This article will provide a brief overview of the assessment, triage, and management of the pediatric patient with a fever.
Course preview
Disclosure Form
Objectives
At the end of this module, the reader should be able to:
- Define pediatric fever.
- Identify the most common causes of pediatric fever.
- Identify appropriate screenings and exam components for a child with a fever.
- Identify appropriate treatment for pediatric fever.
- Identify when pediatric fever is an emergency.
Although the definition of fever has been challenged in recent literature, the current standard definition of a fever in medicine is the elevation of body temperature more than one degree Celsius above “normal” body temperature (Bush, 2018). The standard “normal” body temperature has been defined as 37 Celsius (98.6 Fahrenheit) since the extensive research conducted by Dr. Wunderlich in the 1860s (McElroy & McElroy, 2020). Research of this definition is ongoing, but for the purpose of this article this remains an adequate definition of a fever; it is the same for both children and adults and is defined as at least one standard deviation higher than the average body temperature, i.e., over 38 C or 100.4 F. The exception to this rule is a newborn, up to 28 days old, in which the normal average body temperature is between 37.5 and 38 C; however, a fever in this age group is still defined as a rectal temperature over 38 C (Ward, 2020). The broad and very general physiology of a fever is explained as the resetting of the hypothalamic set point. This triggers vasoconstriction and shunts blood from the periphery to the core, resulting in the conservation of heat, and thus the elevation of body temperature (Bush, 2018).
Pathophysiology and Etiology
As a fever is considered a symptom of disease, and not a disease unto itself, the pathophysiology of fever is manifold. Most fevers are caused by some kind of exogenous pyrogen (literally substances that induce fever) such as bacteria or viruses, but fevers can also be caused by heat, some medications, immunizations, cancers, and autoimmune processes (Bush, 2018). Please note that for the purposes of this article hyperthermia in the setting of heat stroke or heat illnesses will not be discussed and are managed differently. Unless a fever is recurrent, the most common cause of fever in children is infection (Ward, 2020). Viral pathogens are the most common cause of infections in children, whereas, the most common cause of serious bacterial infections in children is a urinary tract infection (UTI). In neonates, the most common bacterial infections are group B strep, E. coli, and Listeria monocytogenes respectively (Joseph et al., 2018). While research demonstrates that there are potential protective and harmful effects of a fever, actual protective effects of a fever in humans have not been confirmed. These conclusions were drawn from animal studies suggesting that the presence of a fever may help stall bacterial growth, but this finding has not been replicated in human studies. Further, the common adage that a fever over 104 ∞F causes brain damage or is associated with worse outcomes has also not been demonstrated outside of animal studies (Ward, 2020).
History, Exam Findings, & Tests
When a child presents with a fever, one of the first history questions should be regarding the child’s immunization status. Children who are not immunized, or those who are not up to date on their immunizations are at much higher risk for bacteremia and sepsis. The duration and severity of the fever should also be noted. Fevers lasting longer than seven days are known as “fevers of unknown origin” and require a different approach than the standard acute fever, which will be discussed separately below (Allen, 2020). Providers should also include questions about the patient’s recent activity level and tolerance, feeding and elimination patterns, and if the parent has witnessed any seizures. The presence and severity of lethargy; irritability; weak, high pitched, or continuous crying; decreased or increased urination with pain; or seizures have been correlated with intermediate to severe risk of serious illness (National Institute for Health and Care Excellence [NICE], 2019). In the neonate, the risk of maternally transmitted infection should also be considered; the history should be expanded to include history of premature rupture of membranes, group B strep status, and history of genital herpes. It should also be determined if the patient has received antibiotics in the last seven days as the risk of an invasive bacterial infection is significantly increased in infants who have recently had antibiotics (Smitherman & Macias, 2020).
In patients over the age of 36 months, evaluation of an initial fever should be symptom focused, as the vast majority of fevers in children of this age group are self-limiting and viral. History should also be focused on acquiring information regarding any associated symptoms in order to narrow down the differential diagnoses. Associated symptoms may include the presence of cough, rash, pain (including location, such as back, abdominal, ear, throat, limb, or joint), restriction of motion in any extremity, and any known exposures and recent travel to endemic areas. In a phenotypically male patient, circumcision status should also be assessed, as UTIs are more prevalent in uncircumcised male patients who are under two years of age in comparison with their circumcised counterparts. The presence of underlying conditions should also be assessed during the history, as diseases such as sickle cell disease, cystic fibrosis, structural abnormalities, and others may predispose patients to certain infections, or place them at a higher risk of rarer causes of infection. Fevers in children over 36 months that were previously healthy, are currently well appearing, and are unable to be linked to a specific source are termed “fever without a source”. This definition applies up to the five-day mark and can occur in up to 40% of cases. As stated above, it is important to remember that the localization of the infectious source may be difficult and warrants further study in this age group as compared to the presence of a simple fever in an older child (Allen, 2020). Further testing and management of fever without a source will be discussed below.
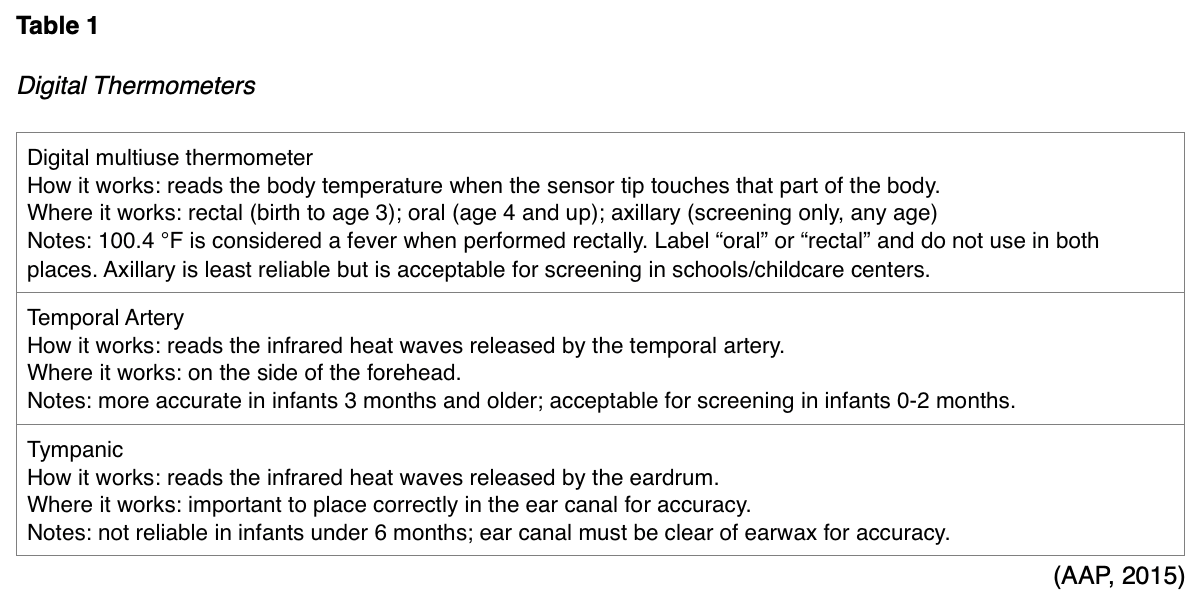
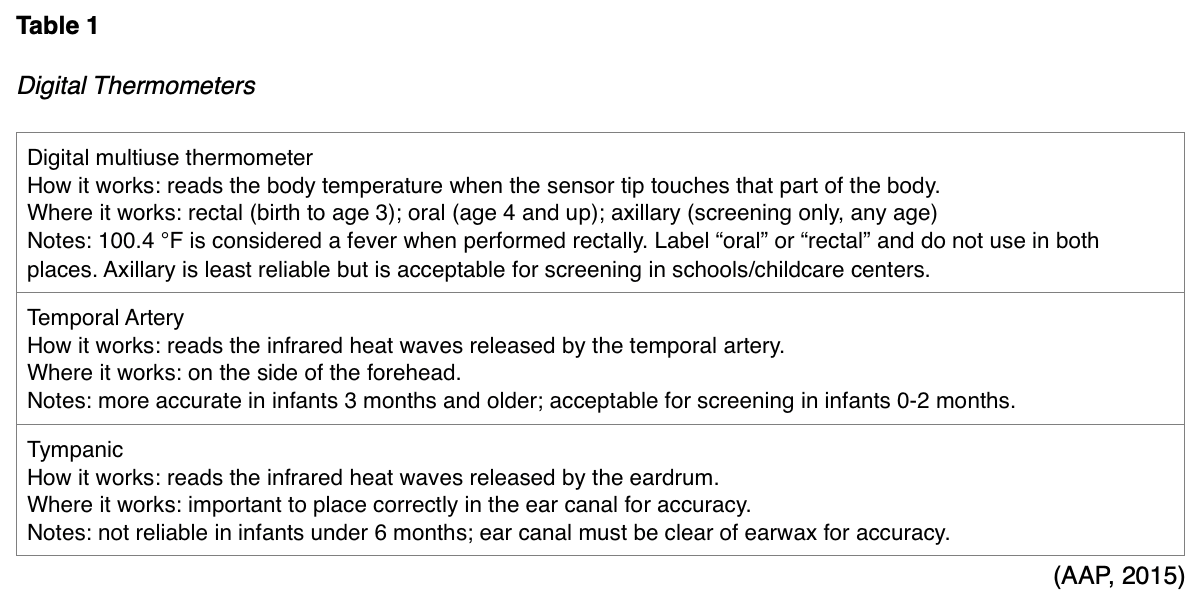
When examining a patient with a fever, the first step is to accurately measure the fever. Fever measurement for outpatient clinical purposes in children three years old and under should always be performed rectally, as peripheral temperatures can measure up to four degrees less than a rectal temperature with poor sensitivity in the detection of a fever in children this young (Joseph et al., 2018). According to the American Academy of Pediatrics (AAP, 2015), rectal temperatures are more accurate, but caution should be exercised to avoid bowel perforation. See Table 1 for more information regarding various options for digital thermometers available.
A comprehensive physical exam should also be performed in order to determine possible sources of infection and accompanying symptoms (Allen, 2020). A full head-to-toe musculoskeletal exam with a focus on infection, including the spine, is important, as is a complete scan for any lymphadenopathy (Oakes, 2017). Previously, the testing and hospitalization of children, especially children under 90 days old, were determined mainly by the severity of the fever. In the 1980s, infants younger than 90 days old who presented with a fever were hospitalized and underwent lumbar puncture and a full sepsis workup. Until recently, little consideration was given to the potential risks involved with such invasive testing in this age group, even when there was a low risk for sepsis (Joseph et al., 2018). Currently, patien
...purchase below to continue the course
ts under three months old should still be evaluated by a provider for any temperature over 38 C or 100.4 F (NICE, 2019; Smitherman & Macias, 2020). However, up-to-date guidelines suggest that risk stratification should be taken into consideration in infants with a fever, and the appearance of the child should be seriously considered along with the level of the temperature. In infants 30 to 60 days old, risk stratification both in the UK and US recommend taking a urinalysis (UA), urine culture (UC), complete blood count (CBC), blood cultures, cerebrospinal fluid (CSF) and chest x-ray (CXR). There is also evidence that C-reactive protein (CRP) and procalcitonin (PCT) levels can assist in determining if the child is high or low risk for invasive bacterial infection. If the child appears well, has a reliable caregiver, and the white blood cell count (WBC), CBC, UA, CSF and CXR are negative, and they are considered low risk (PCT and CRP are within normal limits, or only one is mildly elevated), they may be discharged under the observation of a caregiver with a follow-up appointment within 24 hours. Further treatment should be initiated as premised on the results of the blood cultures (Joseph et al., 2018; NICE, 2019). Furthermore, infants from 60 to 90 days old are now considered to be low risk for bacteremia and meningitis; therefore, their evaluation can be slightly more focused. It is still necessary to get a UA/UC, CBC and blood cultures; however, it is only necessary to get a CXR if the infant has tachypnea, tachycardia, wheezing, or a cough, and a lumbar puncture is only indicated if the child appears toxic or is irritable (Joseph et al., 2018). If these tests are negative and the patient’s PCT and CRP levels are within normal limits, then they may also be discharged home with a caregiver and a follow-up in 24 hours. Empiric antibiotics and hospitalization are only indicated in high risk infants, such as those with an elevated CRP and/ or PCT level (Joseph et al., 2018).
Various methods have been developed in an effort to standardize this stratification process for infants. The “Step by Step” method was validated by Gomez et al. (2016) based on infants who were 90 days old or younger across 11 pediatric emergency centers in Europe. This method places patients into the category of high risk, requiring hospitalization and empiric antibiotics, if any of the following four conditions are met:
1. Is the child ill-appearing? The Pediatric Assessment Triangle may be useful to determine ill versus well-appearing, based on:
- Appearance: the child’s tone, interactiveness, consolability, look or gaze, and speech or cry.
- Work of breathing: the degree to which the child is working in order to oxygenate and ventilate, such as stridor, grunting, wheezing, abnormal positioning, retractions, or flaring of the nostrils on inspiration.
- Circulation to the skin: the color and color pattern of the skin and mucous membranes, noting pallor, cyanosis, or mottling (Fernandez et al., 2017; Gomez et al., 2016).
2. Is the child 21 days old or less?
3. Does the child have leukocyturia (urine test positive for white blood cells)?
4. Is the child’s PCT above or equal to 0.5 ng/mL?
If the answer to any of the above questions is “yes”, then the child should be considered high risk and appropriate management steps should be taken immediately. If all of the above queries are negative, but the child has a CRP that is greater than 20 mg/L or an absolute neutrophil count above 10,000 cells/mm3, they can be considered intermediate risk. Otherwise, if the answers to all of the above is “no”, then the child can be categorized as low risk with relatively little chance of invasive bacterial infection underlying the fever (Gomez et al., 2016).
In patients who are three to 36 months old, evaluation becomes less stratified, as even a severely elevated temperature in children of this age range may not indicate a severe infection. Children between three and 36 months of age with a fever over 102.2 F should be evaluated by a provider and should be managed based on their appearance (Allen, 2020). In fully immunized children, the incidence of bacteremia is less than 1%; despite this statistic, a toxic appearing child, or a child with unstable vital signs, should be managed as if they have sepsis. In well-appearing children, immunization status is the determining factor for the intensity of the work-up required. In a child that is unimmunized or only partially immunized, without an obvious source of infection, who presents with a fever over 102.2 F, WBC, CBC and serum PCT levels should be drawn. Patients in this demographic group with an elevated PCT level or WBC should have blood cultures drawn, and if the WBC is greater than 20,000, a CXR should also be performed. All children should have a UA/UC done if they have symptoms of a UTI, have had a recent UTI, have genital abnormalities, are uncircumcised males under the age of twelve months, or are females under the age of 24 months. Patients older than 36 months with a fever and focal symptoms or who do not appear otherwise well should also be evaluated by a provider (Allen, 2020). In these children, the ordering of lab values and tests should be based on exam findings and accompanying symptoms (Ward, 2020). Systemic inflammatory response syndrome (SIRS) and sepsis should be considered when a child over 36 months has a fever over 101.3 F with tachycardia, tachypnea, or leukocytosis. Of note, SIRS and sepsis may also be considered in the absence of a fever if the child has any combination of tachycardia, tachypnea or leukocytosis (Pomerantz & Weiss, 2020).
Treatment, Management and Medication
The treatment of a fever is recommended in children who have underlying conditions that increase metabolism, have had major head trauma, are post-cardiac arrest, are in shock, or have fluid or electrolyte alterations. Treatment of a fever has not been shown to decrease adverse events in otherwise healthy children. The ultimate goal of fever treatment in these patients is simply to increase the child’s comfort level, and possibly to help prevent fluid loss (Ward, 2020). Fever in children is typically treated with antipyretic agents, such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin). Ibuprofen (Advil, Motrin) is the most effective antipyretic in children, and has also been shown to reduce pain more effectively than acetaminophen (Tylenol) (Joseph et al., 2018). Sources differ on the matter, but UpToDate continues to recommend acetaminophen (Tylenol) as the first line antipyretic for children despite the superior results with ibuprofen (Advil, Motrin) due to its longer and more researched safety history (Ward, 2020). There may be an increased risk of kidney injury in the setting of ibuprofen (Advil, Motrin) in a febrile child who is dehydrated; however, ibuprofen (Advil, Motrin) is preferred in children with liver failure. The combination of ibuprofen (Advil, Motrin) and acetaminophen (Tylenol) has also been shown to be more effective in reducing fever but most studies have failed to prove that this is clinically significant. Sources agree that the combination of these agents is not recommended due to the increased risk of dosage error and possibly increased risk of kidney or liver injury (Joseph et al., 2018; Ward, 2020). The decision to treat fever in an otherwise healthy child should be based on the parent and child’s wishes to reduce discomfort. A downside of treating fever with antipyretic agents is that it affects the ability of the provider to assess the duration of the temperature and may delay the identification of the underlying etiology (Ward, 2020).
Empiric antibiotics are indicated for the symptoms of fever alone in the treatment of children under 90 days old who are determined to be at high risk based on the criteria discussed above. In infants younger than 30 days old, recommended empiric antibiotics include ampicillin (Unasyn) 50 mg/kg IV or gentamycin (Garamycin) 2.5 mg/kg IV. For infants between 30 and 60 days old who are determined to be high risk but with normal CSF analysis, ampicillin (Unasyn) 50 mg/kg IV plus ceftriaxone (Rocephin) 50 mg/kg IV is the recommended empiric antibiotic regimen. If the CSF results are abnormal, the dosage of ampicillin (Unasyn) remains the same, but ceftriaxone (Rocephin) increases to 100 mg/kg IV. For fully vaccinated children between 90 days and 36 months, it is most likely that a fever would be caused by a virus and empiric antibiotics are not advised. However, if the child is high-risk, ceftriaxone (Rocephin) is the empiric antibiotic of choice (Joseph et al., 2018). Empiric antibiotics are not warranted in children over 36 months of age unless shock or sepsis is suspected. If SIRS or sepsis is suspected, children are to be resuscitated and cultured (blood and urine cultures at least, but potentially including CSF culture per facility protocol) first. Further treatment of these children should be managed in a pediatric intensive care unit and is beyond the scope of this article (Pomerantz & Weiss, 2020). Initiation of antibiotic treatment not in the setting of sepsis or SIRS should be based on clinical findings. Empiric antibiotics in these instances are not warranted without an identified source of infection, and it is important to remember that fever alone is not an indication for the prescription of antibiotics (NICE, 2019). For parents of children over three years old, extensive education should be provided that antibiotics are not indicated without an identified source of infection to help with understanding (Joseph et al., 2018; Ward, 2020)
Fever of Unknown Origin
The management of a persistent fever in a child over 101 ∞F that has been present for longer than seven days is different than a higher fever present for a shorter amount of time as discussed above. Fevers meeting these criteria with no identified source after initial evaluation are called fevers of unknown origin (FUO). When evaluating a child with this type of fever, it is crucial to repeat an extensive history. Often, FUOs are common diseases presenting abnormally. Ask how frequently the child’s temperature is being taken, how, and about any associated symptoms. Possible exposures should be reviewed including travel history, insect or animal bites or scratches, previous illnesses, sick contacts, and recent laboratory tests as well as a comprehensive physical examination should be repeated. Labs should include CBC, comprehensive metabolic panel, UA/UC, blood cultures, erythrocyte sedimentation rate, and CRP. Infection, connective tissue disease, and malignancy are the three most common causes of FUO in children, with leukemia and lymphoma cited as the top two contributing malignancies. It should also be noted that FUOs often resolve spontaneously without the causal etiology ever being identified. Further testing and imaging are determined by the history, physical exam, and accompanying symptoms. A comprehensive list of underlying etiologies for FUOs is beyond the scope of this article, but the provider should review neoplasms in children, Kawasaki disease, juvenile idiopathic arthritis, cat scratch fever, and autoimmune diseases in children. A gap of a few days without any fever may indicate two consecutive but separate viral infections. An additional option for testing a child with FUO is a viral polymerase chain reaction (PCR) panel, which can help streamline the work-up and identify common viral pathogens such as adenovirus, influenza, and respiratory syncytial virus (RSV). A CXR can be done if pneumonia is suspected. Cytomegalovirus and Epstein-Barr virus may need to ruled out. If the patient’s CBC indicates a high level of bands (immature WBCs), the provider may consider checking their lactate dehydrogenase, uric acid, and ferritin levels to rule out an oncologic process. A peripheral smear and a referral to a pediatric oncologist should be considered if the above are largely abnormal, or in the context of reports of night sweats or weight loss. If a rheumatologic etiology is suspected, an antinuclear antibody and complement level as well as a referral to a pediatric rheumatologist should be considered. Most advise against a trial of empiric antibiotics in these patients (Oakes, 2017; Palazzi, 2020).
Febrile Seizures
Febrile seizures are fairly common; they can occur in pediatric patients and are associated with fever without other intracranial abnormalities or infections. Children with a genetic predisposition can be more susceptible to febrile seizures. Viruses, bacteria, or vaccines can be causative agents of febrile seizures. Febrile seizures can be classified into three groups: simple, complex, and symptomatic. Simple febrile seizures last less than 15 minutes, are generalized, and occur once within a 24-hour period with no focal component. Complex febrile seizures last more than 15 minutes, have a focal component, and occur more than once in a 24-hour period. A symptomatic febrile seizure is a seizure occurring due to a fever in a child that has a preexisting neurological abnormality. Acute management of the febrile seizure is to maintain a patent airway, ensure effective breathing with oxygen therapy as needed, protect from injury, place in semi-prone position, and loosen clothing. The fever should be treated as noted above, and according to the duration and severity. Rectal diazepam (Valium) can be given for any seizure lasting over five minutes in length; IV diazepam (Valium), lorazepam (Ativan), or phenobarbital is indicated for any seizure lasting longer than 15 minutes (Schellack & Schellack, 2019).
Future Research/Directions
As discussed in the introduction of this article, the current definition of a fever has been in use since the 1860s; however, a 2018 study by Dr. Hausmann and associates suggests that the average human body temperature may be lower than our current understanding. His research suggests that the definition of a “fever” as that of a body temperature in the 99th percentile of normal body temperatures, may be closer to 37.5 C (99.5 F) or higher (2018). Further data analysis of other studies that have large volumes of patient average body temperatures have been preliminarily determined to show that humans’ average body temperature does seem to be steadily declining since the time of Dr. Wunderlich (McElroy & McElroy, 2020). Despite the recent study by Dr. Hausmann receiving a lot of attention in the press, it has not currently been replicated, and children were excluded from the data. For these reasons, it is too early at this time to apply it to current standards of practice, or to extrapolate that there is a need to change the current guidelines for the treatment or evaluation of fever. Dr. Hausmann’s research does suggest that the use of smartphones may be an adequate way to measure temperature in the future, but until this study can be replicated in children, this is still far from being an appropriate way to clinically measure an accurate temperature in children (Hausmann et al., 2018).
References
American Academy of Pediatrics. (2015). How to take a child’s temperature. https://www.healthychildren.org/English/health-issues/conditions/fever/Pages/How-to-Take-a-Childs-Temperature.aspx
Allen, C. A. (2020). Fever without a source in children 3 to 36 months of age: Evaluation and management. UpToDate. www.uptodate.com
Bush, L. M. (2018). Fever. Merck manual professional version. https://www.merckmanuals.com/professional/infectious-diseases/biology-of-infectious-disease/fever
Fernandez, A., Benito, J., Mintegi, S. (2017). Is this child sick? Usefulness of the Pediatric Assessment Triangle in emergency settings. Jornal de Pediatria (93)1, 60-67. https://doi.org/10.1016/j.jped.2017.07.002
Gomez, B., Mintegi, S., Bressan, S., Dalt, L. D., Gervaix, A., & Lacroix, L. (2016). Validation of the “step-by-step” approach in the management of young febrile infants. Pediatrics, 138(2). https://doi.org/10.1542/peds.2015-4381
Hausmann, J. S., Berna, R., Gujral, N., Ayubi, S., Hawkins, J., Brownstein, J. S., & Dedeoglu, F. (2018). Using smartphone crowdsourcing to redefine normal and febrile temperatures in adults: Results from the feverprints study. Journal of General Internal Medicine, 33(12), 2046–2047. https://doi.org/10.1007/s11606-018-4610-8
Joseph, J., Nguyen, N., Olsen, D., & Ung, L. (2018). Special report: A better approach for pediatric fever-finally. Emergency Medicine News, 40(7), 12–14. https://doi.org/10.1097/01.eem.0000542251.15712.47
McElroy, S., & McElroy, J. (2020). Sawbones: Body temperature [Audio Podcast]. https://maximumfun.org/episodes/sawbones/sawbones-body-temperature/.
National Institute for Health and Care Excellence. (2019). Fever in under 5s: Assessment and initial management. (UK); (NICE Guideline, No. 143.) https://www.ncbi.nlm.nih.gov/books/NBK552086/
Oakes, K. (2017). How to have a rational approach to the FUO work-up. Pediatric News. https://www.mdedge.com/pediatrics/article/148842/infectious-diseases/how-have-rational-approach-fuo-work
Palazzi, D.P. (2020). Fever of unknown origin in children: Evaluation. UpToDate. www.uptodate.com
Pomerantz, W. J. & Weiss, S. L. (2020). Systemic inflammatory response syndrome (SIRS) and sepsis in children: Definitions, epidemiology, clinical manifestations, and diagnosis. UpToDate. www.uptodate.com
Schellack, N. & Schellack, G. (2019). An overview of the management of fever and its possible complications in infants and toddlers. Prof Nurs Today, 23(1), 25-33. https://www.semanticscholar.org/paper/An-overview-z21,of-the-management-of-fever-and-its-in-Schellack-Schellack/46c29a25bac8acc96105ca3caa69f5071e1acad3
Smitherman, H. F. & Macias, C. M. (2020). Febrile infant (younger than 90 days of age): Outpatient evaluation. UpToDate. www.uptodate.com
Ward, M. A. (2020). Fever in infants and children: Pathophysiology and management. UpToDate. www.uptodate.com