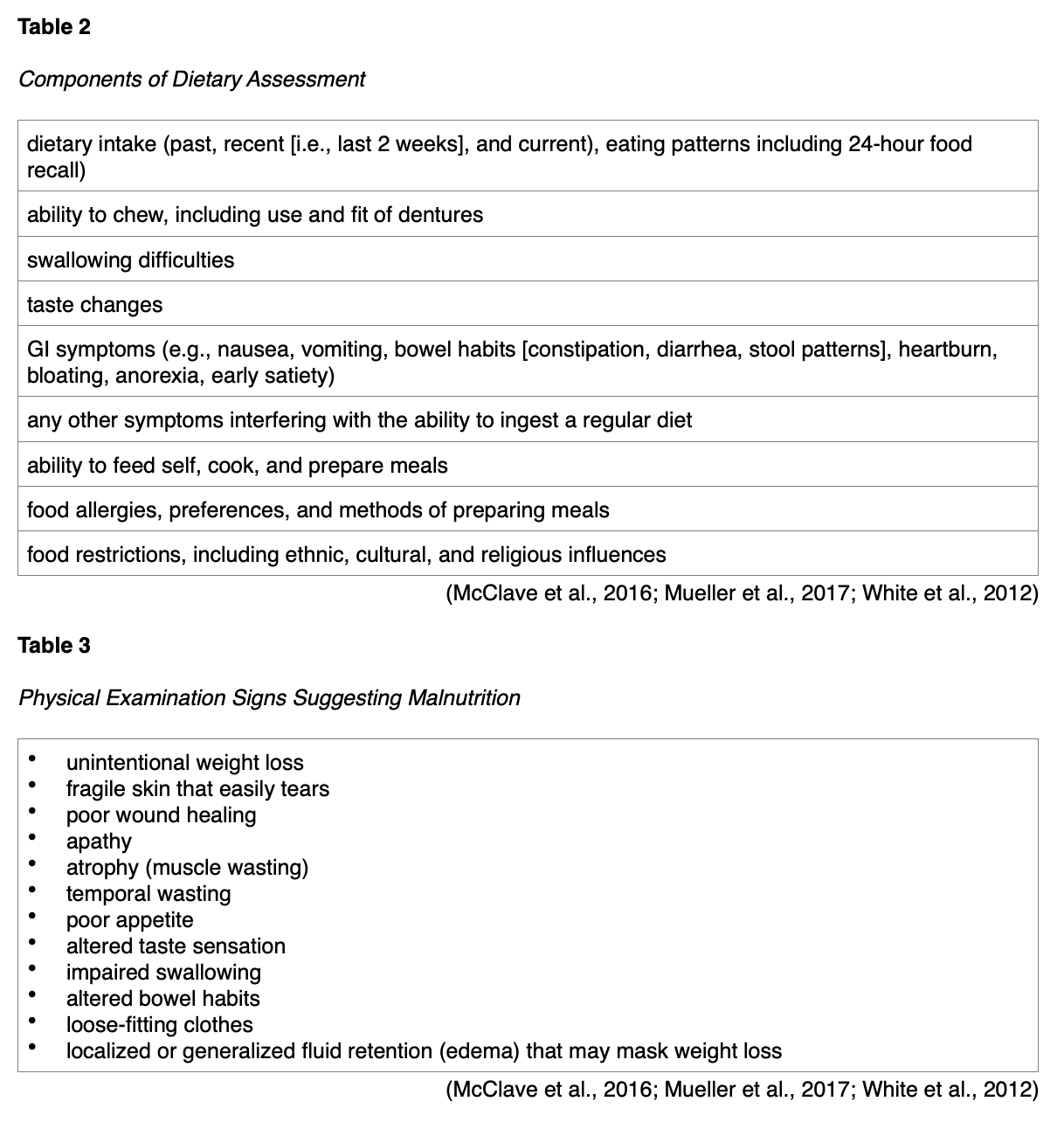
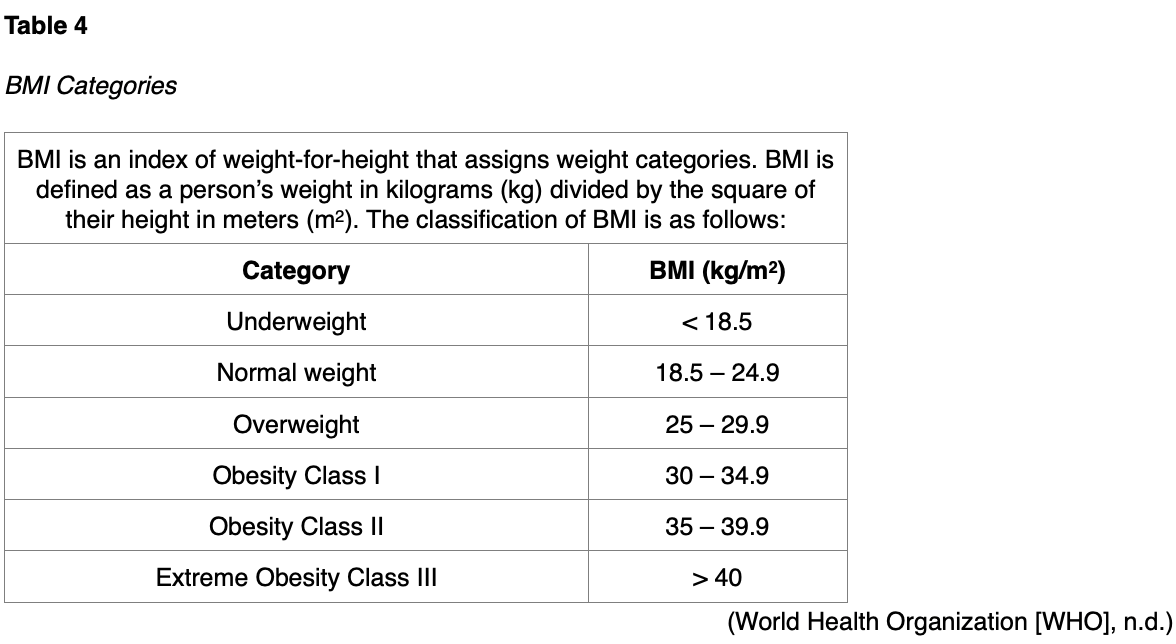
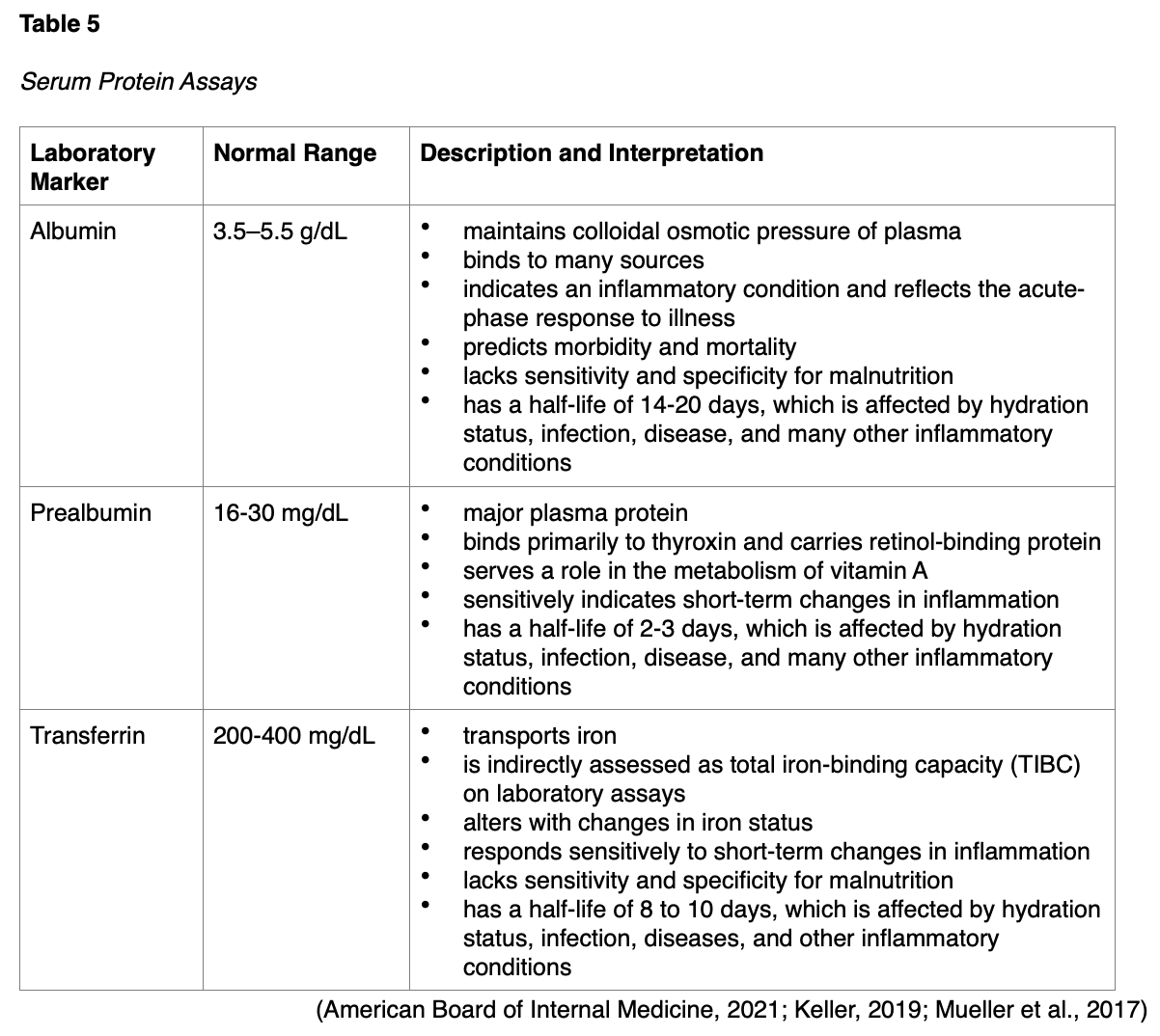
A comprehensive nutrition assessment defines the patient’s nutritional state using a combination of subjective and objective findings. A thorough assessment includes both subjective and objective measures. Subjective measures consist of a complete dietary review (see Table 2), current medical diagnoses, past medical history, medications, lifestyle habits (physical activity level), socioeconomic status/food security, support systems, and substance use (e.g., alcohol consumption, tobacco use, drug abuse). Objective findings are gleaned from a physical examination (see Table 3), anthropometric measurements (e.g., height, usual body weight, current body weight, recent weight change, and body mass index [BMI]; see Table 4), functional and mental health assessment, and biochemical assessment (laboratory values, see Table 5; McClave et al., 2016; Mueller et al., 2017; White et al., 2012).
Laboratory Assays of Malnutrition
Serum proteins such as albumin, prealbumin, and transferrin have traditionally been used as laboratory markers of nutritional status. The prealbumin level is preferred over albumin due to its shorter half-life, reflecting more rapid changes in nutritional status (Keller, 2019). Table 5 provides an overview of these serum proteins and their clinical interpretations. However, despite their widespread presence in the nutritional support literature, AND (2017) and the SCCM/ASPEN guidelines (McClave et al., 2016) collectively advise against using these laboratory assays in the management of critically ill patients. In critical care settings, these serum protein markers reflect the acute-phase response to illness driven by increased vascular permeability and hepatic protein reprioritization. They do not accurately represent nutrition status in the ICU setting and offer little value for clinical decision-making for these patients. Recent evidence has demonstrated that serum levels of these proteins do not change in response to nutrient intake changes, thereby rendering them an inaccurate assessment of malnutrition status (AND, 2017; McClave et al., 2016; Mueller et al., 2017).
Assess for Malnutrition
While the definitions of malnutrition are widely accepted, they lack clearly defined diagnostic criteria. In 2009, ASPEN and the AND recognized the need to standardize the diagnostic approach to malnutrition in adults and coordinating their efforts. Acknowledging that no single parameter is definitive for adult malnutrition, they generated specific criteria to diagnose malnutrition. As cited in their updated consensus statement (White et al., 2012), a diagnosis of non-severe (moderate) or severe malnutrition requires at least 2 of the following six characteristics:
- insufficient energy intake
- weight loss
- loss of muscle mass
- loss of subcutaneous fat
- localized or generalized edema
- diminished functional status as measured by handgrip strength (White et al., 2012)
More recently, in an attempt to establish a global consensus on diagnosing malnutrition, newer criteria were introduced in 2018 from the Global Leadership Initiative on Malnutrition (GLIM). According to the GLIM criteria, at least one phenotypic criterion and one etiologic criterion should be present to diagnose malnutrition:
- Phenotype criteria: Non-volitional weight loss, low BMI, and reduced muscle mass
- Etiologic criteria: Reduced food intake or absorption/assimilation, and inflammation or disease burden (Jensen et al., 2019)
Enteral Nutrition vs. Parenteral Nutrition
EN incorporates any feeding method that uses the GI tract to deliver all or part of a person’s caloric requirements. EN may include a regular oral diet, the use of liquid supplements, or delivery of part or all of the daily requirements via a catheter, stoma, or tube (i.e., tube feeding). EN offers several benefits such as decreased cost, maintenance of gut integrity and gut-associated lymphoid tissue (which is vital for immune support), and the prevention of bacterial translocation and reduced infections. The beneficial effects of EN compared with PN are well-cited across several randomized controlled trials of critically ill patients, with reduced infectious complications associated with sepsis, pneumonia, and intra-abdominal abscess. While EN is the preferred route of nutritional support for critically ill patients, it can be supplemented with PN if nutritional needs are not fully met. However, some patients have complex medical issues that preclude the safe and effective use of the GI tract. PN is appropriate for patients with impaired GI function since it bypasses the normal processes of ingestion, digestion, and absorption, delivering all calories and nutrients through a vein. PN is defined as the intravenous (IV) infusion of nutritional needs for patients who cannot take appropriate amounts of food enterally. The core components of EN and PN will be described throughout this learning activity (McClave et al., 2016; Mueller et al., 2017; Seres et al., 2021).
Overview of EN
EN is the preferred route of nutritional therapy since it helps maintain the integrity of the GI tract. EN is only indicated for patients with a functioning GI tract, with sufficient length and absorptive capabilities. Most critically ill patients cannot eat anything, and they rely entirely on nutritional support to satisfy their caloric needs. In the ICU, EN has two primary purposes: to meet the patient’s nutrient requirements (particularly the significantly increased protein requirement) and to infuse nutrients into the intestines at a rate that upholds the normal intestinal barrier and immunological functions. Protein appears to be the most critical nutrient for healing wounds, supporting immune function, and maintaining lean body mass. Since protein requirements are proportionately higher than energy requirements and thus are not easily met in critical illness settings, the role of early intervention with EN is vital. SCCM/ASPEN guidelines indicate that EN should commence within 24 to 48 hours following the onset of critical illness and admission to the ICU, or as soon as possible after a critically ill patient has been fluid-resuscitated and stabilized (Hoffer et al., 2018; McClave et al., 2016; Mueller et al., 2017).
EN Indications
The most common indications for EN include major trauma, burns, sepsis, intubation, and neurologic conditions that impair swallowing ability (e.g., stroke, amyotrophic lateral sclerosis, Parkinson’s disease). Patients with head and neck cancers often require EN due to obstructing tumors, as it allows them to sustain calories during multimodal and complex treatment modalities (AND, 2020; Mueller et al., 2017).
EN Contraindications
Contraindications to EN therapy include any condition in which use of the GI tract is not feasible. Contraindications to EN include the following:
- nonfunctional GI tract (e.g., severe malabsorptive conditions)
- inaccessible GI tract (e.g., upper GI obstruction precluding feeding tube placement)
- severe short bowel syndrome (< 100 cm of remaining small bowel in the absence of the colon or 50-70 cm of remaining small bowel in the presence of the colon)
- severe GI bleed or GI hemorrhage
- distal high-output GI fistula (an abnormal opening in the GI tract that leaks fluids, secretions, and nutrients)
- paralytic ileus
- peritonitis
- intestinal ischemia
- inoperable mechanical bowel obstruction (AND, 2020; Mueller et al., 2017)
EN Access Devices
There are several options for EN access devices. When selecting the anatomical site for enteral access, HCPs much consider several factors, including but not limited to the following:
- expected duration of therapy (i.e., short-term or long-term)
- underlying medical diagnoses, including gastric and small bowel function
- desired feeding location (i.e., stomach or small intestine)
- nutrient administration mode (i.e., bolus or continuous feeding)
- patient or family preference
- institution-specific resources and expertise of clinicians available for placement (Mueller et al., 2017)
Access devices for short-term enteral access are recommended if the estimated need for feeding will be under 4 weeks. Figure 6 depicts the most common types of enteral access devices. Short-term enteral access is most commonly obtained by nasoenteric or nasogastric tubes inserted through the nose (or less commonly the mouth) into the stomach, duodenum, or jejunum. Long-term enteral access is recommended when enteral feedings may be required for more than 4 to 6 weeks. Long-term EN access is typically obtained through the creation of percutaneous gastric or intestinal access. Examples of long-term access devices include gastrostomy and jejunostomy tubes (Mueller et al., 2017).
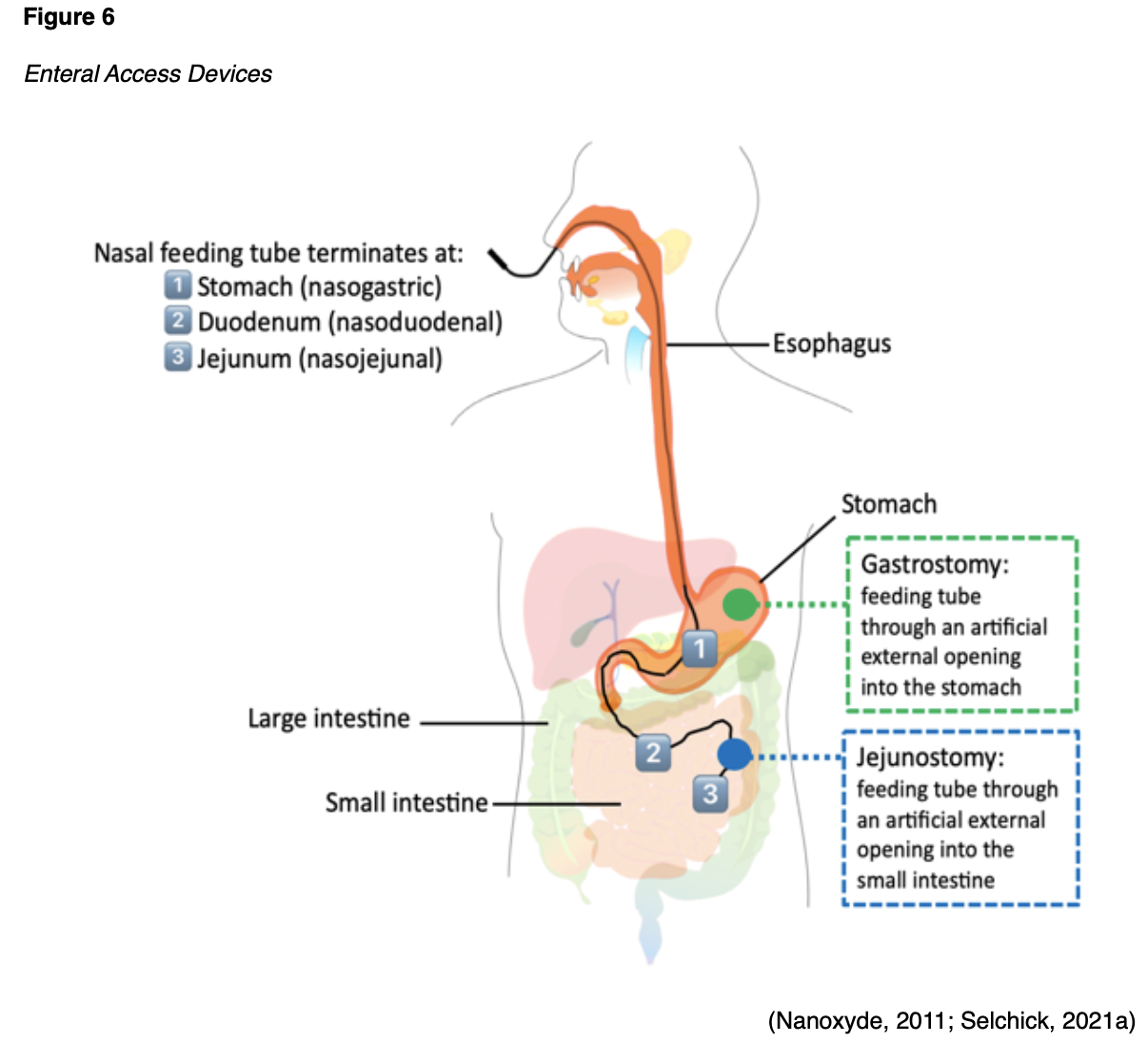
When deciding between gastric or intestinal access in critically ill patients, consideration must be given to the patient’s risk of aspiration or altered gastric emptying. Small bowel (i.e., intestine) feeding decreases the risk of pulmonary aspiration. Small-bore, flexible tubes are typically preferred for awake and alert patients since they can reduce discomfort. These tubes are also beneficial for patients receiving anticoagulation, as they are associated with a reduced risk of upper GI bleeding. An overview of each enteral access device will be described in the next section (Mueller et al., 2017; Seres et al., 2021).
Feeding Tube Sizes
Feeding tubes come in a wide array of sizes, lengths, and diameters. Flow through the tube and susceptibility to clogging are based on its inner diameter. The external diameter measurement is reported for all feeding tube sizes in French units (Fr). According to the Fr scale, 1 Fr is equal to one-third of a millimeter (mm). The diameter (D) around the feeding tube is determined by dividing the Fr by 3, as outlined in the example at the bottom of Figure 7 (Pash, 2018).

Nasoenteric Tubes
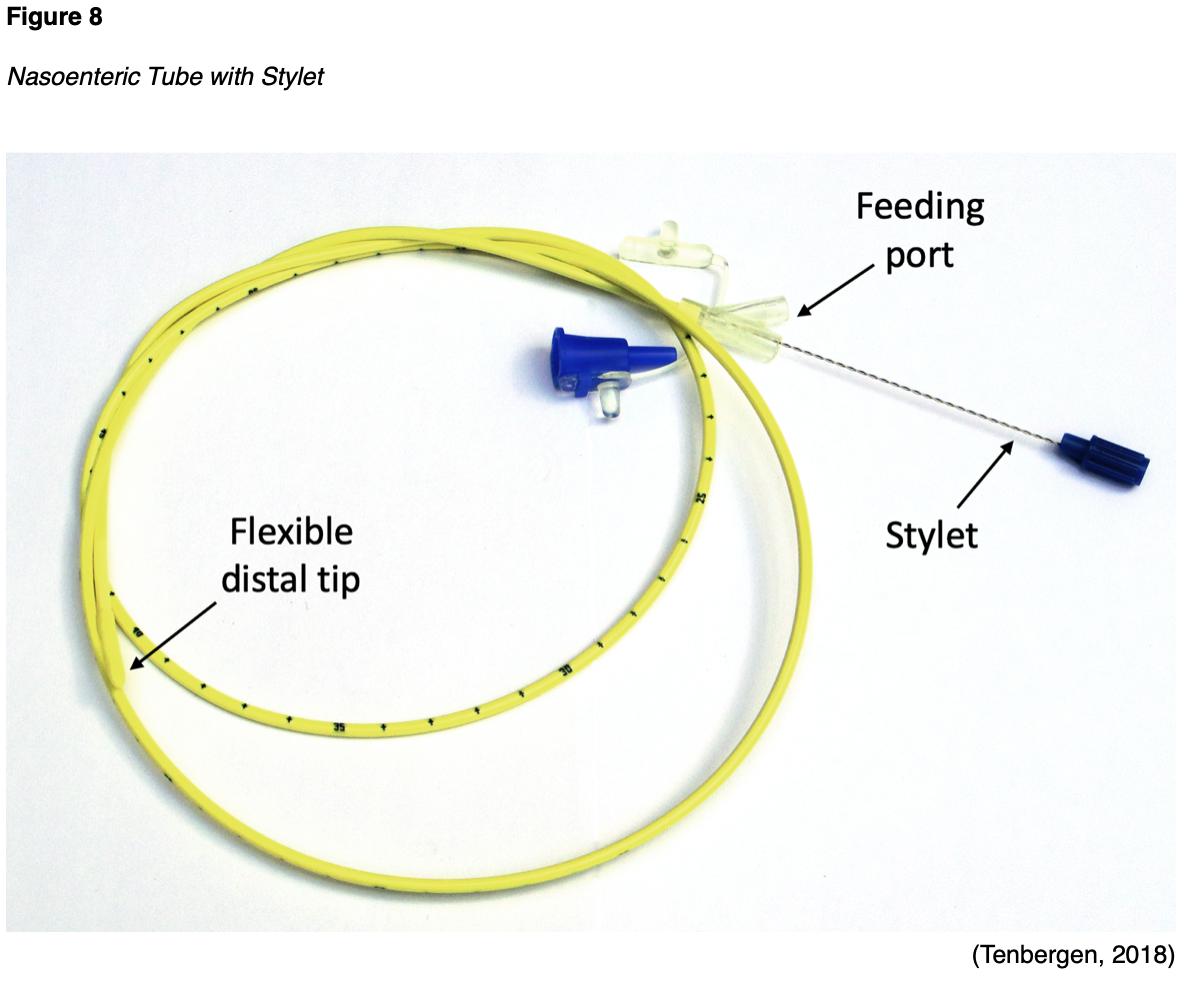
Nasoenteric tubes are ideal for short-term EN and are typically made of polyurethane, offering a larger inner tube diameter for each size. Among adults, the most commonly placed nasoenteric tube size in adults is 16 Fr. However, they can clog easily because they are narrow, as demonstrated in Figure 8. Since these tubes are floppy and flexible, stylets typically accompany them to offer structure and guidance during placement. The stylet is shorter than the tube’s length and has a flexible distal tip to prevent accidental perforation of the GI wall. Nasoenteric tubes may have either a port for feeding or two ports in a “Y” configuration, allowing for both feeding and medication administration (Hodin et al., 2021; Seres et al., 2021).
There are three major types of nasoenteric tubes, which are named according to their termination site, as shown in Figure 6:
- nasogastric (NG) tube: is inserted into the nasal passage, passes through the throat and esophagus, and terminates in the stomach
- nasoduodenal (ND) tube: is inserted into the nasal passage, passes through the throat, esophagus, and stomach, and terminates in the first portion of the small intestine (duodenum)
- nasojejunal (NJ) tube: is inserted into the nasal passage, passes through the throat, esophagus, stomach, and extends to the second portion of the small intestine (jejunum; Hodin et al., 2021; Seres et al., 2021)
ND and NJ tubes are referred to as post-pyloric feeding tubes because they bypass the stomach. All nasoenteric tubes can be placed non-surgically and are temporary. Placement may be performed at a patient’s bedside, with the assistance of specialized tracking devices, or under endoscopy or fluoroscopic guidance by an interventional radiologist. Patients who are awake and alert should be positioned in an upright position, whereas unconscious patients should be placed in a supine position. The tube is placed into a nare, and the advancement of the tip is aided by having the patient swallow. Once the tube is in its proper position, it should be taped securely to the nose, but the tube should not push against the nares due to the risk for pressure ulcers, heightened in unconscious patients who cannot communicate discomfort. The tube can be fixed to the patient’s gown with a safety pin (Hodin et al., 2021; Seres et al., 2021).
Nasoenteric tubes should never be used until confirmation of their proper position is obtained. Placement should be documented with a plain radiograph (x-ray) of the lower chest or upper abdomen. X-ray has been the gold standard for verifying placement for decades; however, more recent studies have suggested that radiographic confirmation is unnecessary when the insertion is guided by imaging technology such as fluoroscopy. Auscultation, pH testing, and capnography are considered unreliable methods and cannot confirm the placement of nasoenteric tubes (Mueller et al., 2017). Once the position of the tube is established, the stylet is removed. The stylet should never be replaced or reinserted because it can lead to GI perforation (Hodin et al., 2021).
After the appropriate nasoenteric tube has been placed and its position verified, the head of the patient’s bed should be raised to at least 30 degrees to reduce the risk of regurgitation and aspiration. Ensuring the patency of nasoenteric tubes is essential since they are easily prone to clogging. Most guidelines recommend that the tubes be irrigated with water every 4 to 8 hours and flushed immediately after each intermittent feeding bolus. While many patients may experience oropharyngeal discomfort, it typically resolves within 24 to 48 hours of placement. Local anesthetic spray may be applied to the oropharynx to alleviate pain and symptoms associated with the gag reflex from a tube’s presence. However, any new or sudden onset of gagging, emesis, or respiratory issues should raise clinical suspicion for possible migration of the tube. In this case, the feeding should be withheld, and the tube positioning should be reevaluated with an x-ray. All nasoenteric tubes impair the esophageal sphincter’s normal functioning, thereby heightening the risk of reflux of gastric content into the esophagus, leading to esophagitis, esophageal stricture, GI bleeding, or pulmonary aspiration. Improperly securing the tube or placing too large a tube in an unconscious patient can lead to pressure ulcers and skin necrosis. Although rare, nasoenteric tubes can perforate the GI tract organs and the respiratory system. These risks are highest in patients who have undergone prior esophageal or gastric surgeries. Removing nasoenteric tubes is typically straightforward and rapid. However, if any resistance is met upon attempted removal, the procedure should be aborted, as the tube should never be forced. In these instances, radiographs should be obtained to identify any underlying pathology that may be causing resistance. Although uncommon, the tube can become knotted or coiled and may require endoscopy or fluoroscopy for safe removal (Hodin et al., 2021; Mueller et al., 2017; Seres et al., 2021).
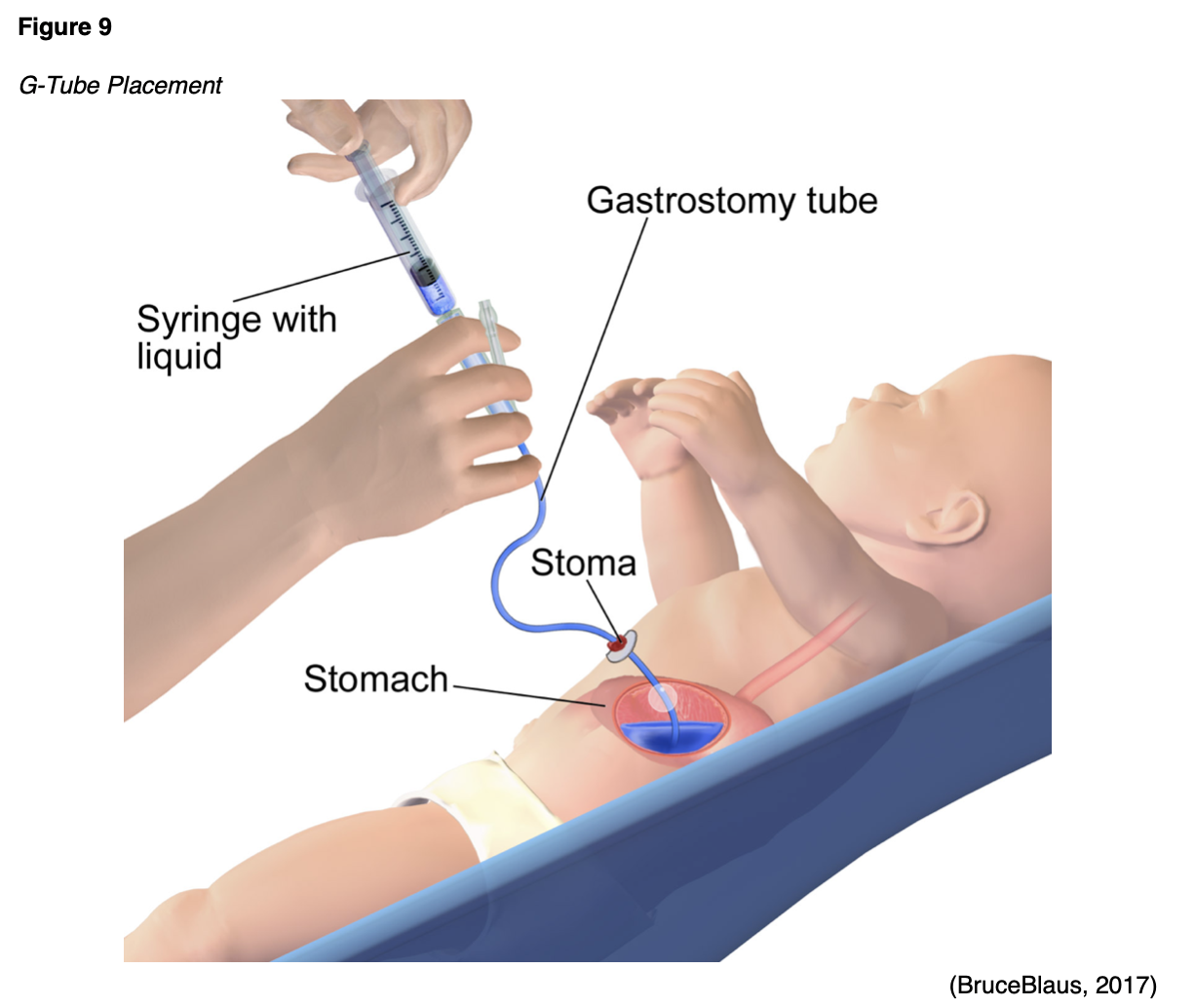
Gastrostomy Tubes (G-Tubes)
Long-term EN requires permanent access to the stomach or small bowel. G-tubes are the most common long-term EN devices and are placed when long-term access (more than 4 weeks) is required. They are inserted directly into the stomach (gastric region) via an abdominal incision (stoma) and can remain in place for months to years. G-tubes offer the most significant benefits for critically ill patients suffering from dysphagic stroke, brain injury, neurodegenerative diseases, or obstruction due to malignancy. Multiple studies have cited G-tubes as a superior feeding method compared to nasoenteric tubes in patients at high risk for aspiration. G-tubes can be placed by endoscopic, fluoroscopic, or surgical techniques. Endoscopic and fluoroscopic procedures are preferred over surgical intervention because they are associated with lower morbidity and cost. Typically, a gastroenterologist or surgeon selects the most optimal device based on the patient’s needs, anatomy, and institutional resources. Most G-tubes are made of silicone for longevity and enhanced flexibility. Percutaneous endoscopic gastrostomy (PEG) tubes are the most common type of long-term EN access. However, no established guidelines currently indicate which ICU patients should receive a PEG over other G-tubes. G-tubes are preferred as the first-line long-term EN access over small bowel tubes (i.e., jejunostomy tubes). Table 7 provides an overview of the most common types of G-tubes (DeLegge et al., 2021; Feeding Tube Awareness Foundation, n.d.).
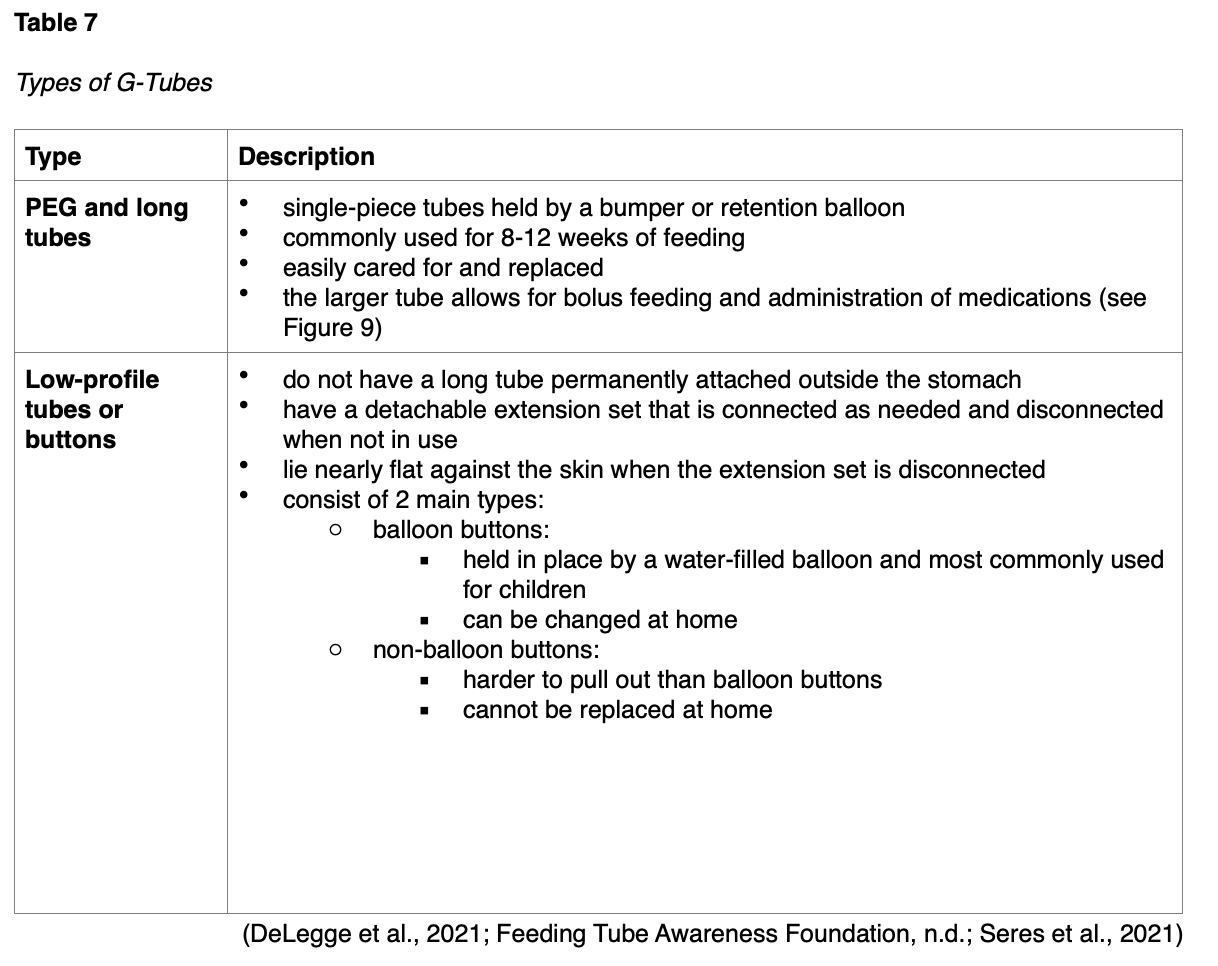
Gastrojejunal (GJ) Tubes
When the stomach needs to be bypassed for feeding, a GJ tube may be considered. However, it is rare for a GJ tube to be placed initially, as most patients start with a G-tube. Like G-tubes, GJ-tubes are inserted into the stomach; however, a thin, long tube is threaded into the jejunum inside the stomach. Most GJ tubes have separate ports to access both the stomach (G-port) and the small intestine (J-port). Less commonly, transjejunal (TJ) tubes can offer access to the small intestine. GJ tubes are available both as buttons or long tubes, as described in Table 7 (Feeding Tube Awareness Foundation, n.d.; Seres et al., 2021).
Pre-Procedural Considerations
While each feeding tube has unique insertion procedures, antibiotic prophylaxis is typically indicated to prevent infection. Furthermore, specific anticoagulation therapy principles need to be considered and are outlined below (DeLegge et al., 2021; Mueller et al., 2017; Seres et al., 2021).
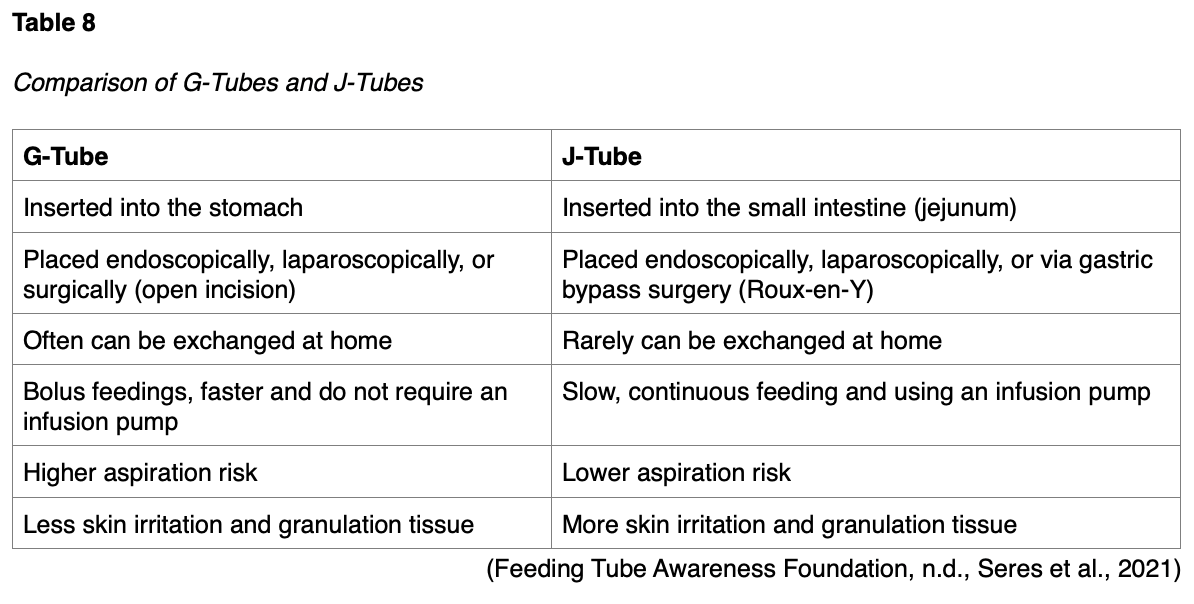
Jejunostomy Tubes (J-Tubes)
According to the SCCM/ASPEN guidelines, feeding tubes in the lower GI tract should be reserved for critically ill patients with a high risk of aspiration or those who have shown intolerance to gastric EN. J-tubes are ideal for cases of delayed gastric emptying, chronic vomiting, a history of regurgitation, or severe acute pancreatitis. J-tubes are also appropriate for those with a risk of aspiration to decrease the risk of aspiration pneumonia. Jejunal feeds minimize pancreatic exocrine secretions by bypassing the upper GI tract, serving as a core aspect of treating pancreatitis. J-tubes decrease the risk of food and fluids passing into the lungs, allowing for early postoperative feeding. These permanent feeding tubes are indicated for long-term EN access and are placed directly into the jejunum. J-tubes are less commonly used than G-tubes and are typically reserved for patients who cannot tolerate G-tubes due to intestinal obstruction or anatomical issues. Several guidelines recommend considering a J-tube when EN access is needed permanently (i.e., lifelong). The jejunum has a smaller width than the stomach, and it does not have an expandable region to accommodate increased volumes. Therefore, J-tubes require slow, continuous feeding via a feeding pump. Feeding through a J-tube typically takes 16 to 24 hours per day. Similar to G-tubes, J-tubes include long tubes and buttons. There are three primary modalities for J-tube placement (McClave et al., 2016; Mueller et al., 2017; Seres et al., 2021):
- Percutaneous endoscopic jejunostomy (PEJ): the tube is directly placed into the jejunum using an endoscope.
- Laparoscopic or open surgery: the J-tube is placed directly into the small intestine through an incision in the abdominal wall.
- Gastric bypass procedure or Roux-en-Y: in this more complex procedure, a small “limb” is constructed in a portion of the jejunum and attached to the abdominal wall. The J-tube is placed in the newly created limb. While this option is more complicated, it allows for a more stable tract and easier tube changes, which can be done at home.
J-tubes are more likely to leak than G-tubes, causing more irritation and granulation tissue development. Table 8 provides a comparison of G-tubes and J-tubes (Feeding Tube Awareness Foundation, n.d., Seres et al., 2021).
EN Feeding and Formulas
EN formulas contain several types of nutrients and water in varying quantities to meet the patient’s needs. Amino acids, probiotics, trace minerals, and fiber may be added to the formulas as needed. While there are numerous commercially prepared formulas, this learning activity focuses on caring for patients who require nutritional support and not formula selection. Nutrition therapy is typically started at a slower initial rate and increased as tolerated toward the patient’s nutritional goals. Current guidelines recommend starting EN as soon as a critically ill patient has been resuscitated, stabilized, and provided with enteral access. EN is then advanced over the following days toward the patient’s nutritional goal. Feeding through a PEG or G-tube tends to mimic oral intake, as the stomach expands when full. Studies have demonstrated a significantly lower frequency of regurgitation with PEG compared to NG feeding tubes. Furthermore, critically ill patients are more likely to achieve nutritional goals when a PEG is used over nasoenteric access. According to the SCCM/ASPEN guidelines, bowel sounds and evidence of bowel function (i.e., passing flatus or stool) are not required for initiation of enteral feedings. The literature supports EN’s feasibility and safety within a patient’s initial 36–48 hours of admission to the ICU regardless of the extent of audible bowel sounds. EN does not have to be held for gastric residual volumes under 400 mL in the absence of other signs of GI intolerance, such as nausea, vomiting, abdominal pain, or distention (McClave et al., 2016; Mueller et al., 2017; Seres et al., 2021).
EN Complications and Management
EN’s most common complications include aspiration of regurgitated formula, fluid and electrolyte abnormalities, hyperglycemia, diarrhea, abdominal pain, and failure to achieve nutritional goals. ICU patients with delayed gastric emptying, an impaired gag reflex, and ineffective coughing have a high risk of aspiration pneumonia. Aspiration is common among mechanically ventilated patients. According to the AND Evidence Analysis Library (AND EAL, 2012), if a critically ill patient is mechanically ventilated and requires EN, a J-tube is recommended over a G-tube. Research studies evaluating ventilator-associated pneumonia (VAP) as a primary outcome suggest that small bowel EN instead of gastric EN reduces VAP. However, other benefits—reducing the number of days on mechanical ventilation, costs of care, and mortality—have not been demonstrated. Continuous EN is tolerated better than bolus feeding and is associated with a lower risk of aspiration (AND EAL, 2012). VAP is mainly caused by the aspiration of infectious pathogens in the oral cavity and throat. Essential measures to prevent VAP include elevating the bed’s head, performing regular oral hygiene, and irrigation practices (AND, 2020; McClave et al., 2016; Mueller et al., 2017).
Abnormally high gastric residual volumes, abdominal discomfort, distention, diarrhea, and nausea create distress for patients, increase the nursing workload, and offset nutritional goals. These issues can be minimized by ensuring normal fluid and electrolyte balance, maintaining strict glucose control, and responding rapidly to GI distress (e.g., administering anti-emetics). EN formulas typically contain standard amounts of fluid, electrolytes, minerals, and nutrients, but they are not designed to manage abnormal fluid volume or electrolyte and mineral requirements, which vary considerably and can change rapidly due to underlying disease processes. Additionally, most formulas are high in glucose. In the context of underlying metabolic adaptations to critical illness (i.e., impaired carbohydrate metabolism and hyperglycemia), blood glucose must be monitored regularly. Measures must be taken to maintain homeostasis as indicated (e.g., intravenous fluid, electrolyte replacement, insulin therapy). Diarrhea is a common complication when bowel function is compromised by illness or medication (e.g., antibiotics). For critically ill patients, infectious and inflammatory etiologies must be ruled out first. EN-associated diarrhea may be controlled by supplementing feeds with fiber-containing formula or by adding antidiarrheal agents. Histamine-2 (H2) blockers or PPIs can also help reduce the net volume of fluid transported to the colon. Finally, all feeding tubes are prone to clogging and obstruction. Inadequate tube flushing, dense formulas, and the introduction of inadequately dissolved solid medications are common causes of clogged tubes (AND, 2020; McClave et al., 2016; Mueller et al., 2017).
The SCCM/ASPEN guidelines advise that EN be withheld from hemodynamically unstable patients until they are fully resuscitated or stabilized. Specifically, EN should be withheld in the following clinical scenarios:
- hypotensive patients (mean arterial blood pressure < 50 mm Hg)
- patients who require the initiation of catecholamine agents (i.e., norepinephrine, phenylephrine, epinephrine, or dopamine)
- patients for whom escalating doses of medications are needed to maintain hemodynamic stability (McClave et al., 2016)
The initiation or re-initiation of EN may be considered with caution in patients undergoing withdrawal of vasopressor support. EN should be withheld in patients on vasopressor therapy with signs or symptoms of intolerance (i.e., abdominal distention, decreased passage of stool or flatus, increased aspiration) due to the potential for gastric ischemia (McClave et al., 2016).
Overview of PN
The successful infusion of hypertonic PN in the 1960s signified a significant advancement in providing nutrition to patients with nonfunctioning GI tracts. PN is typically reserved for patients with contraindications to EN therapy or those whose nutritional goals are unmet by EN. PN is costlier and more resource-intensive, and it carries a higher risk for infection and other complications than EN. In addition to the contraindications to EN listed above, indications for PN therapy include the following:
- inability to meet estimated energy needs after 7 to 10 days of EN
- severe short bowel syndrome
- paralytic ileus
- mesenteric ischemia
- small bowel obstruction
- GI fistula preventing the placement and use of tube feeding distal to the fistula (AND, 2020; Mueller et al., 2017)
Routes of Administration
The components of parenteral feeding formulas determine whether the feeding can be administered via peripheral infusion (i.e., peripheral parenteral nutrition [PPN]) or require a central venous catheter (i.e., central parenteral nutrition [CPN]). PN formulas are hypertonic to body fluids and, if administered inappropriately, may result in complications such as venous thrombosis, thrombophlebitis, or extravasation. The osmolarity of parenteral feeding depends on the quantity of dextrose, amino acids, and electrolyte concentration. PPN is controversial and rarely used. It is reserved for patients who require PN for under 2 weeks and is rarely administered to the critically ill and ICU population. Furthermore, patients receiving PPN must have excellent peripheral venous access and tolerate large volumes of fluid (e.g., 2.5 to 3 L/day). Therefore, this section focuses on CPN, which is also referred to as total parenteral nutrition (TPN). CPN can fulfill a patient’s entire nutrient needs via a reasonable fluid volume tailored to their energy and protein requirements. CPN is administered directly into a patient’s central venous blood supply via a central venous catheter (McClave et al., 2016; Mueller et al., 2017).
Central Venous Catheter (CVC)
A CVC or central line is a long-term indwelling device that can remain in place for extended periods (i.e., months to years). This thin, flexible tube is inserted via puncture directly through the skin into a large vein, often in the neck, chest, arm, or groin. The catheter is threaded through the vein until the tip reaches a large vein near the heart. The area where the central line leaves the skin is called the exit site. CVCs used for CPN include the following types: peripherally inserted central catheter (PICC), tunneled IV catheter, non-tunneled IV catheter, and implanted port. Standards of practice published by the Infusion Nurses Society (INS; Gorski et al., 2016) favor PICCs and tunneled IV catheters for CPN. CVCs may be inserted by specially trained and certified healthcare professionals (e.g., RNs, APRNs, or physicians). Regardless of the device selected, CVC insertion is a sterile procedure and requires formal training, as successful placement depends highly on the technique of the individual inserting the line. Some devices require surgical placement in the operating room or interventional radiology department under fluoroscopy guidance, whereas others allow for bedside insertion. The following section will provide a brief overview of the 4 CVC devices used for CPN (Centers for Disease Control and Prevention [CDC], 2019; Gorski et al., 2016; Leib et al., 2020; McDiarmid et al., 2017).
PICC
A PICC is indicated for long-term access, and the dwell time varies from weeks to months but can be more than a year if proper care is provided. A PICC is inserted in the basilic, cephalic brachial, or median cubital veins in the upper arm; the basilic vein is generally preferred. The line is threaded through the vein so that the catheter tip is located in the lower segment of the superior vena cava (SVC), as demonstrated in Figure 8. A chest x-ray is required to confirm the catheter tip’s placement in the lower SVC before the PICC line is used. Catheter sizes range from 2 Fr to 6 Fr, and the catheter length is approximately 40-60 cm long but is cut to the patient’s size before insertion (Gorski et al., 2016; Leib et al., 2020; Paje et al., 2019).
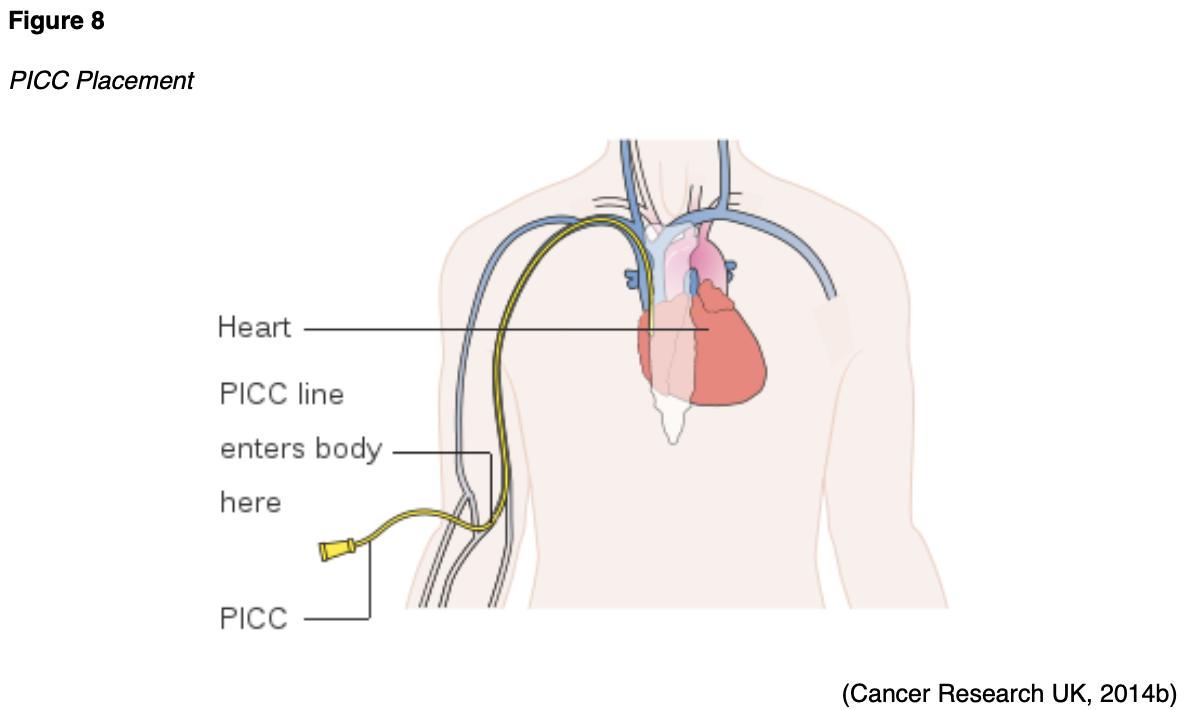
PICC lines are available as single-, double-, and triple-lumen catheters; however, multi-lumen PICC lines have twice the complication rate as single-lumen catheters (Gorski et al., 2016; Paje et al., 2019). INS guidelines recommend that the fewest lumens necessary for the prescribed therapy should be inserted. Furthermore, larger-gauge PICCs are associated with an increased risk of venous thrombosis, so using the smallest lumen possible is also advised (Gorski et al., 2016; Leib et al., 2020).
Tunneled CVC
A tunneled CVC is used when CPN is indicated for several months or longer. It is surgically implanted in a central vein in the neck or chest and then subcutaneously tunneled to an exit site in the chest wall. As demonstrated in Figure 9, the vein entry site is located on the upper chest, and the exit site is located between the third or fourth intercostal space. The tip of the catheter rests in the SVC. A Dacron cuff device is positioned within the tunneled portion of the catheter, approximately 2 to 3 cm from the exit site. Tissue grows around the cuff, thereby creating a mechanical barrier against microorganisms and anchoring the catheter in place. The separation between where the catheter enters the vein and exits the skin is intended to reduce infection risk by preventing organisms from reaching the bloodstream (Leib et al., 2020; McCance & Heuther, 2019).
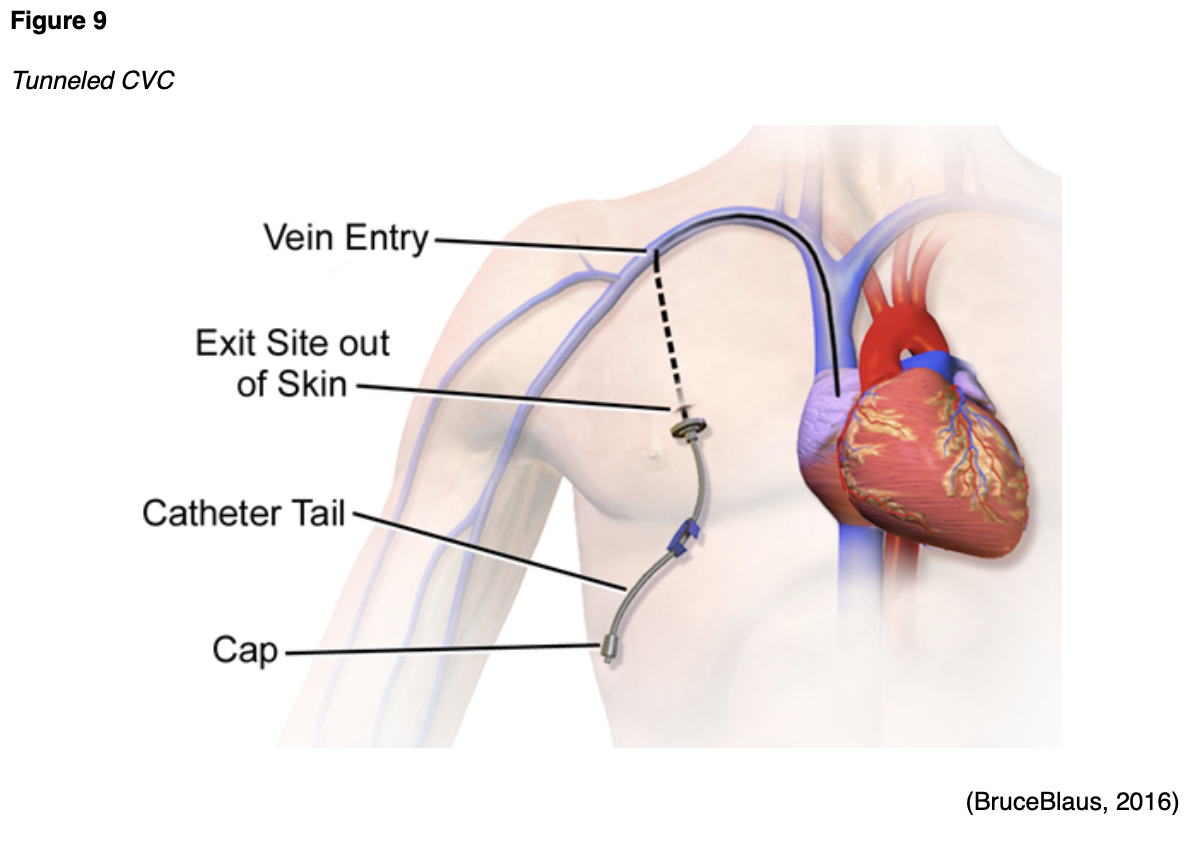
Before using a tunneled CVC, placement of the catheter must be confirmed by an x-ray. The nurse must have an active order from a licensed provider stating that the line may be used, although this policy varies by organization. The INS guidelines recommend placing an initial sterile dressing on the site following insertion. The dressing should be changed 24 hours following line insertion and every 7 days after that, or when visibly dirty, wet, or soiled. Once the insertion site has completely healed over, usually about 21 days following insertion, the line may be left open to the air and uncovered. The nurse must assess the catheter’s patency before use by aspirating for blood return, which should be brisk. Patency should be checked before administering CPN, and the line should also flush without resistance. Syringes smaller than 10 mL should never be used with any type of tunneled CVC (Gorski et al., 2016).
Non-Tunneled CVCs
Non-tunneled CVCs are small-bore catheters inserted percutaneously through the subclavian vein of the upper chest or the jugular veins, as shown in Figure 10. With these devices, the catheter exits the skin in the vicinity of the venous cannulation site (Gorski et al., 2016; Tse & Schick, 2020).
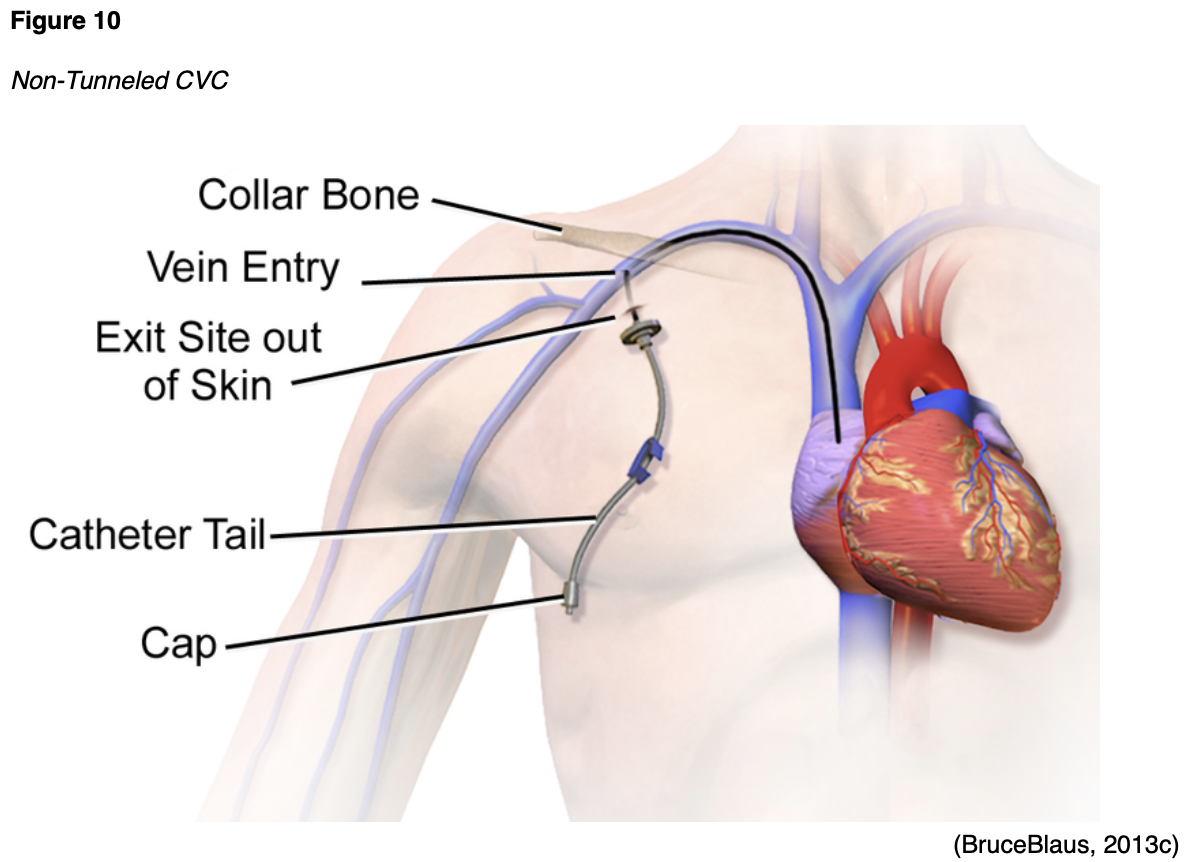
Non-tunneled CVCs are usually 15 to 25 cm in length and can have single, double, triple, or quadruple lumen(s). The catheter is sutured in place to prevent the catheter from migrating or being inadvertently dislodged. The tip of the catheter resides in the SVC, and a chest x-ray must confirm proper placement before use. Non-tunneled CVCs are intended for short-term and temporary use, usually 5 to 10 days (Tse & Schick, 2020).
Implanted Port
An implanted port is surgically placed into a subcutaneous pocket of the anterior chest wall, about an inch beneath the collarbone. The insertion of the device is performed under local anesthesia by a surgeon or interventional radiologist. The port consists of a thin, flexible catheter that is attached to a reservoir. The catheter is threaded into the central venous system via the subclavian, jugular, or femoral vein, and the tip of the catheter resides within the SVC. The reservoir can be made of plastic, stainless steel, or titanium and is about the size of a quarter. It is covered with a self-sealing silicone septum designed to withstand multiple needle punctures (Lippincott, 2019).
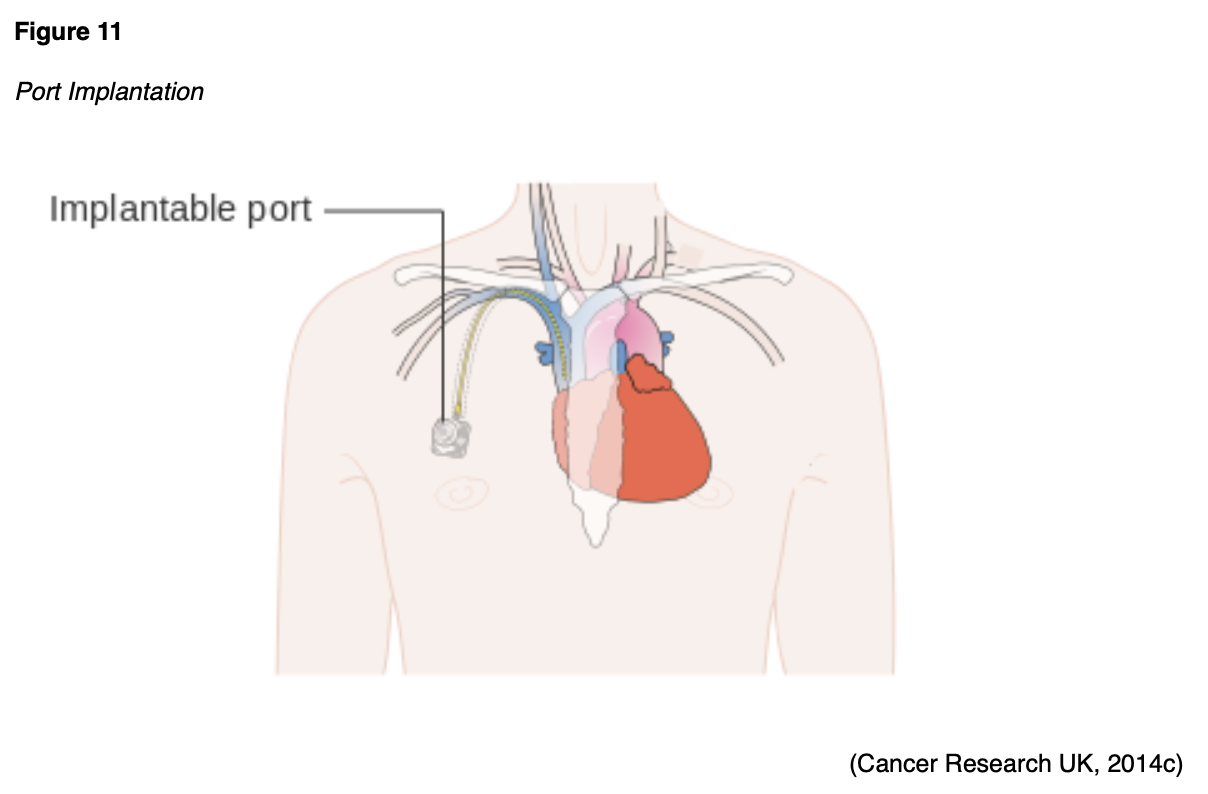
An implanted port is similar to a tunneled catheter, but it is not visible since it resides beneath the subcutaneous tissue. Ports do not require as much maintenance care and do not impede daily activities like PICC lines or tunneled catheters. Ports are also associated with a lower risk of infection than other CVCs (CDC, 2019; Gorski et al., 2016).
CPN Feeding and CVC Care
CPN can be initiated after a patient has been hemodynamically resuscitated; has had their glucose, electrolyte, and acid-base homeostasis established; and can tolerate the fluid volumes involved. CPN is administered using filtration that suits the type of solution/emulsion and infuses via an electronic device equipped with appropriate alarms. Strict adherence to aseptic techniques is advised during all aspects of CPN and CVC care to reduce the risk of catheter-related bloodstream infections (CRBSI). A dedicated line must be allotted for all CPN infusions and labeled for CPN use. No other medications, infusions, or therapies should be infused through the dedicated CPN lumen. According to INS guidelines, the CVC should not be used for routine blood sampling, which is a significant risk factor for CRBSI. The administration sets for CPN must be replaced at least every 24 hours, and current recommendations advise changing the administration set with each new CPN container or bag. Nurses are responsible for monitoring and reporting any potential signs of infection, such as erythema, edema, pain or tenderness, drainage, a fluid pocket in the subcutaneous tunnel, and induration at the exit site or over the pocket. Signs of systemic infection include fevers, chills, rigors, lethargy, disorientation, and confusion in previously alert patients (CDC, 2019; Gorski et al., 2016; Lippincott, 2019).
While CPN formula composition is beyond the scope of this learning activity, the formula typically consists of a high-osmolarity solution with a high proportion of amino acids. In general, the initial dose of dextrose should not exceed 200 g/day to avoid hyperglycemia and refeeding syndrome (see next section). The glucose dose increases each day until it approaches the patient’s energy requirement, and lipids are typically added after the first week. CPN should be discontinued as soon as EN can adequately nourish the patient. Evidence-based guidelines recommend that the dose of CPN should be tapered down as food intake increases. Once a patient tolerates one-half to two-thirds of their food requirement by the enteral route, and there are no other barriers to further improvements in intake, PN should be discontinued. PN should never be suspended to entice increased oral intake. PN does not induce anorexia, and stopping PN does not boost a patient’s appetite (McClave et al., 2016; Mueller et al., 2017).
Complications and Management
Complications associated with CPN occur in 2 major categories: CVC-related issues (e.g., CRBSI, thrombosis, catheter malfunction) and CPN-related issues (e.g., refeeding syndrome, metabolic abnormalities, and organ dysfunction such as hepatic injury; McClave et al., 2016; Mueller et al., 2017).
CRBSI
CRBSI is the most common complication associated with CPN, as several studies have demonstrated an increased risk of infectious complications in patients receiving CPN compared to other patients with CVCs. Proper aseptic insertion technique, meticulous dressing care, and dedicating a single port to CPN reduces this risk. In several clinical trials comparing PN to EN, patients receiving PN had overall superior glycemic control than EN counterparts but were 2 to 4 times more likely to develop CRBSI. Strict infection control protocols are strongly advised regardless of the type of catheter placed to reduce the risk of CRBSI. This includes the following measures:
- handwashing
- aseptic site and hub care (e.g., wearing gloves, prepping the site with topical antiseptics)
- port sterilization before access
- close monitoring of catheter site appearance for redness or inflammation
Many institutional policies enforce the use of chlorhexidine-impregnated dressing over CVCs to reduce the risk of CLABSI rates. There are several best practice protocols for CVC care, which are revised and adapted to each healthcare organization’s specifics. While differences exist according to institution policy, an extensive review of the literature reveals that the vast majority of protocols are premised on preserving the device’s integrity and preventing infection (Gorski et al., 2016; McClave et al., 2016; Mueller et al., 2017).
Catheter Malfunction
Catheter malfunction (e.g., clogging [occlusion] or breakage) is another common complication of CVCs. Catheter occlusion may arise from blood, fat solutions in many PN formulas, or precipitate (abnormal crystal formation in a solution). An occluded catheter is typically managed by instilling a de-clotting agent such as alteplase (TPA) into the catheter to dissolve the clot. When a catheter is cracked, leaking, or broken, the catheter must be repaired or replaced as soon as possible. Symptoms of a fractured catheter can include pain or burning when flushing, swelling, redness, or leakage at the insertion site (Gorski et al., 2016; Lippincott, 2019).
Catheter-Induced Thrombosis
Thrombosis of a blood vessel around a CVC is a serious potential complication of CPN that can be life-threatening if not managed. A thrombus is a stationary clot attached to the vessel wall composed of fibrin and other blood cells. A thrombus can reduce or obstruct blood flow within the vessel, thereby depriving tissues and organs of vital nutrients and inducing tissue ischemia and hypoxia. Since thrombosis can block blood flow in both veins and arteries, complications depend on the clot’s location. The most severe and dangerous complication of venous thrombosis is a pulmonary embolism (PE), a blood clot within the lung. A thrombus detaches from the vessel wall and circulates within the bloodstream, causing a sudden blockage of a vessel (i.e., an embolism). A PE is most commonly caused by DVT, as a piece of the blood clot within the extremity breaks off, travels through the veins, and lodges in the lung’s blood vessels. A PE can completely obstruct blood flow and induce sudden death. It can also cause hypoxia, leading to permanent damage to the lungs or other organs in the body due to insufficient oxygen (Longo, 2019; McCance & Heuther, 2019; Tritschler et al., 2018).
Thrombotic complications associated with CVCs are common and associated with distressing symptoms (e.g., limb swelling, pain, or loss of function), heightened morbidity, catheter dysfunction, increased risk of infection, and higher costs of care. Risk factors for catheter-related thrombosis include larger, multi-lumen catheters. PICC lines have a higher risk of thrombosis than implanted ports or tunneled lines. Depending on the location and extent of the thrombosis, the catheter may or may not need to be removed (Leib et al., 2020; Linkins, 2018; McDiarmid et al., 2017).
For more information on CVCs, including the identification and management of catheter-associated thrombosis, refer to the following NursingCE courses:
- Venous Thromboembolism
- Blood Clotting and Bleeding Disorders
- Vascular Access Devices
CPN Feeding Complications
CPN is associated with a higher risk of feeding complications than EN. The most common metabolic complication of CPN is hyperglycemia, particularly in patients with insulin resistance due to diabetes mellitus, high-dose glucocorticoid therapy, or severe systemic inflammation. Hyperglycemia is worsened by the high levels of glucose (e.g., dextrose) in most CPN formulas. Since critically ill patients have underlying alterations in glucose metabolism, they are more prone to the hyperglycemic complications of CPN. Blood glucose should be monitored several times per day, and insulin may be added to the CPN as indicated to maintain normal average glucose concentrations. Reactive hypoglycemia can occur when high-dextrose, non-insulin-containing CPN is abruptly discontinued. Therefore, to avoid reactive hypoglycemia, CPN should be tapered down slowly before stopping, as noted earlier. Volume overload and fluid retention comprise another common complication of CPN. Hypertonic dextrose CPN formulas stimulate a more intense insulin response than oral glucose. Insulin behaves as a potent antinatriuretic and antidiuretic hormone, potentiating sodium and water retention (AND, 2020; Mueller et al., 2017).
In patients receiving CPN, fluid retention is likely when the total fluid administration exceeds 2 L/day, particularly when patients are not experiencing significant GI losses. Volume overload can be prevented by reducing infusion rates to minimize the need for exogenous insulin therapy, limiting sodium intake, and avoiding overfeeding. Hypertriglyceridemia is a relatively common complication of CPN when the rate of lipid infusion exceeds plasma triglyceride clearance capacity. This is especially concerning for ICU patients since sepsis, renal failure, metabolic alterations in glucose metabolism, and multiple organ failure reduce triglyceride clearance, as outlined earlier in this module. Furthermore, severe pancreatitis is a rare but possible complication of unmanaged severe hypertriglyceridemia. Prolonged CPN, especially when it delivers excess calories, can also lead to hepatic dysfunction, typically manifesting with elevated serum liver enzyme tests (LFTs). Elevated LFTs usually happen within 2 to 4 weeks of initiating CPN but typically normalize, even when CPN is continued. Hepatic complications such as fatty liver and intrahepatic cholestasis occur more frequently with continuous CPN. These conditions can usually be managed by transitioning to cyclic CPN (e.g., CPN is infused for only 12 hours per day; AND, 2020; Mueller et al., 2017).
Refeeding Syndrome
Refeeding syndrome is a potentially fatal condition characterized by severe electrolyte and fluid shifts and metabolic abnormalities in malnourished patients receiving nutritional support. There is no standardized definition or diagnostic criteria for refeeding syndrome, and it can be associated with significant morbidity and mortality. While refeeding syndrome can result from oral, enteral, or parenteral nutrition, it most frequently appears with CPN. Refeeding syndrome’s primary clinical features include alterations in fluid balance, abnormal glucose metabolism, electrolyte disturbances, and vitamin B1 (thiamine) deficiency, as highlighted in Table 9. Metabolic and electrolyte disturbances are primarily caused by the increased use of these nutrients for carbohydrate metabolism. Hypophosphatemia is a classic sign and is present in nearly all cases. Symptoms typically present within 2 to 5 days of starting nutritional support, but some patients can present with asymptomatic depletion of phosphate (AND, 2020; McClave et al., 2016; Mueller et al., 2017).
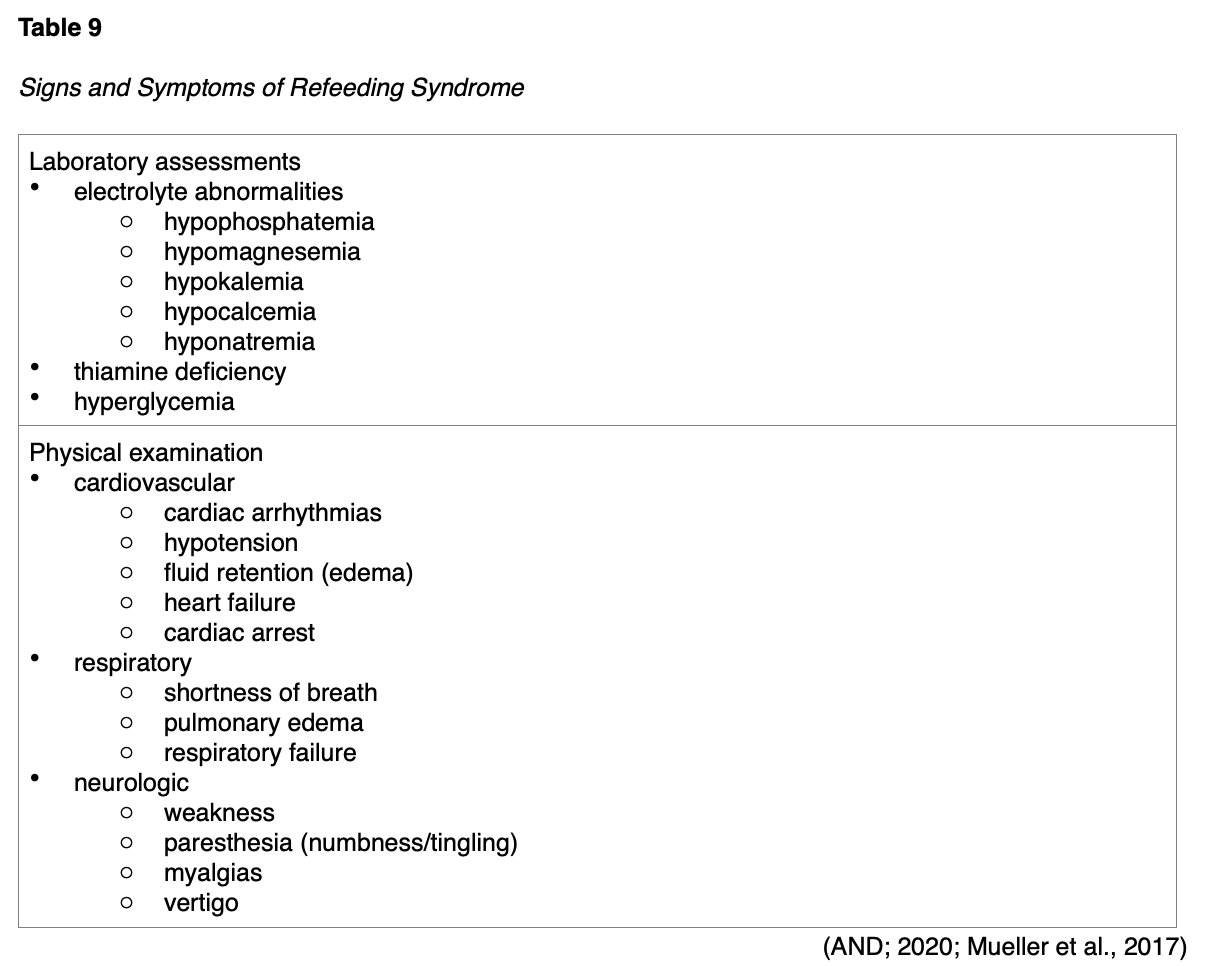
The primary goal of nutritional support is the prevention of refeeding syndrome. Prevention strategies involve identifying and managing underlying risk factors (e.g., severe malnutrition, prolonged NPO status, diuretic use). Such strategies include assessments of baseline electrolytes and corrections of any underlying deficits before initiating EN or CPN. SCCM/ASPEN guidelines recommend adding thiamine supplementation to nutritional support formulas in patients at risk of thiamine deficiency (e.g., patients with underlying alcohol abuse disorders or dependency). The typical thiamine replacement dose is 100 mg daily for 5 to 7 days. Early identification of the warning signs of refeeding syndrome is vital to minimize complications (AND, 2020; McClave et al., 2016; Mueller et al., 2017).
Ethical Considerations in Nutritional Support
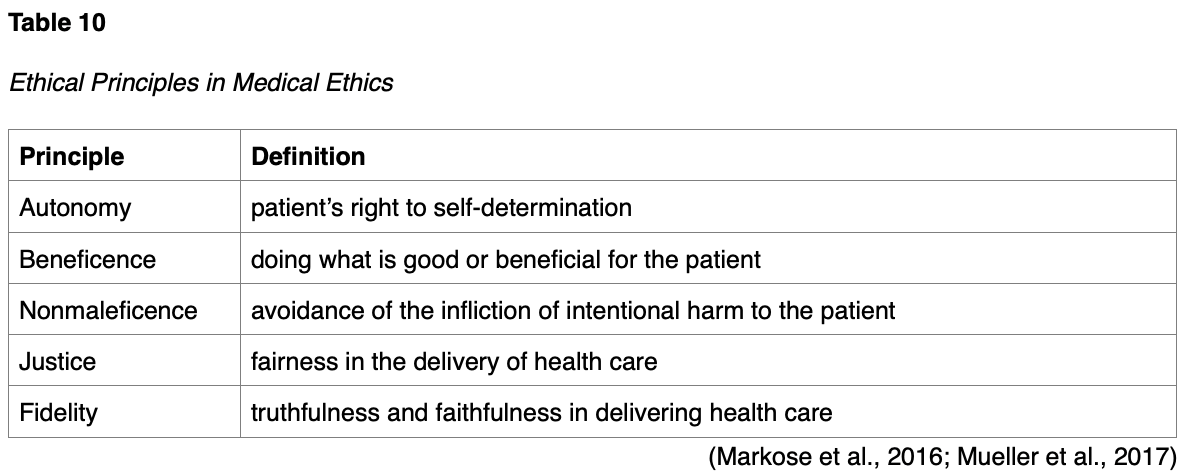
Before initiating EN or CPN, the ethical issues surrounding nutritional support should be considered. Ethics is a discipline studied in nearly all professions that encompasses standards of conduct. Ethics provide the fundamental structure for putting morals or rules of conduct into practice. Despite several misconceptions, ethics do not change with emotions or feelings and are not legally binding. Medical ethics refers to a set of moral standards that govern the behaviors and practices of healthcare professionals. Issues in medical ethics often involve life and death. Ethical arguments related to the role of artificial nutrition and hydration (ANH) are well-cited in the literature on critically ill and dying patients. ANH ethical issues include patient and family wishes, quality of life, goals of care, and the risks and benefits of nutritional therapy in the context of the patient’s diagnosis, prognosis, and long-term care goals (Mueller et al., 2017).
Providing optimal care to critically ill patients requires keen awareness and an understanding of the principles of medical ethics, including autonomy, beneficence, nonmaleficence, justice, and fidelity. These principles are outlined in Table 10. With growing attention on medical futility, the withdrawal or withholding of medical interventions, and aid-in-dying, nurses should not only appreciate the ethical and legal ramifications surrounding these topics but also examine their beliefs and personal biases to ensure care is delivered without prejudice (American Nurses Association [ANA], 2017).
According to the American Medical Association (AMA, 2016), a competent patient with decision-making capacity has the right to decline any medical intervention (including AHN) or request that an intervention be stopped, even when that decision is expected to lead to death. Declining nutrition is a prime example of a patient exercising their right to autonomy. The ANA (2017) position statement on nutrition and hydration for end-of-life care identifies comparable views regarding the acceptance or refusal of clinically appropriate food and fluids, whether delivered by oral or artificial means. Patient (or surrogate) decisions must be respected, provided the decision is based on accurate information and represents patient preferences. If a patient lacks capacity, the patient’s surrogate may decline or ask to stop an intervention on the patient’s behalf. When an intervention is no longer helpful in achieving the patient’s goals for care or desired quality of life, it may be ethically withdrawn. Nutritional support is not indicated when a patient’s prognosis does not warrant continued aggressive therapies or the patient or caregiver refuses nutritional support. The AMA (2016) and the ANA (2017) mutually agree that there is no ethical, moral, or legal difference between withholding care (never starting it) or withdrawing care (stopping it). Furthermore, decisions about accepting or forgoing nutrition and hydration should be honored, including choices about artificially delivered nutrition (e.g., as a means of hastening death). The AMA (2016) urges nurses to work collaboratively with the healthcare team to identify, understand, and advocate for interventions that are congruent with the patient’s goals and preferences early in the course of illness; these steps can help avoid complex ethical dilemmas at the end of life (ANA, 2017).
References
Academy of Nutrition and Dietetics. (2017). Malnutrition measures specification manual: Version 1.2 – October 2017. https://www.eatrightpro.org/-/media/eatrightpro-files/practice/quality-management/quality-improvement/malnutrition-measuresspecificationmanual.pdf
Academy of Nutrition and Dietetics. (2020). Nutrition care manual. https://www.nutritioncaremanual.org/
Academy of Nutrition and Dietetics Evidence Analysis Library. (2012). Critical illness: Executive summary of recommendations. https://www.andeal.org/topic.cfm?cat=4840
American Board of Internal Medicine. (2021). ABIM laboratory test reference ranges – January 2021. https://www.abim.org/~/media/ABIM%20Public/Files/pdf/exam/laboratory-reference-ranges.pdf
American Medical Association. (2016). Code of medical ethics: Caring for patients at the end of life. https://www.ama-assn.org/delivering-care/ethics/code-medical-ethics-caring-patients-end-life
American Nurses Association. (2017). Nutrition and hydration at the end of life. https://www.nursingworld.org/~4af0ed/globalassets/docs/ana/ethics/ps_nutrition-and-hydration-at-the-end-of-life_2017june7.pdf
BruceBlaus. (2013a). Components of the digestive system [image]. https://commons.wikimedia.org/wiki/File:Blausen_0316_DigestiveSystem.png
BruceBlaus. (2013b). Large intestine anatomy [image]. https://commons.wikimedia.org/wiki/File:Blausen_0604_LargeIntestine2.png
BruceBlaus. (2013c). Non-tunneled CVC [image]. https://commons.wikimedia.org/wiki/File:Blausen_0181_Catheter_CentralVenousAccessDevice_NonTunneled.png
BruceBlaus. (2016). Tunneled CVC [image]. https://commons.wikimedia.org/wiki/File:Central_Venous_Access_Device_(Tunneled).png
BruceBlaus. (2017). G-tube [image]. https://commons.wikimedia.org/wiki/File:Gastric_Feeding_Tube_Infant.png
Canadian Malnutrition Task Force. (2021). Subjective global assessment (SGA)- Diagnosing malnutrition. https://nutritioncareincanada.ca/resources-and-tools/hospital-care-inpac/assessment-sga
Cancer Research UK. (2014a). Diagram of the stomach [image]. https://commons.wikimedia.org/wiki/File:Diagram_showing_the_parts_of_the_stomach_CRUK_336.svg
Cancer Research UK. (2014b). PICC [image]. https://commons.wikimedia.org/wiki/File:Diagram_showing_a_PICC_line_CRUK_071.svg
Cancer Research UK. (2014c). Port [image]. https://commons.wikimedia.org/wiki/File:Diagram_showing_an_implantable_port_CRUK_101.svg
Centers for Disease Control and Prevention. (2019). Frequently asked questions about catheters. https://www.cdc.gov/hai/bsi/catheter_faqs.html
DeLegge, M. H., Saltzman, J. R., Seres, D., & Robson, K. M. (2021). Gastrostomy tubes: Placement and routine care. UpToDate. Retrieved March 22, 2021, from https://www.uptodate.com/contents/gastrostomy-tubes-placement-and-routine-care
Feeding Tube Awareness Foundation. (n.d.). Types of tubes. Retrieved March 24, 2021, from https://www.feedingtubeawareness.org/tube-feeding-basics/tubetypes/
Ferguson, M., Capra, S., Bauer, S., & Banks, M. (1999). Development of a valid and reliable malnutrition screening tools for adult acute hospital patients. Nutrition, 15(6), 458-464. https://doi.org/10.1016/s0899-9007(99)00084-2
Gorski, L., Hadaway, L., Hagle, M. E., McGoldrick, M., Orr, M., & Doellman, D. (2016). Infusion therapy standards of practice. Journal of Infusion Nursing, 39(1S), 1-169. https://source.yiboshi.com/20170417/1492425631944540325.pdf
Hodin, R. A., Cochran, A., & Collins, K. A. (2021). Inpatient placement and management of nasogastric and nasoenteric tubes in adults. UpToDate. Retrieved March 20, 2021, from https://www.uptodate.com/contents/inpatient-placement-and-management-of-nasogastric-and-nasoenteric-tubes-in-adults
Hoffer, L., & Bistrian, B. R., & Driscoll, D. F. (2018). Enteral and parenteral nutrition. In J. Jameson, A. S. Fauci, D. L. Kasper D.L., S. L. Hauser, D. L. Longo, & J. Loscalzo (Eds.), Harrison's Principles of Internal Medicine (20th ed.). McGraw-Hill.
Innerbody Research. (2017). Cecum. https://www.innerbody.com/image_dige08/dige44.html
The Joint Commission. (2020). Nutritional and functional screening - Requirement. https://www.jointcommission.org/standards/standard-faqs/critical-access-hospital/provision-of-care-treatment-and-services-pc/000001652/
Jenson, G. L., Cederholm, T., Correia, M. I., Gonzalez, M. C., Fukushima, R., Higashiguchi, T., de Baptista, G. A., Barazzoni, R., Blaauw, R., Coats, A. J., Crivelli, A., Evans, D. C., Gramlich, L., Fuchs-Tarlovsky, V., Keller, H., Llido, L., Malone, A., Mogensen, K. M., Morley, J. E., … Van Gossum, A. (2019). GLIM criteria for the diagnosis of malnutrition: A consensus report from the global clinical nutrition community. Journal of Parenteral and Enteral Nutrition, 43(1), 32-40. https://doi.org/10.1002/jpen.1440
Keller, U. (2019). Nutritional laboratory markers in malnutrition. Journal of Clinical Medicine, 8(6), 775. https://doi.org/10.3390/jcm8060775
Lambell, K. J., Tatucu-Babet, O., Chapple, L., Gantner, D., & Ridley, E. J. (2020). Nutrition therapy in critical illness: A review of the literature for clinicians. Critical Care, 24(35), 1-11. https://doi.org/10.1186/s13054-020-2739-4
Leib, A. D., England, B. S., & Kiel, J. (2020). Central line. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK519511/#_article-19125_s10_
Linkins, L. A. (2018). Prevention of central venous catheter-related thrombosis: Reality or still a dream? The Hematologist, 15(6). https://doi.org/10.1182/hem.V15.6.9032
Lippincott. (2019). Lippincott nursing procedures (8th ed.). Lippincott Williams & Wilkins.
Longo, D. L. (2019). Harrison’s hematology and oncology (3rd ed.). McGraw-Hill Education.
Markose, A., Krishnan, R., & Ramesh, M. (2016). Medical ethics. Journal of Pharmacy & BioAllied Science, 8 (suppl 1), S1-S4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5074007/
McCance, K. L., & Heuther, S. E. (2019). Pathophysiology: The biologic basis for disease in adults and children (8th ed.). Elsevier.
McClave, S. A., Taylor, B. E., Martindale, R. G., Warren, M. M., Johnson, D. R., Braunschweig, C., McCarthy, M. S., Davanos, E., Rice, T. W., Cresci, G. A., Gervasio, J. M., Sacks, G. S., Roberts, P. R., Compher, C., the Society of Critical Care Medicine, & the American Society for Parenteral and Enteral Nutrition. (2016). Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient. Journal of Parenteral and Enteral Nutrition, 40(2), 159-211. https://doi.org/10.1177/0148607115621863
McDiarmid, S., Scrivens, N., Carrier, M., Sabri, E., Toye, B., Huebsch, L., & Fergusson, D. (2017). Outcomes in a nurse-led peripherally inserted central catheter program: A retrospective cohort study. CMAJ Open, 5(3), E535-E539. https://doi.org/10.9778/cmajo.20170010
Mueller, C. M., Lord, L. M., Marian, M., McClave, S. A., & Miller, S. J. (Eds.). (2017). The ASPEN adult nutrition core curriculum (3rd ed.). American Society for Parenteral and Enteral Nutrition.
Nanoxyde. (2011). Enteral assess devices [image]. https://commons.wikimedia.org/wiki/File:Nasogastric_intubation_schema.svg
Paje, D., Rogers, M., Conlon, A., Flanders, S., Bernstein, S., & Choppra, V. (2019). Use of peripherally inserted central catheters in patients with advanced chronic kidney disease: A prospective cohort study. Annals of Internal Medicine, 171(1), 10-18. https://doi.org/10.7326/M18-2937
Pash, E. (2018). Enteral nutrition: Options for short-term access. Nutrition in Clinical Practice, 33(2), 17-176. https://doi.org/10.1002/ncp.10007
Selchick, F. (2021a). Enteral access devices [image].
Selchick, F. (2021b). French (Fr) sizes of feeding tubes [image].
Selchick, F. (2021c). Malnutrition screening tool (MST) [image].
Selchick, F. (2021d). NRS-2002 [image].
Seres, D., Parsons, P. E., & Finlay, G. (2021). Nutrition support in critically ill patients: An overview. UpToDate. Retrieved March 19, 2021, from https://www.uptodate.com/contents/nutrition-support-in-critically-ill-patients-an-overview
Skipper, A., Coltman, A., Tomesko, J., Charney, P., Porcari, J., Piemonte, T. A., Handu, D., & Cheng, F. W. (2020). Position of the academy of nutrition and dietetics: Malnutrition (undernutrition) screening tools for all adults. Journal of the Academy of Nutrition and Dietetics, 120(4), 709-713. https://doi.org/10.1016/j.jand.2019.09.011
Tenbergen. (2018). Nasoenteric tube with stylet [image]. https://upload.wikimedia.org/wikipedia/commons/8/80/Enteral_feeding_tube.png
Tritschler, T., Kraaijpoel, N., Gal, G. L., & Wells, P. S. (2018). Venous thromboembolism: Advances in diagnosis and treatment. JAMA, 320(15), 1583–1594. https://doi.org/10.1001/jama.2018.14346
Tse, A., & Schick, M. (2020). Central line placement. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK470286/
van Zanten, A. R., De Waele, E., & Wischmeyer, P. E. (2019). Nutrition therapy and critical illness: Practical guidance for the ICU, post-ICU, and long-term convalescence phases. Critical Care, 23(368), 1-10. https://doi.org/10.1186/s13054-019-2657-5
White, J. V., Guenter, P. Jensen, G., Malone, A., Schofield, M., Academy Malnutrition Work Group, ASPEN. Malnutrition Task Force, & ASPEN Board of Directors. (2012). Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition. Journal of Parenteral and Enteral Nutrition, 36(3), 275-283. https://doi.org/10.1177/0148607112440285
World Health Organization. (n.d.). Body mass index – BMI. Retrieved March 19, 2021, from https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi