About this course:
The purpose of this module is to augment nursing knowledge of prostate cancer by providing an overview of the condition, its risk factors, clinical features, common subtypes, treatment modalities, and the most common side effects of treatment to enhance nursing practice, patient education, and clinical outcomes.
Course preview
This module aims to augment nursing knowledge of prostate cancer by providing an overview of the condition, its risk factors, clinical features, common subtypes, treatment modalities, and the most common side effects of treatment to enhance nursing practice, enrich patient education, and improve clinical outcomes.
By the completion of this learning activity, the nurse should be able to:
- discuss the epidemiology of prostate cancer in the US and the pathophysiology of the disease
- identify the risk factors, signs and symptoms, primary classifications, and subtypes of prostate cancer
- summarize prostate cancer screening guidelines and the meaning of active surveillance and “watchful waiting” as core components of patient education
- explore prostate cancer treatment modalities, including surgery, radiation, hormonal treatment, antiandrogen therapy, chemotherapy, and immunotherapy
- describe the most common side effects and monitoring parameters of systemic treatments, highlighting the pertinent aspects of patient education
Epidemiology
Aside from skin cancer, prostate cancer is the most common cancer among men in the US. According to the American Cancer Society (ACS, 2020), one in nine men will be diagnosed with prostate cancer during his lifetime. In 2020, there will be an estimated 191,930 new diagnoses and 33,330 deaths from prostate cancer. It is primarily an aging disease, most commonly diagnosed in men 65 years of age and older. According to the Centers for Disease Control and Prevention (CDC, 2020), 13 out of every 100 men will be diagnosed, and about 2 to 3 will die from prostate cancer. Prostate cancer serves as the second leading cause of cancer-related deaths in the US. African American men have the highest incidence of prostate cancer worldwide and are twice as likely to die from prostate cancer than men of other ethnic backgrounds. Despite these numbers, most prostate cancers tend to be slow-growing, low-grade, and nonlethal. Survival rates vary depending upon the disease’s severity and the extent of the disease. At the time of diagnosis, prostate cancer has a nearly 100% survival rate in the early stages but declines to approximately 30% for patients with advanced disease. Currently, there are more than 3.1 million prostate cancer survivors in the US. Since early diagnosis improves health outcomes and reduces morbidity and mortality associated with the disease and its treatment, nurses must become attuned to the potential warning signs and symptoms to help facilitate a timely diagnosis (ACS, 2020; Cadet et al., 2019).
Pathophysiology
The prostate gland is part of the male reproductive system and is comparable in size to a walnut. It is located at the base of the penis beneath the bladder and anterior to the rectum. As demonstrated in Figure 1, the prostate surrounds the urethra and has ducts opening into the prostatic portion of the urethra. It is comprised of both muscular and glandular tissue (Leslie et al., 2020). The prostate gland’s primary function is to form and secrete a slightly alkaline prostatic fluid to carry sperm. This fluid also helps sperm survive in the female reproductive tract’s acidic environment. The prostate contracts rhythmically to push the prostate fluid into the urethra, and the fluid leaves the body out through the penis’ tip during ejaculation (McCance & Heuther, 2019).

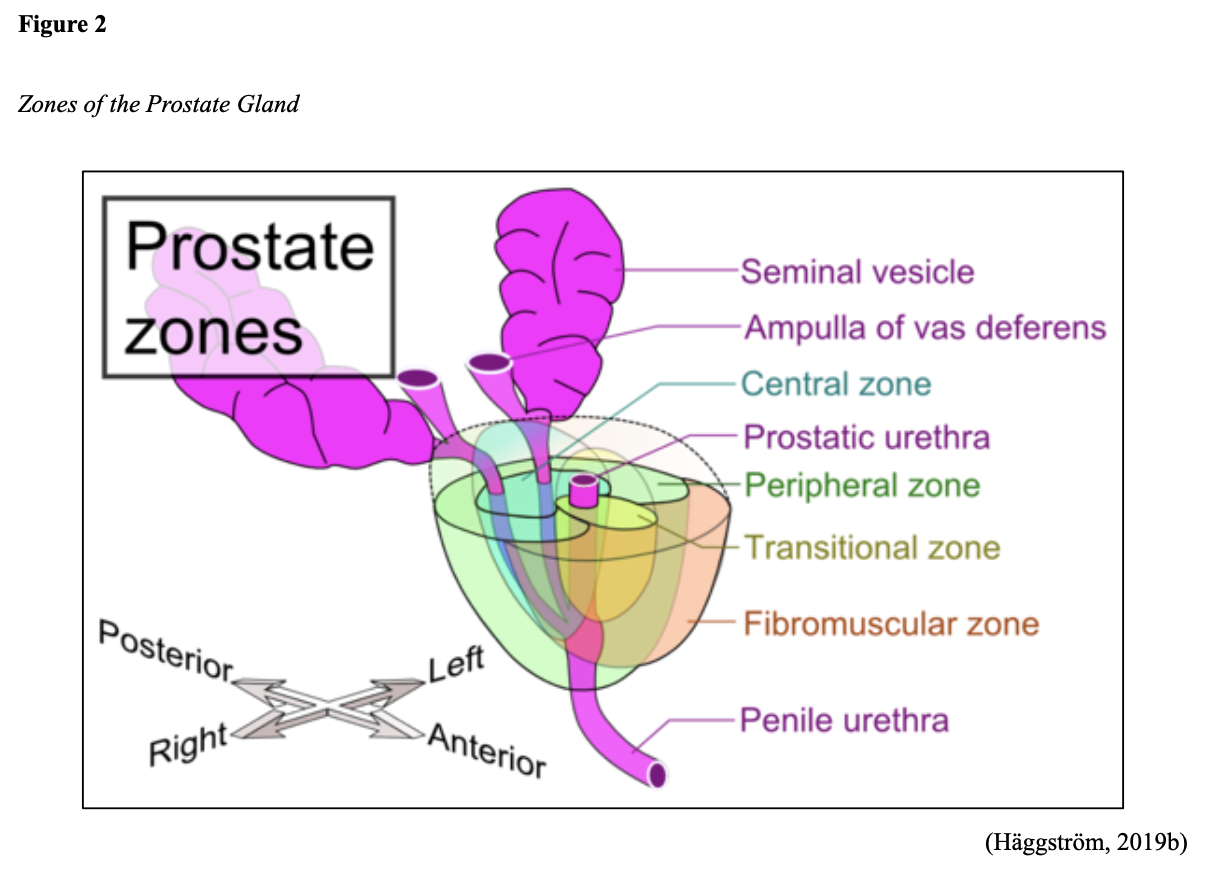
The prostate gland includes three major sections that are important to understand with regards to the development of prostate cancers; the peripheral zone (PZ), central zone (CZ), and transitional zone (TZ). As demonstrated in Figure 2, the PZ comprises the prostate’s largest surface area; 60-75% of cancers arise here. Anatomically, the PZ is positioned at the posterior aspect of the gland, closest to the rectal wall. The CZ surrounds the ejaculatory ducts and makes up about 25% of the gland. While less than 5% of prostate cancers originate within this region, these cancers are more aggressive and pose a higher likelihood of invasion into the seminal vesicles. The TZ surrounds the urethra at the connection point with the prostate gland and is relatively small but grows larger with age. It is responsible for up to 20% of prostate cancers but is more commonly associated with benign prostatic hyperplasia (BPH, or prostate gland enlargement). While the fibromuscular zone is labeled in Figure 2, it is not truly a fourth zone. This region denotes the part of the prostatic urethra that is not enclosed within the PZ, protected by a thick, non-glandular tissue called the fibromuscular stroma (Wang et al., 2018).
Androgens (male sex hormones) are required for the formation, growth, and optimal functioning of the prostate gland and are regulated by the hypothalamic-pituitary-gonadal (HPG) axis. The HPG refers to the complex interplay between the male endocrine system, particularly the hypothalamus, pituitary gland, and gonadal glands. This process is summarized in Figure 3. The two most abundant androgens in males include testosterone and dihydrotestosterone (DHT), with testosterone serving as the primary circulating androgen. These hormones play pivotal roles in prostate cancer growth and treatment (Clavijo & Hsiao, 2018).
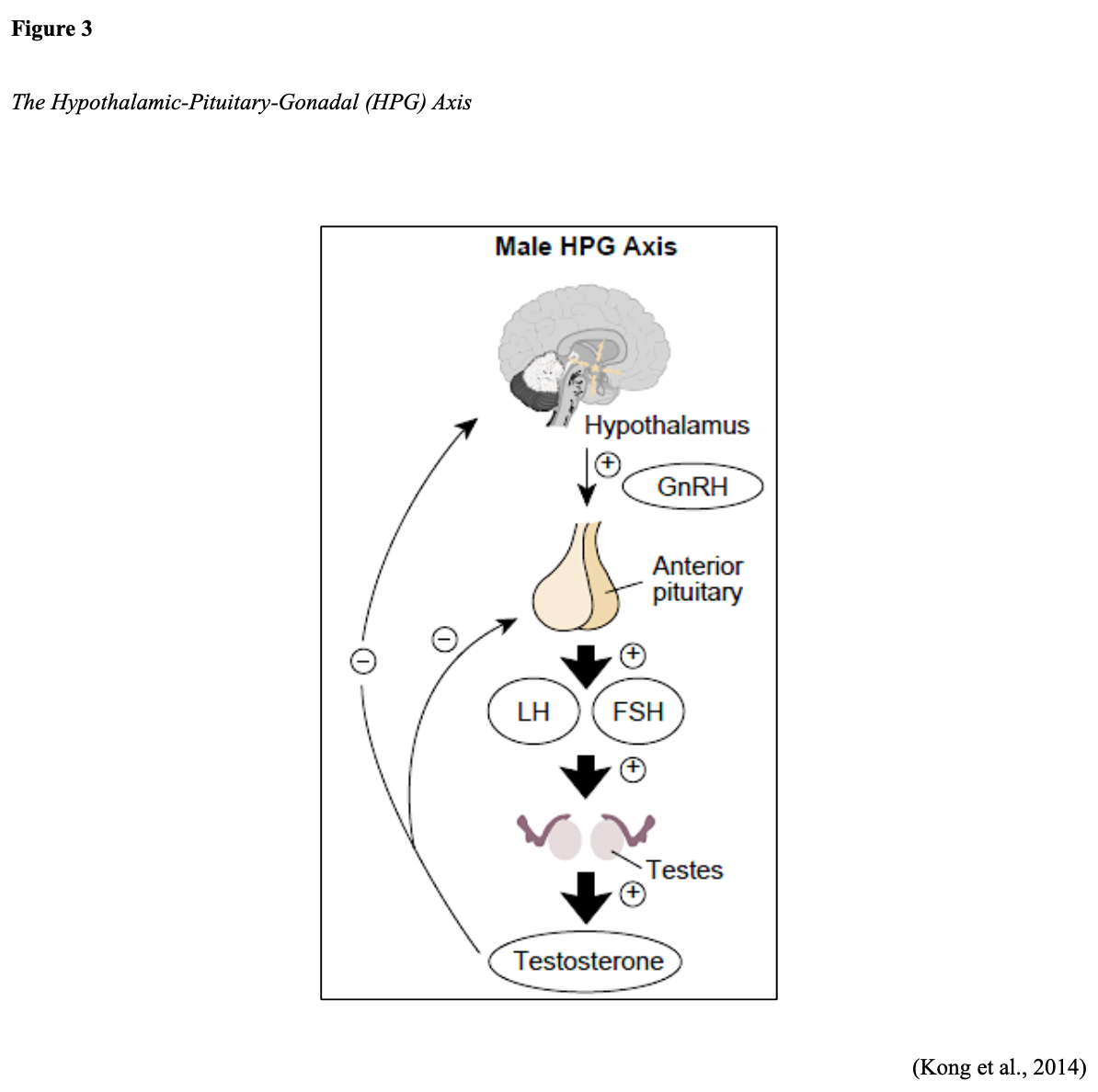
The production of androgens is initiated by the hypothalamus. The hypothalamus creates and releases gonadotropin-releasing hormone (GnRH), also called luteinizing hormone-releasing hormone (LHRH). GnRH prompts the pituitary gland to generate and secrete luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Figure 4 compares this process in males and females. In males, testosterone production is regulated by luteinizing hormone (LH) and LHRH. LH acts on specific cells in the testes to produce testosterone; additional androgens are produced by the adrenal glands (Clavijo & Hsiao, 2018; Fujita & Nonomura, 2019).

Androgens are taken up by prostate cells, where they bind to the androgen receptor (AR) directly or are converted to DHT. DHT is found predominantly in prostate tissue and has a greater affinity for binding to the AR than testosterone. The AR is a steroid receptor transcriptional factor that mediates the actions of both testosterone and DHT. It has a similar structure and functionality to that of the estrogen receptor (ER) that fuels estrogen-based cancers, such as breast cancer in females. Androgens can fuel the growth of prostate cancer by binding to and activating the AR, which subsequently stimulates the overexpression of specific genes that trigger cell growth. Therefore, the AR serves a central role in prostate cancer, particularly castration-resistant prostate cancer (CRPC; Clavijo & Hsiao, 2018; Fujita & Nonomura, 2019).
Prostate Cancer Subtypes
All prostate cancers arise from glandular epithelial cells, which is the most abundant cell type within the prostate gland. More than 95% are adenocarcinomas, which are cancers that form in the mucus-producing glandular cells. Approximately 5% are transitional cell carcinomas, and less than 1% are squamous cell carcinomas. The three major classifications of prostate cancer are summarized in Table 1. While these three classifications can be mutually exclusive diseases, many patients will transition from hormone-sensit
...purchase below to continue the course

Risk Factors
All men are at risk for prostate cancer; however, older age, African American race, and family history of prostate cancer are the most well-cited risks for the condition (US Preventative Services Task Force [USPSTF], 2018). African American men tend to develop prostate cancer at younger ages and endure a more aggressive clinical course than other men. Family history is a significant risk factor, as up to 10% of all prostate cancers are hereditary. Men who have a first-degree relative with prostate cancer (i.e., father or brother) are twice as likely to develop prostate cancer as those with no family history. Men who have two or more first-degree relatives with prostate cancer are at a five-fold increased risk for prostate cancer (CDC, 2020). Other possible risk factors with weaker associations, and less evidence include diets high in saturated fat and obesity; tobacco use is associated with a higher risk of mortality (USPSTF, 2018).
Genetic Mutations
Everyone has BRCA1 and BRCA2 genes. These genes function as tumor suppressor genes that work to prevent cancer by regulating specific cells’ growth and division under physiologic conditions. However, mutations in these genes prevent them from working correctly, thereby increasing cancer development’s propensity. Mutations in the BRCA1/BRCA2 genes are inherited in an autosomal dominant pattern. One copy of the mutated gene in each cell is sufficient to increase the risk of developing cancer. The altered gene can be inherited from either the male or female parent, as each child of a parent with a BRCA1 or BRCA2 mutation has a 50% chance of inheriting the same gene mutation. BRCA mutations occur most frequently within the Ashkenazi Jewish population. Most commonly known for increasing the risk of breast and ovarian cancers in women, mutations in the BRCA2 gene also increase the risk for aggressive prostate cancer in men. BRCA2 mutations are associated with earlier-onset, higher rates of lymph node involvement, distant metastasis at diagnosis, and higher mortality rates. Some studies describe the presence of a BRCA2 mutation as an independent prognostic factor for poorer outcomes in prostate cancer (Hartzfeld et al., 2016). Data from the IMPACT study, which followed 2,900 men with annual PSA screenings for three years, demonstrated that BRCA2 mutation carriers had the most significant risk of developing cancer. Their findings revealed a 5.2% risk in patients with BRCA2 mutations, 3.4% risk in those with BRCA1 mutations, and a 2.7% risk in men who tested negative for both BRCA1/BRCA2 mutations (Page et al., 2019).
Genetic and Molecular Biomarker Analysis
Due to recent advancements in technology and targeted treatment modalities, the National Comprehensive Cancer Network (NCCN) guidelines recommend that patients with advanced or metastatic prostate cancer undergo specialized genetic and molecular biomarker analysis. These specific analyses evaluate for the presence of homologous recombination gene mutations (HRRm) and microsatellite instability-high (MSI-H) or mismatch repair deficiency (dMMR). HRR gene mutations can increase the risk of developing more aggressive prostate cancer, and the most common include BRCA1/2, ATM, and CDK12. HRR gene mutations compromise tumor cells’ ability to correct the DNA damage through the loss of HRR. This mechanism can lead to an increased reliance on poly ADP-ribose polymerase (PARP)-mediated DNA repair pathways for survival, thereby opening up the possibility of targeted treatment pathways, such as the use of PARP-inhibitors (i.e., Olaparib [Lynparza]) in patients with advanced BRCA2-mutant prostate cancer. The presence of MSI-H or dMMR has clinical implications with regards to the potential use and benefit of immunotherapy (specifically, immune checkpoint inhibitors) in several types of cancers. MSI-H or dMMR are relatively uncommon in prostate cancer, with one study demonstrating a prevalence rate of only 3.2%. These mutations pose the potential for durable therapeutic responses to anti-programmed cell death protein 1 (PD-1)/programmed cell death ligand 1 (PD-L1) treatment, such as pembrolizumab (Keytruda), which will be discussed later within the treatment section of this module (Reichert et al., 2019).
Men with a genetic mutation in the HOXB13 gene may also be at increased risk for prostate cancer. HOX proteins are transcription factors that serve various roles in tissue differentiation of developing embryos, organogenesis, and contribute to several other cellular processes such as proliferation, differentiation, apoptosis, and migration (Brechka et al., 2017). The HOXB13 protein also acts as a tumor suppressor, which means that it keeps cells from growing and dividing too quickly or uncontrolled. While all individuals have two copies of the HOXB13 gene, mutations in one copy of the HOXB13 gene are associated with an increased risk for early-onset prostate cancer and CRPC. Research suggests that mutations in this gene impair the protein’s tumor suppressor function, resulting in uncontrolled cellular proliferation and cancer development (US National Library of Medicine, 2020). However, the clinical data is not nearly as robust as with BRCA2 mutations, and there remain numerous gaps in current understanding of how the HOXB13 gene confers increased risk in prostate cancer (Brechka et al., 2017).
Signs and Symptoms
Early prostate cancer generally does not cause pain, sexual dysfunction, or other signs; in most cases, affected men exhibit no symptoms. As the tumor grows or spreads into surrounding structures, patients may develop uncomfortable urinary symptoms, such as difficulty starting or stopping the flow of urine, a feeling of not being able to empty the bladder, or pain with ejaculation. However, many of these symptoms can also occur due to BPH, a common condition affecting a large percentage of men as they age. An enlarged prostate gland can induce uncomfortable urinary symptoms, including bladder, urinary tract, or kidney problems (Mayo Clinic, 2019). With advanced disease, symptoms are often the consequence of cancer metastasizing to other areas in the body. Based on cancer spread patterns, the most common symptoms include bone pain, dysuria, hematuria, flank pain, anemia, fatigue, weight loss, and weakness. (Leslie et al., 2020).
Early Detection and Screening
One of the most powerful tools that nurses have is their ability to develop deep professional relationships with patients and their family members. Nurses are in a unique position to convey the importance of cancer prevention across healthcare settings. To effectively counsel patients on prostate cancer risk reduction, nurses must understand the basis for prostate cancer screening and possess adequate knowledge of evidence-based guidelines and screening recommendations. Nurses can help patients comprehend their options, set realistic expectations, and understand the risks and benefits of screening to make informed decisions. Nurses must also recognize and understand the various features that place patients at increased risk for the disease to ensure they are counseled appropriately (Kahl, 2018). Given the lack of warning signs and symptoms in early prostate cancer, the first findings raising clinical suspicion for the disease are often identified on routine health screenings, such as serum protein (prostate-specific antigen [PSA]) or abnormalities on the digital rectal exam (DRE; Leslie et al., 2020).
PSA
PSA is a protein generated only by the prostate gland and is a tumor marker for prostate cancer. Tumor markers are substances produced by cancer or by the body’s response to cancer’s presence but are also made in smaller quantities by healthy cells, making them nonspecific. The PSA blood test measures the amount of this protein in the blood. A PSA level of less than 4.0 ng/mL was previously considered normal, and higher than 4.0 ng/mL was abnormal, warranting a biopsy to evaluate prostate cancer. Over time, these recommendations have changed. The American Board of Internal Medicine (ABIM, 2020) cites the PSA as having “no specific normal or abnormal level” in their 2020 Laboratory Test Reference Ranges (p.9). The current understanding is that the PSA level varies over time and rises slowly with age, even in the absence of prostate abnormalities (Cadet et al., 2019).
To provide effective counseling to patients undergoing the PSA screening test, nurses must be aware of conditions and medications that can skew the accuracy of the results. The PSA can be elevated in benign conditions such as BPH, prostatitis (infection or inflammation of the prostate gland), or due to specific urologic procedures. Ejaculation, riding a bicycle, or strenuous exercise can induce a transient rise in the PSA for a short time (Leslie et al., 2020; NCI, 2017). Nurses should also perform a thorough review of all medications the patient is currently prescribed, as several agents can inadvertently lower the PSA, leading to false-negative results. For example, commonly prescribed medications for BPH such as 5-alpha-reductase inhibitors or dihydrotestosterone blockers (i.e., finasteride [Proscar] and Dutasteride [Avodart]) can decrease the PSA by approximately 50% (NCCN, 2020).
DRE
As demonstrated in Figure 5, the DRE allows for direct palpation of the PZ region, the most common site of prostate cancer, to assess for lumps, nodularity, or abnormalities that might suggest cancer (ACS, 2019b). Despite its continued use in clinical practice, research has demonstrated that the DRE carries a low specificity and sensitivity for detecting early prostate cancer. In 2018, the USPSTF removed the DRE from its prostate cancer screening guidelines.

Controversies Over Prostate Cancer Screenings
Screening for prostate cancer is routinely performed throughout the US, but its benefit and value is controversial. While it has been the subject of much criticism over the last few decades, it remains unclear if the benefits of prostate cancer screening outweigh the risks for most men. While prostate cancer screenings may lead to earlier diagnosis and treatment, this does not correlate with improved survival (Smith et al., 2019). A major shortcoming of prostate cancer screening is the questionable value of the information received, provoking discrepancies regarding its significance. For men whose prostate cancer is detected by screening, it is impossible to predict who will benefit from treatment. PSA specificity and sensitivity are low, and screening is subject to high false-positive rates. A false-positive entails an abnormal PSA level but no detectable prostate cancer, whereas a false-negative is characterized by a normal PSA level despite the presence of cancer. Further, the PSA test has been criticized for flagging too many slow-growing cancers and subjecting patients to invasive procedures, interventions, treatments, and treatment side effects, when cancer may never have posed a risk to the patient during their lifetime (Cadet et al., 2019; Leslie et al., 2020).
Prostate Cancer Screening Guidelines
The current consensus from the USPSTF, NCCN, and ACS evidence-based screening guidelines is that the decision to perform PSA screening tests should be an individual one. Healthcare professionals are encouraged to discuss the pros and cons of screening patients and engage in shared decision-making before deciding upon screening. This allows men to determine if screening is right for them and strives to reduce prostate cancer’s overdiagnosis and overtreatment. Given the well-cited controversies over prostate cancer screenings, there are a few discrepancies between the three guidelines; however, all classify African Americans or those with a first-degree relative with prostate cancer as high-risk. To enhance nursing knowledge when counseling patients, Table 2 provides a summary of prostate cancer screening guidelines according to each organization (ACS, 2019b; NCCN, 2020; USPSTF, 2018).

Diagnosis and Classification
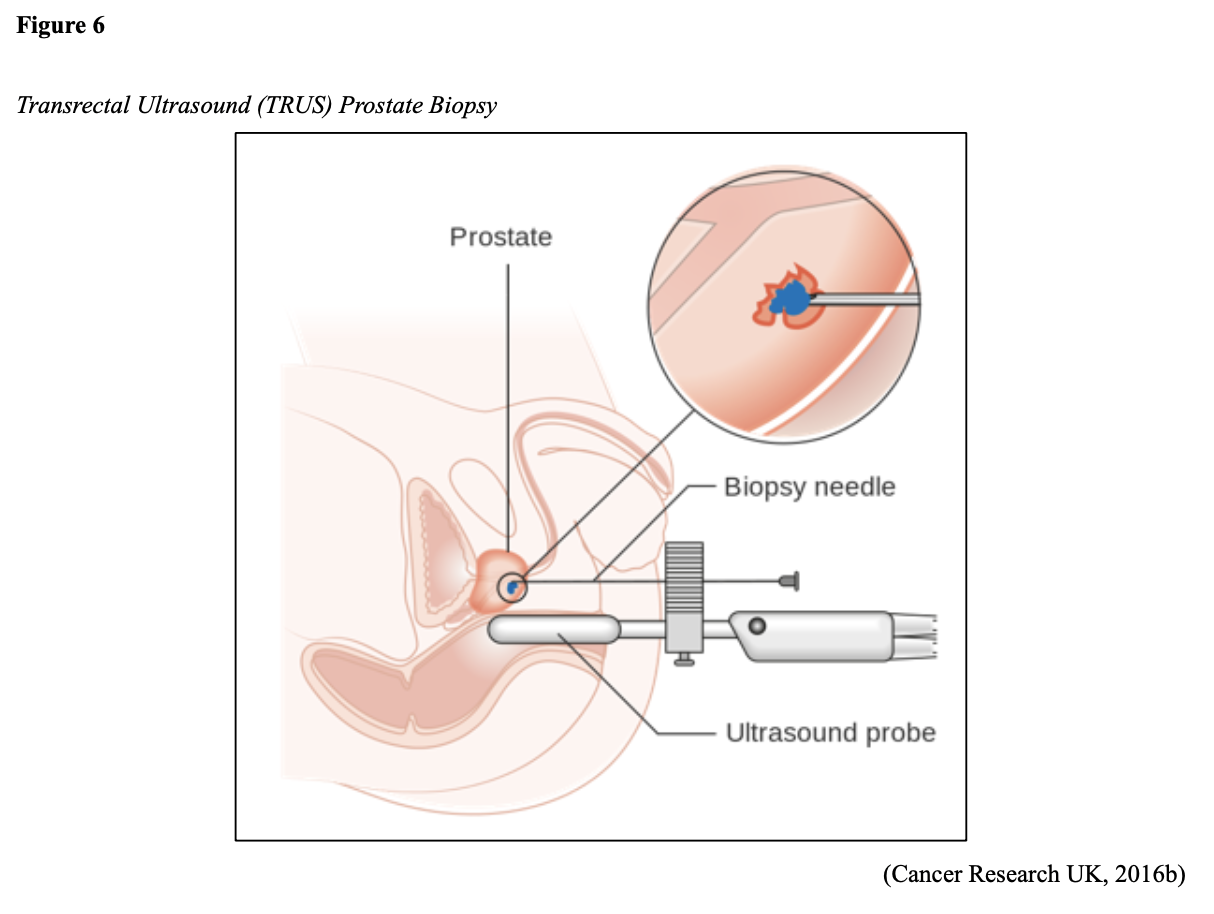
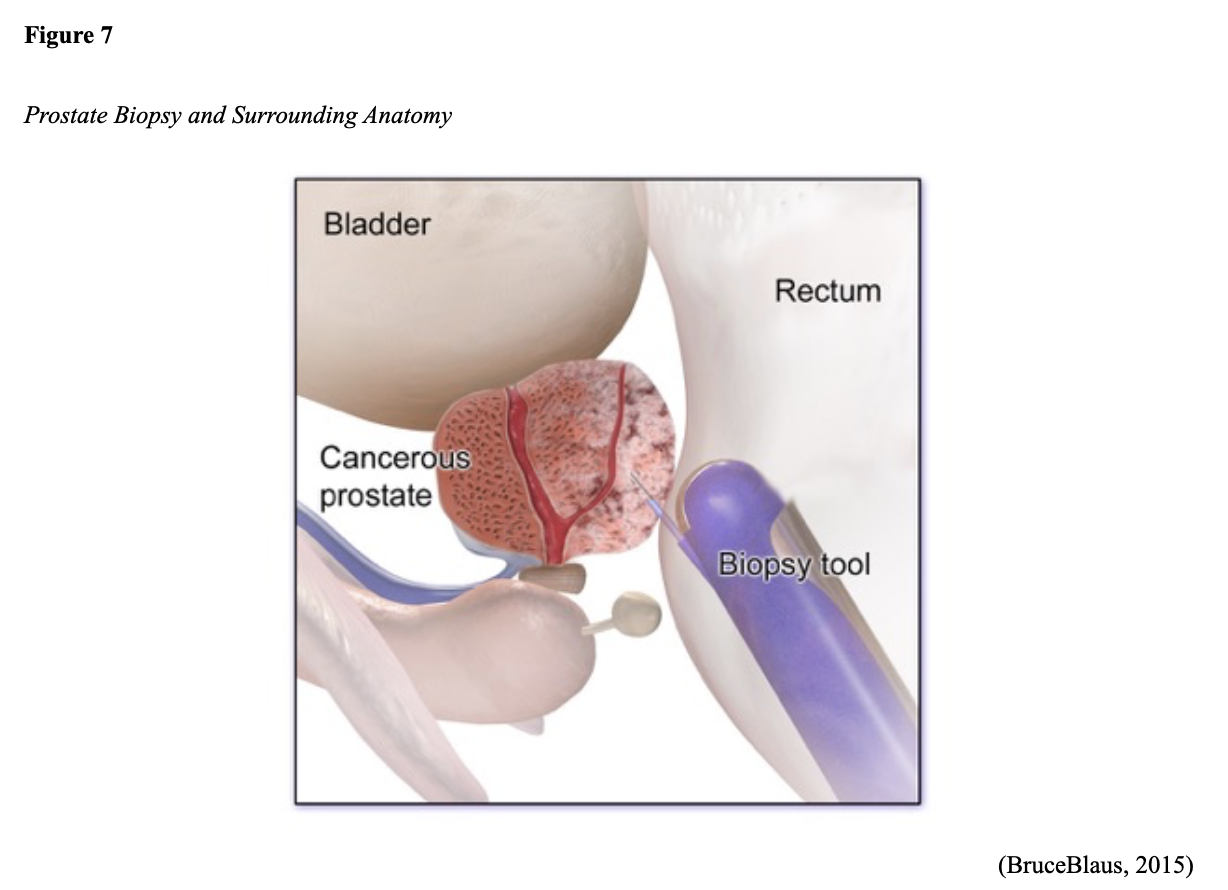
While the PSA and DRE can be useful in detecting prostate gland abnormalities, tissue sampling is necessary to confirm prostate cancer and establish its clinical features. A transrectal ultrasound-guided (TRUS) core biopsy of the prostate is the most common tissue sampling procedure in which a needle is guided through the rectum (transrectal biopsy) or the skin between the scrotum and anus (transperineal biopsy) to remove a small prostate tissue core. This process is repeated several times to obtain up to 12 core tissue samples. The TRUS procedure is demonstrated in Figure 6. Figure 7 provides a magnified view of a prostate biopsy highlighting the prostate’s anatomical location (ACS, 2017; Leslie et al., 2020).
Gleason Score
All prostate cancers are subjected to a histologic grading system called the Gleason score, which is vital in predicting prostate cancer’s behavior and determining the best treatment options. Initially developed in the 1960s, the Gleason score is the most widely used and reliable system to define prostate cancer’s aggressiveness (Leslie et al., 2020). The Gleason score is based on the cellular architecture, microscopic arrangement, and pattern of the glands within the prostate tissue. This is distinct from other cancers, which are generally defined by individual cellular characteristics. To determine the Gleason score, a histologic grade ranging from one to five is assigned to the tissue. This represents how abnormal the cancer cells look under a microscope and how aggressive the cancer appears. As demonstrated in Figure 8, if the cells appear very similar to normal, healthy prostate tissue, they are considered well-differentiated, and a grade one is assigned. If the cells are markedly abnormal and do not have any characteristic features of healthy cells, they are poorly-differentiated, and a grade five is assigned. Grades two through four have features between these extremes. Low-grade cancer cells tend to grow and spread more slowly than high-grade cancer cells. Two grades are assigned; one for the most predominant (primary) pattern identified within the tissue sample and one for the second most predominant pattern. Next, the two grades are added together to form the Gleason score, which ranges between 6 and 10 in modern-day clinical practice (Leslie et al., 2020; Prostate Cancer Foundation [PCF], n.d.).

Prostate Cancer Staging
Prostate cancer is grouped into four stages (I through IV), defined by the extent of the tumor presence and how rapidly the cancerous cells are growing. The four stages are determined by combining the Gleason Score with the Tumor, Nodes, and Metastasis (TNM) system. T stands for the primary tumor and is a measure of the tumor’s size and extent; N stands for lymph node(s) and denotes if cancer has spread into nearby lymph nodes; M stands for metastasis and denotes that cancer has spread to distant sites in the body. Staging is crucial as it helps to determine options for treatment (Leslie et al., 2020; PCF, n.d.). The only way to definitively identify the presence or absence of distant metastases is through radiographic imaging. However, unlike most cancer diagnoses, systemic imaging studies are not universally recommended for all patients diagnosed with prostate cancer. When imaging studies are indicated, the most commonly performed tests may include one or several of the following: radionuclide bone scan, single-photon emission computerized tomography (SPECT), plain film radiographs (x-rays), ultrasound, computerized tomography (CT scans), positron emission tomography/computed tomography (PET/CT) scan, sodium fluoride PET/CT scan, or advanced magnetic resonance imaging (MRI) techniques such as multi-parametric magnetic resonance imaging (mpMRI; NCCN, 2020).
For details regarding diagnostic radiology imaging modalities and nursing implications, refer to the Diagnostic Radiology NursingCE Course and earn 4.25 ANCC credits.
Management
Watchful Waiting
Not all men diagnosed with prostate cancer will require treatment, as it is characteristically slow-growing, and in many cases, patients die from other causes. Active surveillance or “watchful waiting” is usually a reasonable option for early-stage prostate cancer patients. The NCI dictionary of cancer terminology defines watchful waiting as:
“Closely watching a patient’s condition but not giving treatment unless symptoms appear or change. Watchful waiting is sometimes used in conditions that progress slowly. It is also used when the risks of treatment are greater than the possible benefits. During watchful waiting, patients may be given certain tests and exams. Watchful waiting is sometimes used in prostate cancer. It is a type of expectant management” (NCI, n.d.).
Patients often have anxiety and uncertainties regarding this recommendation due to the natural fears associated with a cancer diagnosis. Nurses serve an important role in educating patients on the rationale for watchful waiting, clarifying how this method is evidence-based and can provide valuable information regarding how quickly the prostate cancer is progressing, if at all. Watchful waiting typically involves long-term monitoring with modalities such as periodic PSA testing, DRE exams, prostate biopsies, symptom assessment, and imaging studies until clinicians and patients collectively decide that treatment should be implemented (NCCN, 2020; Urology Care Foundation, 2019).
Treatment Modalities
Treatment for prostate cancer is divided into two major categories; localized and systemic therapies, as outlined in Figure 9. Patients with early-stage and localized disease are commonly offered surgical intervention, followed by adjuvant (post-surgery) radiation therapy. Patients with advanced or metastatic prostate cancer are more likely to be treated with a combination of systemic therapies and are subject to periods of relapse and remission (NCCN, 2020).

Radical Prostatectomy
If the cancer is confined to the prostate, then a radical prostatectomy may be performed. As demonstrated in Figure 10, the entire prostate gland, and usually the seminal vesicles, surrounding tissue, lymph nodes, nerves, and veins are removed. A portion of the urethra is also removed, and the remaining urethra is anastomosed at the bladder neck. A urinary catheter is temporarily inserted to drain the urine and allow the patient to heal (ACS, 2019c).

Erectile dysfunction (ED) or impotence is one of the most common risks associated with radical prostatectomy. Since the nerves which control a man’s ability to have an erection are within proximity to the prostate gland, they may become damaged, severed, or removed during the surgery. Approximately 50% of men with intact nerves will regain some ability to have an erection, but it can take six to twelve months. Men with other health conditions that impair their ability to maintain an erection, such as diabetes or vascular issues, will have a more difficult time regaining their normal function. Urinary incontinence and damage to the urethra is another common risk associated with radical prostatectomy. Following surgery, up to 50% of men will develop urinary incontinence, and the degree of incontinence can range from intermittent dribbling and stress incontinence to continuous leakage requiring the use of pads or incontinence briefs (University of Michigan Health System [UMHS], 2019).
The side effects of prostate cancer treatment on sexual function and quality of life are well-cited. Urinary and sexual dysfunction are the most frequently reported side effects of prostate cancer treatment and among the most distressing. If left untreated, ED can lead to significant physical, psychological, and interpersonal consequences and impair quality of life and overall well-being. Nurses are tasked with addressing these issues with sensitivity, empathy, and compassion, fostering a safe and nonjudgmental environment for patients to openly express their concerns. Nurses should be prepared to educate patients and their partners, offer psychosocial support, and connect patients with resources, support groups, and medical specialists to manage these long-term effects (Yarbro et al., 2018).
Cryotherapy
Cryotherapy, also referred to as cryosurgery or cryoablation, is a minimally invasive surgery that uses thin needles and controlled freezing gas to destroy the cancer cells. It is a relatively novel and revolutionary treatment modality but still lacks rigorous, long-term survival data. It is offered to patients with localized or locally advanced prostate cancer and may be used alongside other treatments. Ultrasound guidance is used to facilitate the placement of the cryoprobes into the prostate since cryotherapy destroys both healthy and cancerous tissue that it comes in contact with. Argon gas is subsequently injected into the prostate, promoting the formation of ice crystals inside and around the cells. The freezing and thawing process destroys the cancer cells by dehydrating them, causing extreme changes in the pH levels, and preventing blood flow, blocking necessary nutrients. While the procedure is generally well-tolerated, nurses should counsel patients that it is normal to experience soreness and hematuria for one or two days following the procedure. Potential complications include urinary incontinence, injury to the rectum, and ED (ZERO - The End of Prostate Cancer, n.d.).
Radiation Therapy
Radiation therapy is a type of localized cancer treatment that uses high-energy rays of electron, proton, or neutron beams to destroy cancer cells. The primary objective is to deliver a precisely measured dose of radiation to a defined tumor with as little injury as possible to surrounding healthy tissue. Radiation induces damage to cancer cells, leading to biological changes in the DNA, rendering them incapable of reproducing or spreading. All healthy and cancerous cells are vulnerable to the effects of radiation and may be injured or destroyed; however, most normal cells can repair themselves and remain functional. The total dose of radiation is hyper-fractionated, which means it is administered in smaller divided doses, or fractions, rather than all at once. Hyper-fractionation allows healthy cells a chance to recover between dosing. Each dose is called a fraction, and the total number of fractions depends on the tumor size, location, reason for treatment, patient’s overall health, performance status, goals of therapy, as well as consideration of any other treatments the patient is receiving. Radiation can be delivered externally or internally, and some patients may receive both types (Yarbro et al., 2018). For prostate cancer, radiation therapy may be administered for early-stage and low-grade prostate cancer confined to the prostate gland or as part of the treatment regimen alongside hormonal therapy. Up to 50% of men will require radiation therapy after surgery (ACS, 2019a; Tamada et al., 2017). The two most common types of radiotherapy used for prostate cancer include internal brachytherapy and external beam radiation therapy (EBRT) and will be described in this subsection (NCCN, 2020).
Brachytherapy
Prostate brachytherapy is a type of minimally invasive radiation therapy that implants a small wire or radioactive seeds directly into the prostatic tissue. Brachytherapy delivers high and concentrated doses of radiation to the prostate gland from inside the body. Hormone therapy is sometimes given for three to six months before brachytherapy to shrink the prostate gland and optimize the radiation effect. The two brachytherapy types include a temporary high-dose-rate (HDR) or a permanent low-dose-rate (LDR), which are performed on an outpatient basis and typically require general anesthesia. Several catheters with radioactive pellets are placed into the prostate gland in HDR brachytherapy, as demonstrated in Figure 11. The catheters transmit concentrated bursts of high-dose radiation pellets into the tumor bed (Memorial Sloan Kettering Cancer Center [MSKCC], n.d.). With LDR brachytherapy, permanent radioactive seeds are placed in the prostate gland and slowly release radiation over several months. Up to 100 seeds may be inserted depending on the size of the prostate. The radiation emitted from the seeds only travels a short distance, limiting the amount of damage to nearby tissues. The radioactivity lessens gradually over several weeks. Nurses should counsel patients on staying at least three feet away from pregnant women and small children for a specified period to ensure any unnecessary risk is avoided. Although there is little clinical data available to validate this recommendation, it is endorsed by the International Atomic Energy Agency (IAEA, n.d.) within their Radiation Protection of Patients (RPOP) recommendations. Patients should also be counseled that detection systems can sometimes pick up low radiation levels at airports, so they should carry a physician’s note or radiation card regarding their treatment. Nurses should reassure patients that they can safely go about their regular routines and lifestyles without potentially exposing others (ACS, 2019a; MSKCC, n.d.).

EBRT
EBRT is radiation delivered from a source outside the body, directly to the cancer site. ERBT uses a linear accelerator to generate and deliver high-energy x-rays in small daily doses. Intensity-modulated radiation therapy (IMRT) is the most common type of EBRT for prostate cancer. It uses a computerized machine that travels around the patient as it delivers the radiotherapy. This technology allows for the more precise shaping and aiming of the radiation beams at the prostate, covering several angles and allowing for increased intensity (strength) of the beams. This technology limits the dose of radiation to surrounding tissues and enables the patient to tolerate a higher radiation dose to cancer, improving clinical outcomes and survival (ACS, 2019a; Fischer-Valuck et al., 2018).
Radiation Side Effects. Nurses caring for patients undergoing radiation therapy serve multifaceted roles in monitoring for and managing side effects. Radiation side effects depend on the specific area(s) of the body affected and the dose received. Radiation for prostate cancer can affect underlying structures located within the radiation field, such as the rectum or bladder (Yarbro et al., 2018). There are also differences in side effect profiles based on the type of radiation received. According to Johns Hopkins Medicine (n.d.), about 25 to 50% of men who undergo brachytherapy will experience ED following prostate brachytherapy compared to nearly 50% of men who undergo EBRT. LDR brachytherapy carries the added risk of the implanted seeds migrating to other sites in the body. Superficial skin irritation at the treatment site is common and can include redness, blistering, and inflammation, giving the skin the classic appearance of a sunburn. The most common side effects of radiation to the prostate include lymphedema in the legs or genital region, urinary frequency, dysuria, incontinence of bladder or bowel, cystitis (inflammation of the bladder), hematuria (blood in the urine), urethral stricture, and proctitis (inflammation of the rectum including pain with defecation and rectal bleeding; ACS, 2019a). Systemic effects may include fatigue, weakness, dehydration, scarring, fibrosis, and adhesion formation (the tissues impacted by radiation stick together; ACS, 2020; Yarbro et al., 2018).
For more information regarding nursing implications in radiation therapy, refer to the Oncology Nursing Part 1: Surgical and Radiation Oncology Nursing CE Course and earn 5 ANCC credits.
Androgen Deprivation Treatment (ADT)
ADT is also commonly referred to as testosterone-depleting therapy. Since testosterone cannot discriminate between healthy tissue receptors and those of cancerous tissue, ADT is the most common systemic treatment modality for prostate cancer. It deprives the body of androgens by lowering (or depleting) the testosterone level. Prostate cancer usually stops growing in response to hormone therapy, at least for a while. CRPC occurs when cancer outsmarts or becomes resistant to ADT therapy and begins to grow again despite hormone-blocking treatments. The most common approaches to androgen deprivation include castration, antiandrogens, and combined-androgen blockade. A castrate level refers to having 90 to 95% less testosterone than a healthy male, and castration may be achieved surgically or chemically. Orchiectomy is the surgical removal of the testicles, a permanent and irreversible procedure that can reduce the testosterone level in the blood by 90 to 95%. Chemical castration is much more common and involves the use of LHRH analogs or LHRH antagonists (NCI, 2019).
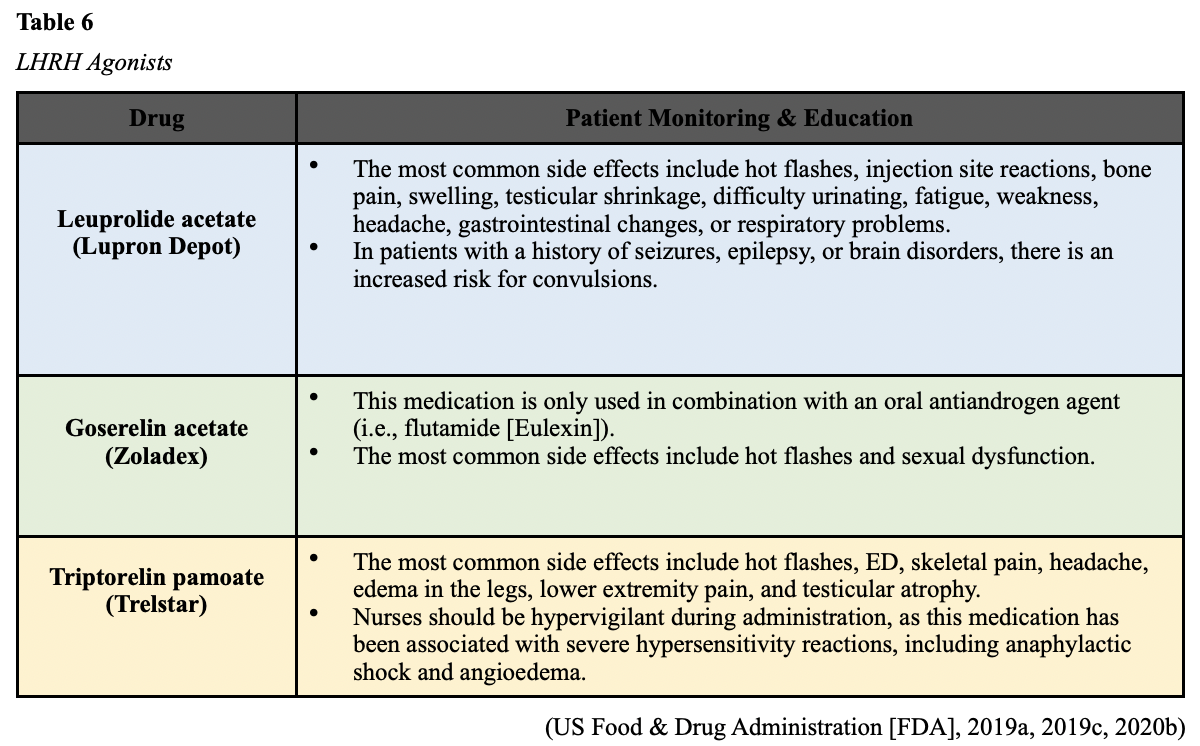
LHRH Agonists
LHRH agonists (sometimes called LHRH analogs) mimic LHRH’s action by occupying the receptors’ pituitary glands. Administration of these drugs causes the testicles to temporarily increase testosterone production, igniting a “testosterone flare” before blocking its release. Since the LHRH agonist has a longer half-life than physiologic LHRH, the LHRH agonist occupies the AR with greater affinity. Over time, the continued presence of high levels of LHRH agonists triggers the pituitary gland to stop producing LH, thereby halting the production of testosterone and reducing the body’s testosterone to castrate level. The testosterone flare is usually counteracted by the concurrent use of oral antiandrogen therapy (described below) for several treatment weeks. LHRH agonists are administered by injection or may be implanted under the skin. Currently, the three primary LHRH agonists used to treat prostate cancer in the US include leuprolide acetate (Lupron Depot), goserelin acetate (Zoladex), and triptorelin pamoate (Trelstar). All three of these agents are administered by injection. Table 6 outlines the pertinent and unique patient teaching points associated with each agent. Nurses caring for patients on LHRH agonists should be aware that all medications in this class carry an increased risk of hyperglycemia/diabetes, myocardial infarction (MI), sudden cardiac death, and stroke. Further, LHRH agonists are associated with an initial testosterone flare, which may cause an acute worsening of symptoms. This is particularly concerning for patients with advanced prostate cancer as it can lead to significant bone pain and ureter or bladder outlet obstruction (NCI, 2019). The testosterone flare can also induce spinal cord compression (SCC) in patients with metastatic disease to the spinal column in severe cases. SCC is an oncologic emergency characterized by compression of the spinal cord from malignant tumor invasion into the epidural space. SCC requires prompt recognition and immediate attention to preserve function and reduce morbidity. The symptoms of SCC may be overt or subtle in presentation and may be overlooked, contributing to increased morbidity and mortality. Nurses are vital to improving patient outcomes, as they are often the first point of contact with the patient and involved in patient triage and assessment. Delayed or improper treatment can lead to devastating functional losses. The actions of a skilled nurse can thwart progression to a life-threatening emergency. Nurses should become well-versed in the following key signs and symptoms of SCC:
- sudden onset of acute back pain that worsens in the supine recumbent position and may be relieved by sitting
- neurologic dysfunction such as numbness or paresthesia
- bowel or bladder dysfunction such as incontinence, passing very little urine, or inability to urinate or defecate
- altered gait or difficulty ambulating
Initiating treatment as early as possible is critical and involves administering corticosteroids to reduce vasogenic edema within the spinal cord, thereby improving neurologic dysfunction and relieving pain. Definitive treatment typically involves radiation therapy or neurosurgery (Klemencic & Perkins, 2019; Olsen et al., 2019; Yarbro et al., 2018).
LHRH Antagonists
LHRH antagonists are referred to as GnRH antagonists. These agents work by preventing LHRH from binding to its receptors in the pituitary gland, thereby inhibiting LH and testosterone production. Unlike LHRH agonists, LHRH antagonists do not cause a testosterone flare. Degarelix (Firmagon) is currently the only LHRH antagonist approved for prostate cancer treatment in the US (NCI, 2019). Like LHRH agonists, Degarelix (Firmagon) is also administered as an injection. Nurses should counsel patients on the most common side effects, including mild injection site reactions (localized pain, erythema, swelling or induration), hot flashes, and weight gain. Patients will also need to undergo periodic cardiac monitoring (with an EKG) and liver function tests. Although rare, hypersensitivity reactions have been reported (FDA, 2015a).
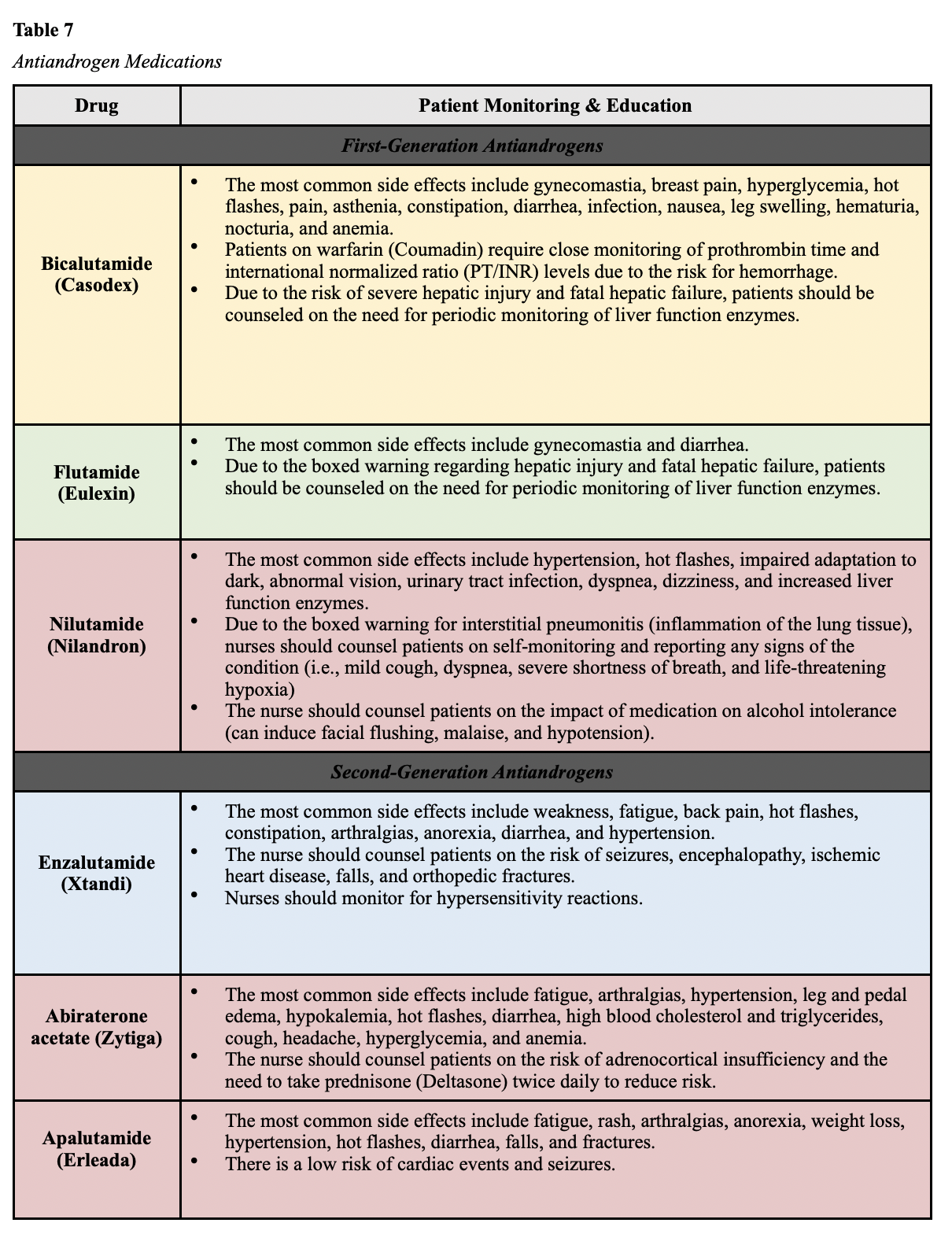
Antiandrogen Therapy
Antiandrogens are also called androgen receptor inhibitors or androgen receptor antagonists. These medications differ from LHRH antagonists by blocking particular facets of androgen signaling. They compete with androgens by binding to the AR. Testosterone circulates through the body but cannot interact with the prostate gland or promote cancer growth. Antiandrogens are oral medications that are rarely used as single agents since they do not block testosterone production. Instead, they are used concomitantly with LHRH agonists (unless the patient has undergone a bilateral orchiectomy). This combined regimen is referred to as a combined androgen blockade. There are two major classes of antiandrogens; first-generation and second-generation. First-generation antiandrogens are credited with establishing the androgen receptor blockade as an effective treatment strategy in prostate cancer; however, they do not completely block all androgen receptor activity. These agents primarily block androgen production in the testes. First-generation antiandrogens currently approved for use in the US include bicalutamide (Casodex), flutamide (Eulexin), and nilutamide (Nilandron). Second-generation antiandrogens were developed to improve upon the mechanisms of first-generation drugs and in an attempt to bypass resistance to therapy. Second-generation agents have increased specificity and higher affinity for androgen receptors. Abiraterone acetate (Zytiga) was the first second-generation antiandrogen approved by the FDA in 2011. It is slightly different than others in the class as it works by preventing androgen biosynthesis and testosterone production in the testes, the adrenal glands, and the tumor. There are four second-generation antiandrogens currently approved by the FDA: enzalutamide (Xtandi), abiraterone acetate (Zytiga), apalutamide (Erleada), and darolutamide (Nubeqa). Table 7 outlines some drug-specific patient teaching points (NCI, 2019; Rice et al., 2019).
Oral cancer drugs are potentially hazardous and require special precautions to ensure safety when handling, especially for caregivers. Nurses serve a critical role in educating patients and caregivers on safe drug handling and disposal before oral cancer medications are prescribed. Some essential teaching points adapted from the Oncology Nursing Society (ONS) chemotherapy administration safety standards include the following:
- Patients should keep cancer drugs in the original packaging until they’re used or placed within the daily pillbox.
- Patients should not mix chemotherapy medications with other medications in their pillbox.
- Patients should perform hand hygiene (soap and water) before and after handling all medications.
- Patients should not let their medication come in contact with household surfaces (countertops, tables). If they do, they should clean the surface thoroughly to remove all traces of the drug.
- Patients should store medications in a cool, dry place, away from excess heat or sunlight exposure.
- Patients should never discard cancer medications in the household trash, place them down the drain, or flush them down the toilet.
- Patients should inquire with their pharmacist about where to return unused and left-over medication.
- Empty pill bottles may be put in household trash; patients should not recycle the bottles.
- Patients should never reuse cancer medication pill bottles.
- Caregivers should transfer the medication into a cup or spoon when handling the medication. If picking up the medication with their hand is unavoidable, caregivers should wear disposable gloves to prevent any unnecessary exposure (i.e., absorption via the skin).
- If there is any contact with bodily fluids, household trash should be double-bagged.
- Patients and caregivers should discard gloves in household trash after one use; they should not reuse gloves (Olsen et al., 2019).

Chemotherapy
Chemotherapy works by destroying quickly dividing cells and is not commonly used as an upfront treatment option for prostate cancer. Due to the slow-growing nature of the disease and the high toxicity associated with chemotherapy, it is generally reserved for more advanced, widespread disease stages that have become refractory to the effects of ADT and antiandrogen therapy. When used as salvage therapy for progressive disease, chemotherapy has shown success in extending the longevity and quality of life in many patients. As a class, chemotherapy encompasses a group of high-risk, hazardous drugs that are administered with the intent to destroy as many cancer cells with as minimal effect on healthy cells as possible. Chemotherapy generally works by interfering with the normal cell cycle, impairing DNA synthesis and cell replication, which thereby prevents cancer cells from dividing, multiplying, and forming into new cancer cells. Since cancer cells tend to divide rapidly, chemotherapy targets cells that divide quickly. As a result, it also impacts healthy cells that divide quickly, such as those within the gastrointestinal tract, skin cells, and bone marrow. The most common chemotherapy agents used for prostate cancer include docetaxel (Taxotere), paclitaxel (Taxol), cabazitaxel (Jevtana), carboplatin (Paraplatin), and vinblastine (Velban) (NCCN, 2020; Olsen et al., 2019).
Side effects of chemotherapy are inevitable due to the nonspecific nature of cytotoxic therapy and how it simultaneously impacts healthy cells along with cancerous cells. However, side effects vary based on the drug type, dosage, duration of treatment, and specific patient factors. Not all patients respond in the same way, and not all chemotherapy agents pose the same risks. Assessment and education are the most critical components to ensuring timely recognition, intervention, and management of side effects as experienced by each patient. Many side effects, such as nausea, can be primarily thwarted by implementing appropriate prevention strategies and medications. As a group, the most common side effects include decreased blood counts (anemia, thrombocytopenia, neutropenia), fatigue, nausea, anorexia, alopecia (hair loss), mucositis (mouth sores), diarrhea, skin changes, and peripheral neuropathy (damage to the sensory nerves; Olsen et al., 2019; Yarbro et al., 2018).
PARP Inhibitors
PARP inhibitors are a class of targeted agents referred to as small molecule inhibitors that block the PARP. This protein has a critical role in cell growth, regulation, and repair, helping cancer cells repair themselves and survive. This inhibition leads to cancer cell death. PARP-inhibitors have revolutionized how BRCA–mutant cancers, such as ovarian cancer and breast cancers, are treated. Their value has recently been discovered in BRCA-mutant prostate cancers (Yarbro et al., 2018). On May 15, 2020, the FDA granted accelerated approval of rucaparib (Rubraca) for patients with BRCA-mutant, metastatic CRPC who have been previously received ADT and chemotherapy. The most common side effects of rucaparib (Rubraca) include fatigue, anemia, anorexia, rash, nausea, vomiting, diarrhea, constipation, thrombocytopenia, and increased transaminase levels (Oncology Nursing Society [ONS] Voice, 2020). Olaparib (Lynparza) is another oral PARP-inhibitor that is currently being studied with regard to its clinical usefulness for BRCA-mutant prostate cancers. Recent clinical results from the Targeted Agent and Profiling Utilization Registry (TAPUR) Study were presented at the 2020 American Society of Clinical Oncology (ASCO) Annual Meeting. In two small cohorts, olaparib (Lynparza) resulted in objective responses or stable disease for at least 16 weeks in more than two-thirds (68%) of patients with BRCA1 or BRCA2-mutant advanced prostate cancer (ASCO, 2020).
Immunotherapy
Sipuleucel-T (Provenge) is cellular immunotherapy customized using each patient’s immune cells to create a vaccine. The patient’s immune cells are collected through a process called leukapheresis and then developed into a vaccine devised to boost the patient’s immune system’s ability to attack prostate cancer. The cells are subsequently returned to the patient through an IV infusion about 72 hours later. Nurses should counsel patients on the cell collection process; they will receive three doses, about two weeks apart. The infusion is generally well-tolerated, and the most common side effects include fever, chills, infusion-related reactions, and headache (NCCN, 2020). Pembrolizumab (Keytruda) is a type of immunotherapy that blocks the PD-1 pathway and triggers the immune system to recognize cancer cells as foreign and attack them. In prostate cancer, the role of pembrolizumab (Keytruda) is limited, reserved for patients with an MSI-H or dMMR mutation (Reichert et al., 2019). The most common side effects of pembrolizumab (Keytruda) include fatigue, nausea, anorexia, cough, diarrhea, arthralgias, myalgias, skin rash, pruritus, and flu-like symptoms. An immune response can impact any organ system, inducing nonspecific inflammation throughout the body, ranging from mild inflammatory effects to life-threatening reactions that develop without warning. Some of the most severe include hepatitis, pneumonitis, enterocolitis, uveitis, and Stevens-Johnson syndrome (SJS), a rare, severe disorder of the skin and mucous membranes. Therefore, all immunotherapy agents carry boxed warnings for immune-mediated adverse reactions (irAEs), which can be fatal if left untreated. Nursing care of the patient receiving immunotherapy requires cautious triage and continuous meticulous assessment to identify signs of potential irAEs, as a timely diagnosis is critical to ensure prompt response and reduce morbidity. Most immune-related events are reversible with immunosuppressive steroid treatment, but patient education is vital. Nurses must teach patients and caregivers about the importance of self-assessment and the immediate reporting of any symptoms. With pneumonitis, symptoms can range from mild cough and dyspnea to severe shortness of breath and life-threatening hypoxia. GI toxicity can range from mild diarrhea and abdominal cramping to severe colitis, which can be fatal if not managed. Skin toxicity may develop as mild pruritus or dermatitis and can progress to SJS. Life-threatening endocrinopathies can cause an abundance of symptoms that can vary widely, such as extreme weakness, excessive fatigue or lethargy, electrolyte disturbances, thyroid inflammation, and pituitary dysfunction (Olsen et al., 2019; Winer et al., 2018).
For a more detailed review of the principles of radiation, chemotherapy, immunotherapy, and specific nursing implications, refer to the following NursingCE courses:
- Oncology Nursing Part 1: Surgical and Radiation Oncology (5 ANCC contact hours)
- Oncology Nursing Part 2: Chemotherapy and Oncologic Emergencies (5 contact hours)
- Oncology Medication Administration for LPNs and RNs (7 ANCC contact hours)
Skeletal-Related Events (SREs)
Since bone is one of the most common sites of metastases for prostate cancer, bone health and preventing SREs is an important part of prostate cancer treatment. Bisphosphonates such as denosumab (XGeva) and zoledronic acid (Zometa) are injectable agents that reduce the risk for disease-related skeletal complications, such as fracture, SCC, or the need for palliative surgery or radiation therapy to the bones. Under physiologic conditions, the body is continuously breaking down and rebuilding bone to maintain the strength and health of the bones. In patients with bone metastases from cancer, the breakdown and rebuilding of bones can become overactive, weakening the bones and leading to serious complications such as fractures. Since osteoclasts are the cells responsible for bone resorption, denosumab (XGeva) binds to the RANK ligand (RANKL), a protein that is essential for the formation, function, and survival. By binding to the RANKL, denosumab (Xgeva) inhibits osteoclastic activity, thereby decreasing bone resorption and increasing bone mass and strength. The most common side effects include hypocalcemia, weakness, fatigue, acute kidney injury, nausea, diarrhea, infusion reactions, and flu-like symptoms. Although rare, atypical subtrochanteric and diaphyseal femoral fractures have been reported in patients receiving bisphosphonate therapy; these fractures occur after minimal or no trauma. Nurses should counsel patients on the importance of adequate calcium and vitamin D intake either through dietary sources or supplementation to reduce the risk for hypocalcemia and atypical fractures. Additionally, all bisphosphonates carry a risk for osteonecrosis of the jaw (ONJ), which is a severe medication complication resulting in progressive bone destruction in the maxillofacial region. The pathophysiology of ONJ is poorly understood, but it can lead to significant morbidity, infection, and negatively impact the quality of life. The risk of ONJ is heightened with dental extractions or implants. Patients should be educated on risk reduction strategies such as maintaining good oral hygiene practices, routine follow up with their dentist, and avoiding dental implants or extractions. Nurses should encourage all patients to undergo a baseline dental evaluation prior to starting bisphosphonate therapy (NCCN, 2020; Rosella et al., 2016).
References
American Board of Internal Medicine. (2020). ABIM laboratory test reference ranges - January 2020. https://www.abim.org/~/media/ABIM%20Public/Files/pdf/exam/laboratory-reference-ranges.pdf
American Cancer Society. (2017). Prostate pathology. https://www.cancer.org/treatment/understanding-your-diagnosis/tests/understanding-your-pathology-report/prostate-pathology.html
American Cancer Society. (2019a). Radiation therapy for prostate cancer. https://www.cancer.org/cancer/prostate-cancer/treating/radiation-therapy.html
American Cancer Society. (2019b). Screening tests for prostate cancer. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/tests.html
American Cancer Society. (2019c). Surgery for prostate cancer. https://www.cancer.org/cancer/prostate-cancer/treating/surgery.html
American Cancer Society. (2020). Key statistics for prostate cancer. https://www.cancer.org/cancer/prostate-cancer/about/key-statistics.html
American Society of Clinical Oncology. (2020). TAPUR study shows encouraging results for olaparib in BRCA-mutated advanced prostate and pancreatic cancers. https://www.asco.org/about-asco/press-center/news-releases/tapur-study-shows-encouraging-results-olaparib-brca-mutated
Brechka, H., Bhanvadia, R. R., VanOpstall, C., & Griend, D. J. (2017). HOXB13 mutations and binding partners in prostate development and cancer: Function, clinical significance, and future directions. Genes & Diseases, 4(2), 75-87. https://doi.org/10.1016/j.gendis.2017.01.003
BruceBlaus. (2015). Prostate biopsy and surrounding anatomy [image]. https://commons.wikimedia.org/wiki/File:Prostate_Needle_Biopsy.png
Cadet, M. J., Allen, D. H., & Patterson-Johnson, J. (2019). Prostate cancer: How nurse practitioners can aid in disease diagnosis and management. Clinical Journal of Oncology Nursing, 23(3), 247-250. https://doi.org/10.1188/19.CJON.247-250
Cancer Research UK. (2015). HDR brachytherapy for prostate cancer [image]. https://commons.wikimedia.org/wiki/File:Diagram_showing_how_you_have_high_dose_brachytherapy_for_prostate_cancer_CRUK_419.svg
Cancer Research UK. (2016a). Radical prostatectomy [image]. https://commons.wikimedia.org/wiki/File:Diagram_showing_before_and_after_a_radical_prostatectomy_CRUK_473.svg
Cancer Research UK. (2016b). Transrectal ultrasound (TRUS) prostate biopsy [image]. https://commons.wikimedia.org/wiki/File:Diagram_showing_a_transperineal_prostate_biopsy_CRUK_473.svg
The Centers for Disease Control and Prevention. (2020). Prostate cancer. https://www.cdc.gov/cancer/prostate/index.htm
Clavijo, R. I., & Hsiao, W. (2018). Update on male reproductive endocrinology. Translational Andrology and Urology, 7(Suppl 3), S367-S372. https://doi.org/10.21037/tau.2018.03.25
Fischer-Valuck, B. W., Rao, Y. J., & Michalski, J. M. (2018). Intensity-modulated radiotherapy for prostate cancer. Translational Andrology and Urology, 7(3), 297-307. https://doi.org/10.21037/tau.2017.12.16
Fujita, K., & Nonomura, N. (2019). Role of androgen receptor in prostate cancer: A review. World Journal of Men’s Health, 37(3); 288-295. https://doi.org/10.5534/wjmh.180040
Häggström, M. (2019a). Gleason score [image]. https://commons.wikimedia.org/wiki/File:Gleasonscore.jpg
Häggström, M. (2019b). Prostate zones [image]. https://commons.wikimedia.org/wiki/File:Prostate_zones.png
Hartzfeld, D., Berse, B., Lowrance, W., Dash, A., Brawer, M., Lawrence, J., Meyer, L., & Lynch, J. (2016). Caring for patients with prostate cancer who are BRCA positive. Federal Practitioner, 33(Suppl 1), 46S-51S. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6375406/pdf/fp-33-2s-46s.pdf
Hemeonc.org. (2019). Flutamide (Eulexin). https://hemonc.org/wiki/Flutamide_(Eulexin)
International Atomic Energy Agency. (n.d.). Brachytherapy – What patients need to know. Retrieved September 6, 2020, from https://www.iaea.org/resources/rpop/patients-and-public/brachytherapy
Johns Hopkins Medicine. (n.d.). Erectile dysfunction after prostate cancer. Retrieved September 5, 2020, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/prostate-cancer/erectile-dysfunction-after-prostate-cancer
Kahl, K. L. (2018). Nurses play integral role in newly issues colorectal screening guidelines. https://www.oncnursingnews.com/web-exclusives/nurses-play-integral-role-in-newly-issued-colorectal-screening-guidelines
Klemencic, S., & Perkins, J. (2019). Diagnosis and management of oncologic emergencies. West J Emerg Medicine, 20(2), 316-322. https://doi.org/10.5811/westjem.2018.12.37335
Kong, L, Zhang, T., Tang, M., & Wang, D. (2014). The hypothalamic-pituitary-gonadal (HPG) axis [image]. https://commons.wikimedia.org/wiki/File:Hypothalamic–pituitary–gonadal_axis_in_males.png
Leslie, S. W., Soon-Sutton, T. L., Sajjad, H., & Siref, L. E. (2020). Prostate cancer. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK470550/
Mayo Clinic. (2019). Benign prostatic hyperplasia (BPH). https://www.mayoclinic.org/diseases-conditions/benign-prostatic-hyperplasia/symptoms-causes/syc-20370087
McCance, K. L., & Heuther, S. E. (2019). Pathophysiology: The biologic basis for disease in adults and children. (8th ed.). Elsevier.
Memorial Sloan Kettering Cancer Center. (n.d.). Brachytherapy for prostate cancer. Retrieved September 6, 2020, from https://www.mskcc.org/cancer-care/types/prostate/treatment/brachytherapy
National Cancer Institute. (n.d.). NCI dictionaries: Watchful waiting. Retrieved October 17, 2020, from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/watchful-waiting
National Cancer Institute. (2005). Visuals online: Prostate and nearby organs [image]. https://visualsonline.cancer.gov/details.cfm?imageid=4280
National Cancer Institute. (2008). Visuals online: Digital rectal exam [image]. https://visualsonline.cancer.gov/details.cfm?imageid=7136
National Cancer Institute. (2017). Prostate-specific antigen test. https://www.cancer.gov/types/prostate/psa-fact-sheet#what-is-a-normal-psa-test-result
National Cancer Institute. (2019). Hormone therapy for prostate cancer. https://www.cancer.gov/types/prostate/prostate-hormone-therapy-fact-sheet#r5
National Comprehensive Cancer Network. (2020). NCCN guidelines version 2.2020: Prostate cancer. https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf
Olsen, M., LeFebvre, K., & Brassil, K. (2019). Chemotherapy and immunotherapy guidelines and recommendations for practice. (1st Ed.). Oncology Nursing Society
Oncology Nursing Society Voice. (2020). FDA grants accelerated approval to rucaparib for BRCA-mutated, metastatic, castration-resistant prostate cancer.
https://voice.ons.org/news-and-views/fda-grants-accelerated-approval-to-rucaparib-for-brca-mutated-metastatic-castration
OpenStax College. (2013). Sex hormone production [image]. https://commons.wikimedia.org/wiki/File:Figure_28_03_01.jpg
Page, E. C., Bancroft, E. K., Brook, M. N., Assel, M., Al Battat, M. H., Thomas, S., Taylor, N., Chamberlain, A., Pope, J., Raghallaigh, H. N., Evans, D. G., Rothwell, J., Maehle, L., Grindedal, E. M., James, P., Mascarenhas, L., McKinley, J., Side, L., Thomas, T., … Eeles, R. A. (2019). Interim results from the IMPACT study: Evidence for prostate-specific antigen screening in BRCA2 mutations carriers. European Urology, 76(6),831-842. https://doi.org/10.1016/j.eururo.2019.08.019
Prostate Cancer Foundation. (n.d.). Gleason score and grade group. Retrieved October 17, 2020, from https://www.pcf.org/about-prostate-cancer/diagnosis-staging-prostate-cancer/gleason-score-isup-grade/
Reichert, Z. R., Urrutia, J., & Alumkal, J. J. (2019). Microsatellite instability as an emerging biomarker for checkpoint inhibitor response in advanced prostate cancer. JAMA Oncology, 5(4), 478-479. https://doi.org/10.1001/jamaoncol.2018.5789
Rice, M. A., Malhotra, S. V., & Stoyanova, T. (2019). Second-generation antiandrogens: From discovery to standard of care in castration-resistant prostate cancer. Frontiers in Oncology, 9(801), 1-12. https://doi.org/10.3389/fonc.2019.00801
Rosella, D., Papi, P., Giardino, R., Cicalini, E., Piccoli, L., & Pompa, G. (2016). Medication-related osteonecrosis of the jaw: Clinical and practice guidelines. Journal of International Society of Preventive & Community Dentistry. 6(2), 97-104. https://doi.org/10.4103/2231-0762.178742
Selchick, F. (2020). Prostate cancer treatment modalities [image].
Smith, R. A., Andrews, K. S., Brooks, D., Fedewa, S. A., Manassaram-Baptiste, D., Saslow, D., & Wender, R. C. (2019). Cancer screening in the United States, 2019: A review of current American Cancer Society guidelines and current issues in cancer screening. CA: A Cancer Journal for Clinicians, 69(3), 184-210. https://doi.org/10.3322/caac.21557
Tamada, S., Ninomiya, N., Kitamoto, K., Kato, M., Yamasaki, T., Iguchi, T., Ohmachi, T., & Nakatani, T. (2017). Comparative effectiveness of radical prostatectomy and curative radiotherapy in localized prostate cancer: Long-term follow-up. Journal of Radiation Research, 58(4), 552-558. https://doi.org/10.1093/jrr/rrw119
University of Michigan Health System. (2019). Radical prostatectomy. https://www.uofmhealth.org/health-library/hw77111
Urology Care Foundation. (2019). What is advanced prostate cancer? https://www.urologyhealth.org/urologic-conditions/advanced-prostate-cancer
US Food & Drug Administration. (2015a). Highlights of prescribing information: FIRMAGON (degarelix for injection). https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/022201s009lbl.pdf
US Food & Drug Administration. (2015b). Highlights of prescribing information: Nilutamide tablets. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/207631Orig1s000lbl.pdf
US Food & Drug Administration. (2017). Highlights of prescribing information: CASODEX® (bicalutamide). https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/020498s028lbl.pdf
US Food & Drug Administration. (2018). Highlights of prescribing information. ZYTIGA® (abiraterone acetate) tablets. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/202379s024lbl.pdf
US Food & Drug Administration. (2019a). Highlights of prescribing information: LUPRON DEPOT® (leuprolide acetate for depot suspension). https://www.rxabbvie.com/pdf/lupronuro_pi.pdf
US Food & Drug Administration. (2019b). Highlights of prescribing information: XTANDI® (enzalutamide). https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/203415s015lbl.pdf
US Food & Drug Administration. (2019c). Highlights of prescribing information: ZOLADEX® (goserelin acetate implant). http://documents.tersera.com/zoladex-us/10.8mg_MagnumPI.pdf
US Food & Drug Administration. (2020a). Highlights of prescribing information: ERLEADA® (apalutamide) tablets. http://www.janssenlabels.com/package-insert/product-monograph/prescribing-information/ERLEADA-pi.pdf
US Food & Drug Administration. (2020b). Highlights of prescribing information: TRELSTAR® (triptorelin pamoate for injectable suspension). http://www.trelstar.com/pdf/TrelstarPrescribingInformation_May2020.pdf
US National Library of Medicine. (2020). HOXB13 gene. https://ghr.nlm.nih.gov/gene/HOXB13
US Preventative Services Task Force. (2018). Screening for prostate cancer: US preventative services task force recommendation statement. JAMA, 319(18), 1901-1913. https://doi.org/10.1001/jama.2018.3710
Wang, G., Zhao, D., Spring, D. J., & DePinho, R. A. (2018). Genetics and biology of prostate cancer. Genes & Development, 32, 1105-1140. https://doi.org/10.1101/gad.315739.118
Winer, A., Bodor, J. N., & Borghaei, H. (2018). Identifying and managing the adverse effects of immune checkpoint blockade. Journal of Thoracic Disease, 10(Supple 3); S480-S489. https://doi.org/10.21037/jtd.2018.01.111
Yarbro, C. H., Wujcik, D., & Gobel, B. H. (Eds.). (2018). Cancer nursing: Principles and practice. (8th ed.). Jones & Bartlett Learning.
ZERO – The End of Prostate Cancer. (n.d.). Cryotherapy. Retrieved September 5, 2020, from https://zerocancer.org/learn/current-patients/types-of-treatment/cryotherapy/