The purpose of this module is to review non-pharmacological pain reduction strategies, as well as the non-opioid pharmacological treatment of pain to enhance the knowledge and clinical skill of the advanced practice nurse providing care to patients with pain.
...purchase below to continue the course
s circulation, relaxing the patient's muscles, thereby reducing anxiety. It decreases pain by increasing
circulation to the area.
Massage techniques should be avoided on areas where skin integrity is impaired, or there is a change in the appearance of the skin, a blood clot is possible, or an infection is present.
Acupuncture and acupressure involve the stimulation of subcutaneous tissues at specific points using needles (acupuncture) or the digits (acupressure). Only individuals with specialized training can perform these techniques.Therapeutic ultrasound delivers heat and enhances blood flow to deep tissues for improved and accelerated injury healing (Berger et al., 2013; USDHHS, 2019).Cognitivebehavioral therapy (CBT) is another component of the multimodal approach to pain management. It focuses on changing how a patient perceives pain to reduce distress and alleviate or suppress discomfort. Some of the most common CBT strategies include distraction, relaxation, guided imagery, biofeedback, and Reiki therapy.
- Distraction directs the patient's attention to something other than the pain, as it is well documented that decreased attention to the presence of pain can reduce the perceived pain level. Distraction technique can be used during a painful diagnostic procedure or while waiting for an analgesic to take effect. Specific strategies include ambulation, deep breathing, visitors, television, games, prayer, and music.
- Relaxation techniques include meditation, yoga, and progressive muscle relaxation.
- Meditation involves focusing on an object sitting in a comfortable position and clearing the mind of all thoughts. Using meditation for twenty minutes, twice a day, decreases heart rate, blood pressure, and the respiratory rate.
- Yoga has been practiced in India for centuries and typically includes assuming poses, breathing exercises, and meditation. Yoga increases muscle strength and tone, reduces anxiety, and lowers blood pressure.
- Progressive muscle relaxation involves slow, deep abdominal breathing while progressively tightening and relaxing the muscles. The technique is typically performed in a logical sequence, such as beginning with the feet and moving up the rest of the body.
- Guided imagery involves pleasant mental images such as a lake or the mountains. This technique shifts the patient's thoughts away from the pain. It can be used during painful diagnostic procedures. Patients must be able to concentrate to benefit from the use of guided imagery, which makes this technique more difficult for patients who experience acute and severe pain.
- Biofeedback is a therapy that uses electric sensors to assist a patient in controlling physiological responses such as heart rate and blood pressure.
- Reiki is a natural healing technique in which a therapist channels energy into a patient by touch to promote physical and emotional healing (Berger et al., 2013; Lin et al., 2017; USDHHS, 2019).
Interventional Pain Procedures
Interventional pain medicine is a medical subspecialty of pain medicine that diagnoses and treats pain with minimally invasive interventions geared toward alleviating pain and minimizing the use of pharmacological therapies. Most interventional pain procedures are performed on an outpatient basis and are, therefore, more cost-effective. Procedures vary in their degree of complexity and invasiveness. Some are considered minor procedures that can be performed in the outpatient office setting while others require image-guidance (using ultrasound, fluoroscopy, or computed tomography) in a radiology department by an interventional radiologist. Some commonly used interventional pain procedures include:
- Trigger point injections- the use of dry needling or local anesthetic to inject and disrupt palpable, tense bands of skeletal muscle fibers to relax and lengthen the fibers. These may be done intramuscular or intrabursal (to treat bursitis).
- Joint injections- typically involves the use of a corticosteroid and/or a local anesthetic that is injected into facet joint(s) or intra-articular injections into the shoulder, elbow, wrist, knee, ankle, etc. to manage arthritis or injury.
- Peripheral or sympathetic nerve blocks- the use of a local anesthetic mixed with a corticosteroid that is injected or infused around a specific nerve or group of nerves to treat or diagnose postoperative pain, neuropathies, neuropathic pain, and chronic pain. An example is a celiac plexus block, which may help relieve abdominal pain related to chronic pancreatitis.
- Epidural steroid injections- an injection of corticosteroid medication into the epidural space (outside the dural sac) to treat neuropathic leg (related to a nerve root irritation in the low back) or arm pain (less common, related to a nerve root irritation in the neck).
- Radiofrequency ablation- the use of high frequency energy waves to ablate or stun nerves that may be contributing to pain; administration can be conventional or pulsed.
- Neuromodulation- activate central or peripheral nerves using electrical, ultrasound, or magnetic stimulation devices to relieve pain or reduce pain sensitivity. An example includes vagus nerve stimulation in the treatment of cluster and migraine headaches.
- Spinal cord stimulators- uses the concept of neuromodulation (above) in a permanently implanted stimulator along the lower spinal cord to manage lower extremity neuropathic pain.
- Implanted intrathecal pain pump- allows for the delivery of opioids, baclofen (Lioresal), or other medications directly into the spinal fluid to receptors on the spinal cord or the brain using a fraction of the dose required with oral administration, reducing many of the adverse drug effects. Risks include infection/meningitis, delayed respiratory depression, granuloma formation, and hypogonadism (USDHHS, 2019).
Pharmacological Interventions
Pharmacologic therapy is usually a component of an effective, multimodal pain management plan, particularly for the treatment of chronic pain. Analgesics are a mainstay for relieving pain and are comprised of two main categories: nonopioids and opioids (USDHHS, 2019).
Nonopioid Analgesics
Nonopioid analgesics have anti-inflammatory, antipyretic, and analgesic effects. However, the properties among the different medications vary, as each drug has its independent mechanism of action, as well as risks and benefits. Non-opioid medications can mitigate and minimize opioid exposure (USDHHS, 2019). Two of the most common types of nonopioid analgesics include nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen (Tylenol). These medications are appropriate for the treatment of mild to moderate pain. They are easily accessible to patients as many are available over the counter and do not require a prescription (USDHHS, 2019).
First-generation NSAIDs include ibuprofen (Motrin, Advil), indomethacin (Indocin), diclofenac (Zorvolex), ketorolac (Toradol), nabumetone (Relafen) and meloxicam (Mobic). These drugs inhibit both COX-1 and COX-2, which are forms of the enzyme cyclooxygenase that converts arachidonic acid into prostaglandins. Both COX-1 and COX-2 are integral components of the inflammatory process, but COX-1 also protects the gastrointestinal tract and is involved in kidney and platelet function. Therefore, when COX-1 is inhibited by first-generation NSAID therapy, inflammation, pain, and fever are reduced, but gastric ulceration, renal impairment, and bleeding can occur. First-generation NSAIDs are also given to prevent stroke and myocardial infarction and to treat the discomfort of rheumatoid arthritis and osteoarthritis. Second generation NSAIDs, such as celecoxib (Celebrex), inhibit only COX-2. It decreases inflammation, pain, and fever, but it does not reduce platelet aggregation. It is administered to treat osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, and dysmenorrhea (U.S. Food & Drug Association [FDA], 2016).
While NSAIDs can provide significant relief from many types of pain, they are not without risks. NSAIDs are associated with GI, cardiovascular, and renal effects. Some of the most commonly reported side effects include GI bleeding, gastric ulcers, acute kidney injury, bleeding events, heart failure secondary to sodium retention, as well as myocardial infarction (MI), and stroke. Not all NSAIDs pose the same level of risks. For instance, cardiovascular risks, including thrombosis and MI are heightened in COX-2 selective NSAIDs such as Celecoxib (Celebrex), whereas GI side effects are reduced. Semi-selective NSAIDs such as meloxicam (Mobic) and indomethacin (Indocin) pose less cardiovascular risk than COX-2 selective, however these medications should still be used with caution in patients who are at increased cardiovascular risk. Gastrointestinal risks such as bleeding and ulcers are increased in nonselective NSAID medications, including ibuprofen (Motrin) and naproxen (Naprosyn) (Shah, 2018).
According to the American Geriatrics Society Beers Criteria (BC) for Potentially Inappropriate Medication Use in Older Adults, indomethacin (Indocin), ketorolac (Toradol), ibuprofen (Motrin), and meloxicam (Mobic) should be avoided in older adults. Due to the risk of GI bleeding, peptic ulcer disease, and kidney damage, it is advised that these medications are instead replaced with celecoxib (Celebrex), naproxen (Aleve) or ibuprofen (Motrin) in combination with proton pump inhibitors (PPIs) for GI protection. The use of misoprostol (Cytotec) or PPIs such as omeprazole (Prilosec) or pantoprazole (Protonix) reduces the GI risks but does not eliminate them (American Geriatrics Society [AGS], 2015).
Aspirin, also known as acetylsalicylic acid (ASA) is the oldest medication in this category. It is currently the most commonly used drug in the world and has proven to be lifesaving in the prevention of cardiovascular disease (Desborough et al., 2017). Due to its antiplatelet properties, many providers prescribe a dose of 81 mg to 325 mg once daily as prophylaxis for myocardial infarction. Additionally, the emergency treatment protocols for acute myocardial infarction include the administration of chewable non-enteric coated aspirin (162 to 325 mg) at the first recognition of symptoms. ASA is not without risks, and while it is considered cardio-protective at low doses, it carries an Increased risk for GI side effects such as GI bleeding and ulcers (Switaj et al., 2017).
Salicylism toxicity, otherwise known as aspirin poisoning, is a serious condition that occurs due to the intentional or accidental overdose of salicylates. The condition develops when aspirin levels rise above the therapeutic range and can occur from the acute ingestion of large doses of aspirin at one time, or due to chronic intake of small to large doses over a more extended period. The most common clinical manifestations of the condition include ringing in the ears (tinnitus), dizziness, and headache. Serious symptoms include hyperventilation, agitation, fever, convulsions, disorientation, confusion, hallucinations, respiratory arrest, and coma. The condition has high morbidity and mortality; at least 1-2% of patients will die. Overdose of other NSAIDs such as ibuprofen (Motrin, Advil) can occur and present with manifestations similar to those of aspirin; however, generally, they are not as severe (Runde et al., 2019). Reye syndrome is a rare but serious complication that occurs when aspirin is administered for fever reduction in children and adolescents who have a viral illness, such as chickenpox or influenza. Pediatric patients should never be given aspirin to manage a fever. Awareness of this syndrome has dramatically reduced its occurrence (Desborough et al., 2017).
Acetaminophen (Tylenol) is one of the most popular analgesics in the US, as it is an effective treatment for alleviating pain, fever, allergy, cough, cold, flu, and sleeplessness. It is often an ingredient in over-the-counter cough and cold remedies. Like aspirin, acetaminophen blocks pain by inhibiting prostaglandin synthesis of COX-1 and COX-2, thereby suppressing pain and fever. However, acetaminophen (Tylenol) does not suppress inflammation or platelet aggregation. The medication is dosed at 325 mg to 650 mg every 4 to 6 hours as needed, or 1 g every 6 hours as needed. However, the short-term maximum daily dose is not to exceed 4 g per day for patients without risk factors, as acetaminophen carries a severe risk for overdose and subsequent hepatotoxicity. The long-term maximum daily dose is 2 g per day. Due to the heightened risk for liver damage and acute liver failure when consumed in higher than recommended doses, the FDA has limited all acetaminophen products to 325 mg per dosage unit. Also, the FDA has enforced the need for boxed warnings to be added to all acetaminophen products to highlight the potential for severe liver injury, including liver failure with overuse. Acetaminophen is also frequently combined with an opioid in some pain medications such as hydrocodone/acetaminophen (Vicodin) and oxycodone/acetaminophen (Percocet). Some combination products contain as much as 650 mg per tablet, and patients are not always aware that acetaminophen is an ingredient in the combined medications (FDA, 2018a).
Patients should be counseled on the risk for acetaminophen (Tylenol) overdose and encouraged to routinely check the labels of all combination analgesics to determine the amount of acetaminophen contained in the product before ingesting. Further, frequent alcohol use while taking large doses of acetaminophen contributes to the risk of liver damage. Patients with a preexisting liver injury such as cirrhosis, fatty liver, or hepatitis, as well as those who consume more than three alcoholic drinks per day, should limit or avoid the use of acetaminophen as much as possible (Burns et al., 2019).
Acetaminophen (Tylenol) overdose is a significant cause of overdose-related liver failure and death in the US; however, when identified early, mortality rates are low. Acetaminophen is rapidly absorbed through the gastrointestinal tract within the duodenum, and about 90% of the drug is metabolized in the liver. The onset of liver injury is rapid, and diagnosis is characterized by marked elevations in plasma aminotransferases (liver enzymes) and rising prothrombin time (PT)/international normalized ratio (INR). The clinical course of acetaminophen poisoning follows four sequential stages, as outlined below.
- Stage I (30 minutes to 24 hours): nausea, vomiting, lethargy, diaphoresis, and pallor;
- Stage II (24 to 72 hours): laboratory evidence of hepatotoxicity and nephrotoxicity become apparent, including hyperbilirubinemia, elevated PT, and clinical manifestations such as right upper quadrant (liver) pain and tenderness and hepatomegaly;
- Stage III (72 to 96 hours): elevations in liver function enzyme tests peak by 96 hours (plasma alanine transaminase [ALT] and aspartate aminotransferase [AST] levels may exceed 10,000 IU/L), hyperbilirubinemia (bilirubin usually exceeding 4.0 mg/dL), and clinical manifestations such as jaundice, confusion (hepatic encephalopathy), bruising or bleeding, oliguria, and multiorgan system failure, which may lead to death. Death most commonly occurs during stage III.
- Stage IV (four days to two weeks): patients who survive stage III enter a recovery phase that usually begins around day four following the overdose. Patients often develop chronic liver changes, including necrosis and chronic liver disease; some patients may eventually need a liver transplant (Burns et al., 2019).
It is recommended that adult patients who present within four hours of a potentially toxic ingestion of acetaminophen (a single dose of 7.5 g or greater) undergo gastrointestinal decontamination with activated charcoal (AC). AC is a gastric lavage technique that induces emesis, thereby limiting the absorption of acetaminophen and reducing the need for N-acetylcysteine (Acetadote) treatment. N-acetylcysteine (Acetadote) is the antidote for acetaminophen overdose and poisoning. It should be given to all patients at significant risk for hepatotoxicity. Severe hepatotoxicity is uncommon, and death is rare when this antidote is administered within eight hours of the acetaminophen overdose. Acetylcysteine decreases the build-up of hepatotoxic metabolites from the acetaminophen overdose to prevent or lessen the damage to the liver. It can be given orally or intravenously, and there are several protocols available for administration which vary according to institution policy and patient tolerance (Heard et al., 2019).
Adjuvant Analgesics
Other types of non-opioid analgesics include anticonvulsants, antidepressants (particularly serotonin-norepinephrine reuptake inhibitors [SNRIs] and tricyclic antidepressants [TCAs]), as well as topical analgesics and some types of anxiolytics. Often referred to as adjuvant analgesics, many medications within these classes are prescribed in addition to a primary analgesic, such as an opioid analgesic. The goal is to provide a synergistic effect, heightening pain relief while reducing the need for and dosage of the opioid. A reduced dosage of the opioid minimizes the risk of adverse effects and opioid dependency. These adjuvant medications can help alleviate other manifestations that aggravate pain (depression, seizures, inflammation), and are useful for treating neuropathic pain (Qaseem et al., 2017). According to the USDHHS (2019), first-line pharmacologic therapy for neuropathic pain is not opioids, but instead includes anticonvulsants, SNRIs, TCAs, and topical analgesics. While these medications are not opioids, they still pose serious risk of adverse effects and require close monitoring. Each category is outlined briefly below.
Anticonvulsants
Anticonvulsants are medications initially developed to treat seizures and are often called antiseizure drugs. They are commonly used to treat different pain syndromes; they are particularly useful in neuropathic pain conditions such as peripheral neuropathy, postherpetic neuralgia (PHN), and migraines. Increasingly, these medications are also used as part of a multimodal approach for the treatment of perioperative pain to reduce the need for narcotics and opioids postoperatively. Gabapentin (Neurontin) and pregabalin (Lyrica) are most commonly prescribed for chronic neuropathic pain such as PHN and diabetic neuropathy, and Lyrica is also FDA-approved for fibromyalgia management (USDHHS, 2019). According to findings from a 2017 Cochrane Database Systematic Review, when administered at doses of 1800 mg to 3600 mg daily, gabapentin can provide adequate levels of pain relief to patients with PHN and peripheral diabetic neuropathy. However, while gabapentin has been shown to reduce pain for some patients with chronic neuropathy significantly, it is also associated with increased risk for sedation, fatigue, changes in mood, and may trigger depressive episodes. Therefore, it should be used with caution in patients with concomitant psychiatric conditions or those with a history of depression, suicidal thoughts or ideation (USDHHS, 2019; Wiffen et al., 2017).
Carbamazepine (Tegretol) is FDA-approved for the treatment of trigeminal neuralgia (TN). Carbamazepine inhibits voltage-gated sodium channels, reducing the excitability of neural membranes, and potentiates gamma-aminobutyric acid (GABA) receptors. The usual starting dose of carbamazepine is 100 to 200 mg twice daily, and it is recommended that the daily dose is increased by 100 mg every other day until sufficient pain relief is attained or until intolerable adverse effects prevent further upward titration. For the management of TN pain, the standard total maintenance dose is 300 to 800 mg per day, administered in two or three divided doses. The maximum suggested daily dose is 1200 mg. The most common adverse effects include dizziness, sedation, disturbances in concentration, ataxia, and visual disorders such as diplopia. It must be used with caution in patients on cancer chemotherapy that cause bone marrow suppression because carbamazepine can additionally induce leukopenia. Other potentially serious but uncommon adverse effects include Stevens-Johnson syndrome, systemic lupus erythematosus, toxic epidermal necrolysis, elevated liver enzymes, and hepatotoxicity, as well as hyponatremia and aplastic anemia. Routine laboratory monitoring, including complete blood count, serum sodium, and liver function tests, should be done to monitor for these serious adverse effects. In addition, patients should be educated on the importance of avoiding grapefruit juice while taking carbamazepine, as it inhibits the metabolism of the medication, can increase its therapeutic effects, and heighten adverse effects (Al-Quliti, 2015).
Topical Analgesics
Topical lidocaine (Lidoderm) patch is FDA-approved for the treatment of PHN but is also used for a variety of other pain conditions. It is considered a safe, well-tolerated, and effective treatment option for the management of certain types of localized pain. It poses a low risk for systemic effects as only a very small fraction of the dose reaches the systemic circulation and may be used for extended periods. It does not pose the potential for abuse, addiction, dependence, or tolerance. Available by prescription only, it is dispensed in the form of a medicated patch, usually 10 cm x 14 cm, comprised of 5% lidocaine-containing hydrogel adhesive. The patch is applied to the affected area and remains in place for up to 12 hours, exerting localized analgesic effects without inducing numbness. It works by decreasing the nerve membrane permeability to sodium ions, inhibiting depolarization, and transmission of pain signals. In addition, there is an associated cooling effect that accompanies the application of the hydrogel to the affected area. It is essential that patients are instructed to apply the patch to intact skin only, it should remain in place for 12 hours, and then be removed for at least 12 hours, at which time a new patch may be reapplied. The most common adverse effects include local skin irritation, erythema, and inflammation at the application site (Endo Pharmaceuticals, 2018).
Capsaicin (Capsagel, Salonpas) is a topical analgesic derived from chili pepper extract; it is a neuropeptide-releasing agent that targets peripheral sensory neurons. It is applied to the skin to control peripheral nerve pain, and its benefits in managing chronic neuropathic pain have been widely studied. Available primarily over the counter in the form of a gel or patch, it depletes neurotransmitters of substance P, thereby reducing pain perception. It has several potential adverse effects that primarily affect the site of application, including pain, erythema, pruritus, skin eruptions such as rash, lesions, vesicles, skin dryness, hives, and swelling (Derry et al., 2017).
Tricyclic Antidepressants (TCAs)
TCAs are helpful in reducing neuropathic pain, as well as a variety of other chronic pain conditions. The most commonly prescribed TCAs used for pain include amitriptyline (Elavil) and nortriptyline (Pamelor). They have independent analgesic properties and are known to potentiate the effects of opioids. By enhancing the effects of serotonin and norepinephrine, TCAs also treat depression, which is a significant factor associated with chronic pain as outlined earlier. Unfortunately, the disadvantage of TCAs is that they are associated with several adverse effects, including orthostatic hypotension, dry mouth, dizziness, weight gain, memory impairment, urinary retention, constipation, sedation, tachycardia, and cardiac conduction abnormalities (particularly QTc interval prolongation). Best practice guidelines recommend that TCAs be initiated at low doses and gradually titrated depending on tolerance to achieve optimal effect. Further, to minimize the effects of orthostatic hypotension and sedation, patients should be advised to take the medication at bedtime. Additional instructions for patients experiencing adverse effects while taking TCAs include the following:
- Avoid sudden changes in position and sit or lie down if feeling dizzy;
- Increase fluid intake and sip fluids throughout the day;
- Increase fiber intake;
- Increase physical activity;
- Take a stimulant laxative and a stool softener as needed (Wang et al., 2018).
- Tricyclic antidepressants and skeletal muscle relaxants (cyclobenzaprine [Flexeril], carisoprodol [Soma]) should be avoided/used with caution in older adults secondary to anticholinergic effects (Terrery, 2016).
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
According to the USDHHS (2019), SNRIs, such as duloxetine (Cymbalta) and venlafaxine (Effexor), are useful for a variety of chronic pain conditions, including musculoskeletal pain, fibromyalgia, and neuropathic pain conditions. The primary benefit of these medications over TCAs is that they have better safety profiles and significantly fewer adverse effects which leads to greater tolerability and increased compliance. SNRIs are associated with reduced risk of drowsiness, cognitive impairment, and cardiac conduction abnormalities. However, these medications are still not without risks, as they have the potential to induce hepatotoxicity, anorexia, fatigue, and sexual dysfunction. Duloxetine (Cymbalta) is FDA-approved for peripheral diabetic neuropathy and fibromyalgia but is also used for chronic musculoskeletal pain. The recommended dose is 60 mg per day, but the patient may be started at 30 mg once daily for one week before increasing to the recommended dose. Venlafaxine (Effexor XR) is not FDA-approved for any pain conditions, but it is commonly used off-label for the treatment of neuropathic pain and other chronic pain. Pain relief is usually achieved with a dose of 75 to 225 mg per day. A benefit of these medications is their concurrent effect on mood disorders. As with all antidepressant medications, the patient must be assessed for suicidal thoughts or ideations before starting therapy, and ongoing throughout treatment (USDHHS, 2019; Wang et al., 2018).
Skeletal Muscle Relaxants (SMRs)
Similar to NSAIDs (discussed above), the American College of Physicians (ACP) recommends the use of SMRs prior to opioids for acute pain based on moderate quality evidence of the risks versus benefits of these medication. SMRs, such as cyclobenzaprine (Flexeril) and carisoprodol (Soma), function by potentiating norepinephrine, antagonizing serotonin, and/or blocking the neuromuscular junction by binding to acetylcholine receptors. They resulted in a small improvement in pain relief in most studies, but no significant effect on function, as opposed to NSAIDs, which did both. They are associated with central nervous system effects, such as sedation and dizziness. They are also anticholinergic, and are therefore not recommended in older patients and may cause dry mouth, constipation, etc. Some medications in this class have specific indications, such as baclofen (Lioresal) which may be administered intrathecally or orally to treat painful spasticity associated with certain underlying neurological conditions such as stroke and multiple sclerosis (MS)(Qaseem et al., 2017).
Glucocorticoids
Glucocorticoids reduce pain by decreasing inflammation, and therefore are useful in treating painful inflammatory conditions such as rheumatoid arthritis and gout. This includes dexamethasone (Decadron), methylprednisolone (Medrol Dosepack), and prednisone (Deltasone). Long-term use of systemic steroids can have several serious adverse effects, including but not limited to adrenal insufficiency, hyperglycemia, bone loss, skin thinning, cataracts, weight gain, and immunosuppression. Therefore, these medications are not advised for long-term use; they should not be stopped abruptly, but should be tapered downward as soon as possible (Berger et al., 2013).
Bisphosphonates
Bisphosphonates such as alendronate (Fosamax), ibandronate (Boniva), denosumab (Xgeva), and zoledronic acid (Zometa, Reclast) are indicated for the prevention and treatment of osteoporosis. Additionally, they are also useful in the treatment of cancer-related bone pain due to malignant bone metastases or primary bone cancers. These medications work by inhibiting the action of osteoclast cells, decreasing bone turnover, and increasing bone density (Payne et al., 2017). Bisphosphonates carry serious risks, including irritation of the upper GI tract, hypocalcemia, medication-related osteonecrosis of the jaw (MRONJ), and atypical femur fracture (AFF). Their use is contraindicated in patients with hypocalcemia, esophageal stricture, upper GI disease, as well as those with severe renal dysfunction and creatinine clearance of less than 35mL/min. Before starting bisphosphonate therapy, patients should be fully educated on the potential risks and warnings associated with bisphosphonate therapy. Instructions for patients who take oral bisphosphonates include the following:
- Take first thing in the morning with a full glass of water while sitting or standing.
- Remain sitting or standing for at least 30 min after taking the medication (60 minutes for ibandronate [Boniva]).
- Do not eat or drink anything for at least 30 min after taking the medication (60 minutes for ibandronate [Boniva]) (American Association of Clinical Endocrinologists and the American College of Endocrinology [AACE/ACE], 2016).
Antihistamines
Less commonly, antihistamines are used as adjunctive therapy with certain types of opioids. These antagonists block histamine receptors in the body. Hydroxyzine (Atarax, Vistaril) potentiates the effects of opioid analgesics, reduces anxiety, and promotes sedation, aiding in sleep. However, antihistamines may potentially cause several adverse effects, including drowsiness, dry mouth, restlessness (including restless leg syndrome), irritability, nervousness, and difficulty passing urine (American Cancer Society [ACS], 2019).
For additional information, proceed to the third part of this 3-part series entitled, Part 3: Opioid Prescribing and Monitoring
References
Al-Quliti, K. W. (2015). Update on neuropathic treatment for trigeminal neuralgia. Neurosciences, 20(2), 107-114. https://doi.org/10.17712/nsj.2015.2.20140501
American Association of Clinical Endocrinologists and American College of Endocrinology (2016). Clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis - 2016. Endocrine Practice, 22(Suppl 4), 1-42. https://doi.org/10.4158/EP161435.GL
American Cancer Society. (2019). Non-opioids and other drugs used to treat cancer pain. https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/pain/non-opioids-and-other-drugs-to-treat-cancer-pain.html
American Geriatrics Society. (2015). American Geriatrics Society 2015 Beers
Criteria for potentially inappropriate medication use in older adults. https://www.guidelinecentral.com/summaries/american-geriatrics-society-2015-updated-beers-criteria-for-potentially-inappropriate-medication-use-in-older-adults/#section-society
Berger, A. M., Shuster, J. L., & Von Roenn, J. H. (2013). Principles and practices of palliative care and supportive oncology (3rd ed.). Lippincott Williams & Wilkins
Burns, M. J., Friedman, S. L., & Larson, A. M. (2019). Acetaminophen (paracetamol) poisoning in adults: Pathophysiology, presentation, and diagnosis. UpToDate. https://www.uptodate.com/contents/acetaminophen-paracetamol-poisoning-in-adults-pathophysiology-presentation-and-diagnosis?search=Acetaminophen%20(paracetamol)%20poisoning%20in%20adults:%20Pathophysiology,%20presentation,%20and%20diagnosis&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H1
Derry, S., Rice, A. S. C., Cole, P., Tan, T., & Moore, R. A. (2017). Topical capsaicin (high concentration) for chronic neuropathic pain in adults (review). Cochrane Database of Systematic Reviews, 1, 1-67. https://doi.org/10.1002/14651858.CD007393.pub4.
Desborough, M. J., & Keeling, D. M. (2017). The aspirin story – from willow to wonder drug. British Journal of Haematology, 177, 674-683. https://doi.org/10.1111/bjh.14520
Endo Pharmaceuticals. (2018). Lidoderm® (lidocaine patch 5%). https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/020612s014lbl.pdf
Heard, K., & Dart, R. (2019). Acetaminophen (Paracetamol) poisoning in adults: Treatment. UpToDate. https://www.uptodate.com/contents/acetaminophen-paracetamol-poisoning-in-adults-treatment?search=acetaminohpen%20poisoining&source=search_result&selectedTitle=1~91&usage_type=default&display_rank=1
Lin, Y. C., Wan, L., & Jamison, R. N. (2017). Using integrative medicine in pain management: An evaluation of current evidence. Anesthesia & Analgesia, 125(6), 2081-2093. https://doi.org/10.1213/ANE.0000000000002579,
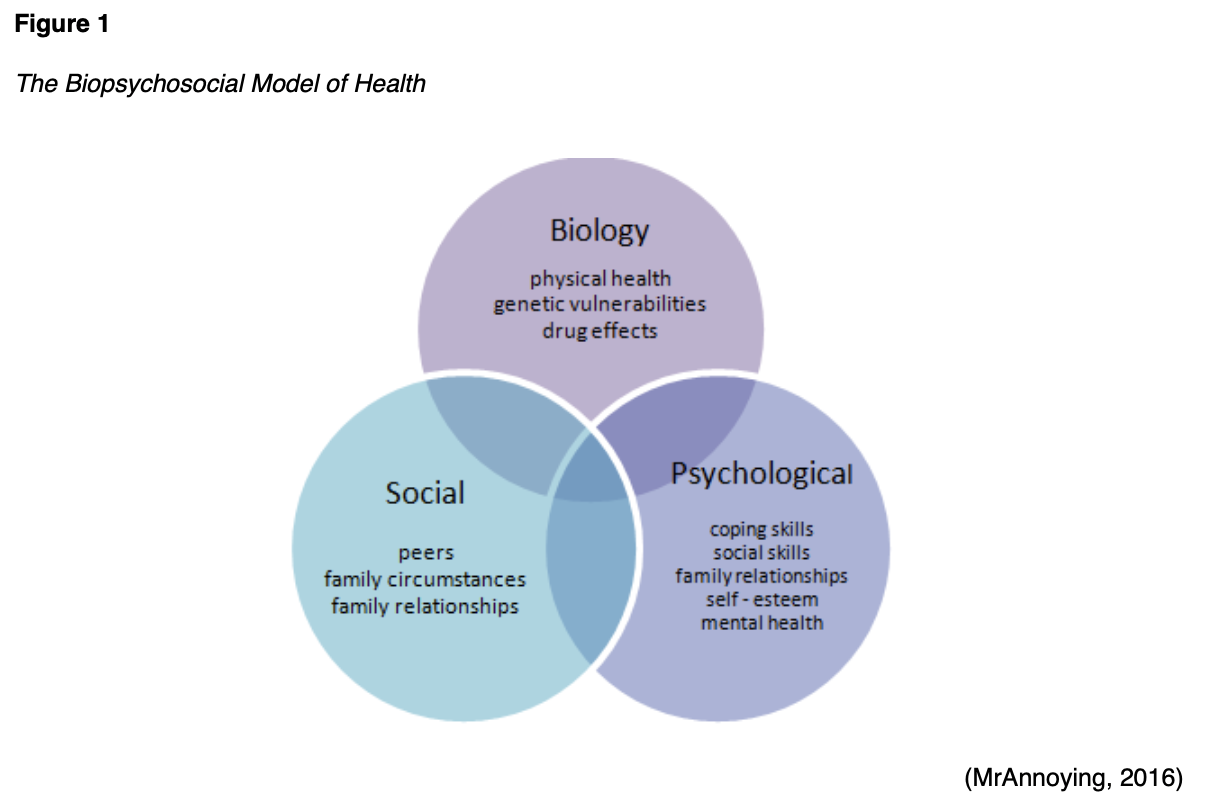
MrAnnoying. (2016). The biopsychosocial model of health [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Biopsychosocial_Model_of_Health_1.png
Payne, K. F., Goodson, A. M., Tahim, A. S., Rafi, I., & Brennan, P. A. (2017). Why worry about bisphosphonate-related osteonecrosis of the jaw? A guide to diagnosis, initial management, and referral of patients. British Journal of General Practice, 67(660), 330-331. https://doi.org/10.3399/bjgp17X691565
Qaseem, A., Wilt, T. J., Mclean, R. M., & Forciea, M. A. (2017). Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine,166(7), 514-530. https://doi.org/10.7326/m16-2367
Runde, T. J., & Nappe, T. M. (2019). Salicylates toxicity. StatPearls [Internet], https://www.ncbi.nlm.nih.gov/books/NBK499879/
Shah, V. (2018). NSAIDS: Are they all the same?
https://www.clinicalcorrelations.org/2018/02/01/nsaids-are-they-all-the-same/
Switaj, T. L., Christensen, S. R., & Brewer, D. M. (2017). Acute coronary syndrome: Current treatment. American Family Physician, 95(4), 232-240. https://www.aafp.org/afp/2017/0215/p232.pdf
Terrery, C. L., & Nicoteri, J. A. (2016). The 2015 American Geriatric Society Beers Criteria: Implications for nurse practitioners. The Journal for Nurse Practitioners,12(3), 192-200. https://doi.org/10.1016/j.nurpra.2015.11.027
US Department of Health and Human Services. (2019). Pain management best practices inter-agency task force report: Updates, gaps, inconsistencies, and recommendations. https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf
US Food & Drug Association. (2016). Nonsteroidal anti-inflammatory drugs (NSAIDs). https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/nonsteroidal-anti-inflammatory-drugs-nsaids
US Food & Drug Administration. (2018). FDA drug safety communication: Prescription acetaminophen products to be limited to 325 mg per dosage unit; Boxed warning will highlight potential for severe liver failure. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-prescription-acetaminophen-products-be-limited-325-mg-dosage-unit
Wang, S., Han, C., Bahk, W., Lee, S., Patkar, A. A., Masand, P. S., & Pae, C. (2018). Addressing the side effects of contemporary antidepressant drugs: A comprehensive review. Chonnam Medical Journal, 54 (2), 101-112. https://doi.org/10.4068/cmj.2018.54.2.101 www.ncbi.nlm.nih.gov/pmc/articles/PMC5972123/
Wiffen, P. J., Derry, S., Bell, R. F., Rice, A. S. C., Tolle, T. R., Phillips, T., & Moore, R. A. (2017). Gabapentin for chronic neuropathic pain in adults (review). Cochrane Database of Systematic Reviews, 6, 1-130. https://doi.org/10.1002/14651858.CD007938.pub4.