About this course:
The purpose of this course is to explore the most common types of psychotherapy, providing an overview of the wide range of therapeutic approaches, indications, and core components to enhance nursing practice and the care of patients with mental health conditions.
Course preview
This module explores the most common types of psychotherapy, providing an overview of the wide range of therapeutic approaches, indications, and core components to enhance nursing practice and the care of patients with mental health conditions.
By the completion of this course, the nurse should be able to:
- define psychotherapy and discuss its indications, benefits, and limitations
- describe the historical background of various psychotherapies and the evolution of psychotherapy as a treatment for mental illness
- distinguish between each type of psychotherapy and their evidence-based indications, therapeutic strategies, and core features
Psychotherapy is a mainstay in the treatment of mental health conditions and is often combined with medications to manage distressing symptoms. Evidence-based psychotherapies are efficacious, beneficial, and cost-effective for many mental, emotional, and behavioral disorders. The American Psychiatric Association (APA, 2019) defines psychotherapy as any psychological service moderated by a trained professional (i.e., psychotherapist) who employs communication and interaction principles to assess, diagnose, and treat mental health disorders. Also referred to as talk therapy, psychotherapy is premised on establishing a supportive environment and collaborative relationship between the patient and psychotherapist to foster open discussion in an objective, neutral, and nonjudgmental manner. According to their respective state licensing boards, a psychotherapist includes any professionally trained and licensed individual to treat mental health conditions (e.g., psychologist, psychiatrist, psychiatric nurse, advanced practice registered nurse [APRN], counselor, therapist, or social worker). Psychotherapy is provided to individuals, couples, families, or small groups, and the most appropriate type is based on a person’s specific needs, problem(s), diagnoses, and individual preferences. While therapeutic approaches are varied and numerous, this module will discuss several of the most common evidence-based psychotherapeutic subtypes to increase the nurse's understanding of psychotherapy as a legitimate treatment for mental health conditions (APA, 2019; Wampold, 2019).
Epidemiology
Mental health conditions are prevalent throughout the world and create a significant public health challenge with high rates of disease burden. Individuals affected by mental health disorders have a higher incidence of co-occurring medical conditions that are poorly managed, contributing to increased symptom burden, lower levels of treatment adherence, higher levels of healthcare service utilization, and increased cost (Cook et al., 2017). In the US, nearly 1 in 5 adults (51.5 million) live with a mental illness. According to the National Center for Health Statistics (NCHS), in 2019, an estimated 29% of Americans aged 18 to 25 and 25% of those aged 26 to 49 suffered from some form of mental illness (National Institute of Mental Health [NIMH], 2021). Mental illness is explicitly defined as "having any mental, behavioral, or emotional disorder in the past year that met criteria of the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, or DSM-V, excluding developmental or substance use disorders" (Terlizzi & Zablotsky, 2020, p. 1). Mental health is as critical as physical health, and impairments can range from mild to life-altering, affecting a person’s overall health and functioning. Symptoms of mental illness differ depending on the type and severity of the problem, the most common of which include sleep and eating disturbances, social withdrawal, feelings of hopelessness, anger, prolonged sadness, suicidal thoughts, and an increased likelihood of substance abuse (NIMH, 2021).
Data from the 2019 National Health Interview Survey revealed that 19.2% of adults received mental health treatment in the prior 12 months, and 9.5% received some type of therapy. The percentage of adults who received therapy from a mental health professional declined with age (i.e., from 11.6% among those aged 18–44 to 5.7% among those aged 65 and over). Adult females were more likely than males to receive therapy, and non-Hispanic White adults (23.0%) were more likely to receive therapy than non-Hispanic Black (13.6%) and Hispanic (12.9%) adults (Terlizzi & Zablotsky, 2020). Public attitudes toward mental illness serve a prominent role in help-seeking behaviors. As cited in a recent systematic review and meta-analysis by Angermeyer and colleagues (2017), attitudes toward psychotherapy have significantly improved over the last 25 years, and prior negative stigmas regarding mental health treatment have declined. According to the researchers, the US public readily recommends and supports psychotherapy as a practical, effective, and evidence-based treatment strategy for mental illness. Their findings revealed that psychotherapy ranks as the most popular mental health treatment modality and is consistently preferred over medication (Angermeyer et al., 2017). Still, a significant gap remains between the availability of effective psychotherapies and their widespread delivery (Cook et al., 2017).
Indications, Benefits, and Limitations
While psychotherapy offers countless therapeutic benefits, the target outcomes include eliminating or controlling distressing symptoms (e.g., addictive behaviors, distress, anxiety, sadness, fear) and improving function, quality of life (QOL), and well-being. Patients with mental, emotional, or behavioral difficulties who receive psychotherapy achieve better outcomes than those who do not. Psychotherapy is more effective than several alternatives, including pharmacological therapy, and does not carry the risk of adverse side effects or high-cost burden. Research has also demonstrated that patients prefer psychotherapy to pharmacological treatments. Each therapeutic approach has specific indications; some are formulated for particular contexts, whereas others are effective across multiple frameworks. According to the APA (2020b), some of the most common generalized indications for psychotherapy include the following:
- to treat a psychiatric disorder
- to change maladaptive and disruptive thoughts
- to provide support during and/or following a crisis, major life event, difficult period, or a chronic problem impairing functioning and QOL
- to enhance a patient's capacity to make behavioral changes (e.g., weight loss, smoking cessation)
- to ameliorate or cope with relationship problems (e.g., marital issues or family conflict; Lebow, 2021)
Depression and anxiety disorders are among the most common and specific indications effectively treated with psychotherapy, with a substantial literature base highlighting its success. Research demonstrates that those who receive psychotherapy for depression and anxiety disorders achieve more durable treatment responses (i.e., are less prone to relapse) and better symptom control than when medication is used alone. Additionally, psychotherapy has demonstrated efficacy in treating substance abuse disorders (SUDs), marital problems, obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), personality disorders, sexual dysfunction, and other health problems (e.g., eating disorders like anorexia nervosa or bulimia nervosa, life-threatening or terminal illness like cancer or cystic fibrosis). It is useful across all populations, including children, adolescents, adults, and older adults (APA, 2020b; Wampold, 2019). Furthermore, "psychotherapy, as practiced in the real world, is as effective as psychotherapy delivered in the controlled conditions of randomized clinical trials" (Wampold, 2019, p.7).
Although psychotherapy is effective, it is underutilized and can be difficult to access at times, depending on location, and may not be covered or be inadequately covered by medical insurance. Most
...purchase below to continue the course
Overview of Cognitive and Behavioral Therapies
Psychiatrist Aaron Beck introduced the concept of cognitive therapy in the 1960s, premised on the idea that how an individual thinks determines their feelings and actions. Cognitive therapy focuses on what patients think rather than what they do and how this thinking leads to feelings of distress. Beck's initial efforts targeted depression, revealing how an individual's self-defeating attitude sustains depressive rumination. Beck maintained that altering dysfunctional thoughts and adverse emotional reactions could lessen and potentially alleviate distress and depressive symptoms. Specific interventions aim to help patients identify maladaptive cognitions (i.e., negative, harmful, or ineffective self-statements, beliefs, and thinking patterns). In this approach, increasing awareness of cognitive processes helps eliminate disparaging thought patterns that lead to despair. Cognitive therapy teaches patients to refute or disconfirm situational misappraisals and distorted core beliefs by identifying and rationalizing thoughts, collecting further data, and considering logical evidence to disprove them. Patients learn to construct alternate, more evidence-based appraisals, and core beliefs. By isolating distorted beliefs, patients learn to employ behavioral interventions to restructure actions and reduce maladaptive behaviors.
The principles of behavioral therapy involve changing behavior to diminish dysfunction and improve QOL. Unlike cognitive therapy, behavioral therapy does not focus on delving deeply into one's thoughts. Instead, it underscores the principles of learning applied to changing undesirable and dysfunctional behaviors, such as phobias, bedwetting, and nail-biting. By employing various conditioning techniques and tactics (e.g., behavioral activation [BA], systematic desensitization), patients learn healthier, more productive behaviors. Cognitive and behavioral therapies are frequently grouped into a single category based on their interconnectedness. They have evolved tremendously over the last several decades, extending their application to an array of psychotherapeutic approaches (Craske, 2017).
Cognitive Behavioral Therapy (CBT)
CBT is among the most well-cited and established forms of psychotherapy, as it has the most rigorous evidence supporting its clinical utility. It is often referred to as the gold standard of psychotherapy, as other forms of psychotherapy have not demonstrated superior efficacy for some conditions. It was originally applied to managing depression, and it was the first psychotherapy identified as evidence-based in most clinical guidelines (David et al., 2018). In addition to treating depression, it has demonstrated effectiveness in several other conditions, including anxiety, trauma (e.g., PTSD, childhood trauma, and sexual trauma), SUDs, eating disorders, and couples' distress. CBT may also help manage certain aspects of psychosis (e.g., psychotic episodes, schizophrenic delusions) and is validated across diverse demographics, including veterans and active service members (APA, 2019; Stein, 2020). According to Craske (2017), the overarching features of CBT include short-term, problem-focused, cognitive, and behavioral interventions. It is not a one-size-fits-all model, as there are several variations. CBT teaches patients to restructure cognitive distortions and self-defeating behaviors and replace them with more accurate thoughts and functional behaviors. The focus is narrowed to the patient's current problem(s) to provide practical solutions and strategies to manage them successfully. The specific intervention(s) employed will depend on the underlying issue, and a few primary subtypes of CBT are discussed in the next section. Patients are encouraged to apply the behaviors to real-life settings, allowing them to practice the skillset during the therapeutic relationship to troubleshoot new behaviors and obtain feedback from the psychotherapist. Patients learn to track their thoughts and activities to identify the affective and behavioral consequences during debriefing sessions with the psychotherapist. CBT is time-limited and typically consists of 8 to 16 sessions. In addition to face-to-face and telephone sessions, it can also be administered via computer-based programs, referred to as computer-based CBT (CCBT; APA, 2019; Craske, 2017; Stein, 2020).
CBT-Insomnia (CBT-I)
Insomnia and depression commonly coexist, and CBT-I is recommended as a first-line treatment for affected patients. CBT-I is a multi-component approach targeting behaviors and thoughts that interfere with sleep. In a recent systematic review and meta-analysis, Feng and colleagues (2020) found CBT-I to be safe, effective, and superior to no treatment for insomnia. CBT-I may be delivered face-to-face in individual or group settings over an average of 4 to 8 sessions. This approach includes sleep hygiene principles (e.g., establishing a consistent bedtime routine, avoiding substances like caffeine after lunch or alcohol and nicotine before bed or activities like vigorous exercise within 2 to 3 hours of sleep that interfere with sleep, avoiding daytime sleeping, optimizing the sleep environment, and creating a stable bedtime and wake time) and sleep restriction (e.g., limiting the time spent in bed to the approximate time of desired sleep). Patients are advised to create a 2-week sleep diary documenting their sleep habits, and the CBT-I approach is individualized based on the diary. The time spent asleep should be added to half of the time spent awake in bed, yielding the prescribed sleep restriction. This time should never be under 5 hours. Once the patient sleeps for at least 80% of the prescribed time for 7 consecutive days, the prescription should be increased by 20 minutes for the following week. Figure 1 provides an example of a sleep restriction calculation (Reynolds & Cone, 2018; Winkelman, 2021).

CBT-I teaches patients to avoid all other activities in bed (e.g., reading, watching TV) other than sleeping and sex. Patients are encouraged to go to bed when they feel most sleepy and get out of bed if they start feeling anxious while lying awake. If they feel anxious and unable to sleep, the patient should leave the room for approximately 10 to 15 minutes and return to bed when they feel sleepy. A scheduled wake time should be adhered to consistently, regardless of the amount of sleep achieved. This concept, which is called stimulus control, is designed to repair the cognitive association between the patient's bed, bedtime, and sleep. The cognitive components of CBT-I typically focus on anxious thoughts associated with sleep quality and quantity, realistic sleep quantity expectations, accurate attribution of daytime dysfunction and symptoms, and relaxation techniques (e.g., progressive muscle relaxation, diaphragmatic breathing, and meditation). The relaxation techniques decrease sympathetic stimulation and physical arousal at bedtime and facilitate calmness and awareness by reconnecting the mind and body.
Common misconceptions that should be addressed for patients with chronic insomnia include the belief that (a) sleep must occur for 8 hours uninterrupted to be sufficient, (b) sleep initiation should occur within 10 minutes, and (c) initial tiredness upon awakening indicates poor sleep quality. This cognitive retraining typically takes the most time and may require a referral to a psychiatric provider or sleep center (Reynolds & Cone, 2018; Winkelman, 2021). A recent study by McCurry and colleagues (2021) found that CBT-I delivered via telephone was effective. This randomized controlled trial (RCT) was completed in Washington State and involved 282 participants 60 years of age and above with chronic osteoarthritis pain. The researchers found that over half (56%) of the study participants remained in remission at a 1-year follow-up visit (McCurry et al., 2021). For most patients, nonpharmacological treatments should be given for 6 weeks to improve insomnia symptoms before escalating treatment to include a pharmacologic component (Reynolds & Cone, 2018).
Trauma-Focused CBT (TF-CBT)
TF-CBT is an evidence-based treatment strategy indicated for children and adolescents (ages 3 to 18) to help them overcome trauma-related difficulties. TF-CBT is most effective in treating childhood PTSD, child maltreatment, and other traumatic life events. TF-CBT also helps non-offending parents/caregivers (i.e., those who were not part of the child's trauma or abuse) cope effectively with their emotional distress surrounding the traumatic events and develop healthy skills to support their child (Children’s Bureau, 2018). Several studies cite TF-CBT as more effective for traumatized children than traditional psychotherapy options. In a follow-up study from a multicenter RCT for traumatized children, Jensen and colleagues (2017) found that youth who received TF-CBT experienced a more efficient improvement in trauma-related symptoms than those who received therapy as usual (TAU). These improvements associated with TF-CBT were sustained after 18 months. Furthermore, those assigned to TAU received 1.5 times the number of treatment sessions.
The primary objective of TF-CBT is to help the child and their parents/caregivers identify and cope with their distress and alter maladaptive behaviors. The TF-CBT treatment model employs trauma-sensitive interventions with CBT strategies individualized to the child and their specific circumstances while fostering a therapeutic relationship with the child and their parent/caregiver. The principal treatment components are denoted by the acronym "PRACTICE" and include the following:
- psychoeducation and parenting skills
- relaxation
- affective expression and regulation
- cognitive coping
- trauma narrative development and processing
- in vivo gradual exposure
- conjoint parent-child sessions
- enhancing safety and future development
Like other types of CBT, TF-CBT is a short-term approach (typically 12 to 16 sessions). It is often integrated with a more extensive treatment plan for children struggling with other mental, emotional, or behavioral challenges. TF-CBT is commonly comprised of one-on-one sessions for the child and the parent/caregiver, as well as child-parent joint sessions (Children’s Bureau, 2018).
Trauma-Focused Psychotherapy for Veterans. Active military service members and veterans are particularly vulnerable to trauma and the traumatic effects of PTSD. Stress is a standard component of everyday life; once the stressor is removed, individuals will typically resume their normal behaviors. However, active military service members and veterans are often impacted by combat stress and PTSD. Combat stress is a natural reaction to the mental and emotional strain placed on the mind and body in dangerous and traumatic situations. This condition can be challenging to detect since the symptoms can vary and include physical, emotional, and behavioral manifestations. Combat stress typically occurs for brief periods, and symptoms usually resolve after a service member returns home. PTSD is a psychiatric condition characterized by neural functioning changes in response to overwhelming stress, trauma, or horror. It may be preempted by either direct or indirect exposure to the trauma, including bearing witness to or hearing about horrific events. In both conditions, symptoms are not due to medication, substance use, or any other identifiable illness and cause significant distress or functional impairment (National Center for PTSD, 2021; US Department of Veterans Affairs [VA], 2019).
According to the VA (2019) and the most recent Substance Abuse and Mental Health Services Administration (SAMHSA, 2020) National Survey on Drug Use and Health, 1 in 4 (or 3.9 million) veterans had a mental illness. Combat stress and PSTD are prevalent, as nearly 20% of service members returning from deployment have or will have some form of these stress disorders. The VA Clinical Practice Guidelines for the Management of PSTD (2017) recommend individualized, trauma-focused psychotherapy as a highly regarded, first-line treatment for PTSD. Trauma-focused psychotherapy occurs over an average of 8 to 16 sessions during which the traumatic event is thoroughly explored. Trauma-focused psychotherapy implements various techniques, such as visualizing, analyzing the trauma (through talk or reflection), and altering unhelpful beliefs about the trauma to help patients recover from the event. Three trauma-focused therapies with significant evidence in the veteran population include prolonged exposure therapy (PE), cognitive processing therapy (CPT), and eye-movement desensitization and reprocessing (EMDR). These therapies have also been applied to non-veteran adults who experienced varying forms of trauma (e.g., physical abuse, sexual trauma) with demonstrated efficacy, but they are most well-known regarding their role in managing PTSD in veterans (National Center for PTSD, 2017, 2021).
PE. PE is one of the most widely studied forms of trauma-based psychotherapy and is validated across diverse populations (e.g., race-based trauma and rape victims). According to the National Center for PTSD (2020c), PE carries the strongest clinical recommendation across clinical practice guidelines for trauma and is considered suitable for patients with comorbidities such as SUD. PE was developed from the emotional processing theory, propositioning that PSTD develops from pathological fear and emotional structures in response to trauma. The fear and emotional structures are comprised of a stimulus (e.g., the offending event, noise, person, place, memory) that elicits a series of emotional and/or physiological responses when triggered (e.g., the sound of fireworks on the 4th of July may cause a veteran to feel distressed and anxious [heart-pounding, jittery, sweaty, unsafe, and wanting to flee the scene]). PE posits that recovery depends on modifying these altered fear and emotional responses, which can be accomplished through repeated exposure. Repeated exposure to the feared stimulus can reacclimate and revise the body's adverse emotional and physiological reactions in a relatively safe and controlled setting. The patient is equipped with positive coping skills (e.g., cognitive restructuring, relaxation techniques) to reset emotions and teach their mind and body that these traumatic memories and reminders are not dangerous and can be experienced without significant distress. As applied to the example above, when the fireworks are set off, the veteran could remind themselves that they are safe, their elevated heart rate is not dangerous, and they do not need to flee the scene. Additional core components of PE include repeated in-vivo confrontation (e.g., exposure to people, situations, or objects that the patient is avoiding due to emotional distress), repeated imaginal exposure to the trauma (e.g., recounting the details of the traumatic memory, writing a letter about the traumatic event), processing the details of the relived event, and holding a farewell ritual to leave the trauma in the past. PE is typically delivered in 8 to 15 weekly sessions, with each session lasting approximately 90 minutes (National Center for PSTD, 2020c).
CPT. CPT was initially used for female victims of sexual assault and rape and has demonstrated efficacy in treating refugees and those with PTSD-related conditions. Research indicates that CPT is an effective treatment for PSTD in veterans, significantly reducing symptom burden. It is currently recommended as a first-line treatment by all major PTSD treatment guidelines, including the VA, International Society for Traumatic Stress Studies (ISTSS), National Institute for Health and Care Excellence (NICE), and APA. CPT regards PTSD as a disorder of non-recovery, signifying that the patient's beliefs about the causes and consequences of the traumatic event are repeatedly relived, thereby generating powerful undesirable emotional responses. Overwhelming negative emotions preclude accurate processing of the traumatic event, counteracting the patient's recovery. Patients avoid triggers to prevent these emotional responses, further hindering natural recovery. In CPT, these avoidances are referred to as "stuck points." The primary goal of CPT is to identify the patient's stuck points. Through cognitive restructuring, patients acquire a more accurate understanding of their memories and emotions to drive the recovery process. During CPT, patients learn to reframe the negative thoughts surrounding the trauma. The psychotherapist engages the patient in a discussion about the event while encouraging the patient to talk about negative thoughts and complete short writing assignments. While CPT may be conducted via individual or group sessions, it is most effective in the individual format. It was developed initially as a 12-session protocol delivered over 3 months but can be customized depending on the patient's needs (National Center for PTSD, 2017, 2020a).
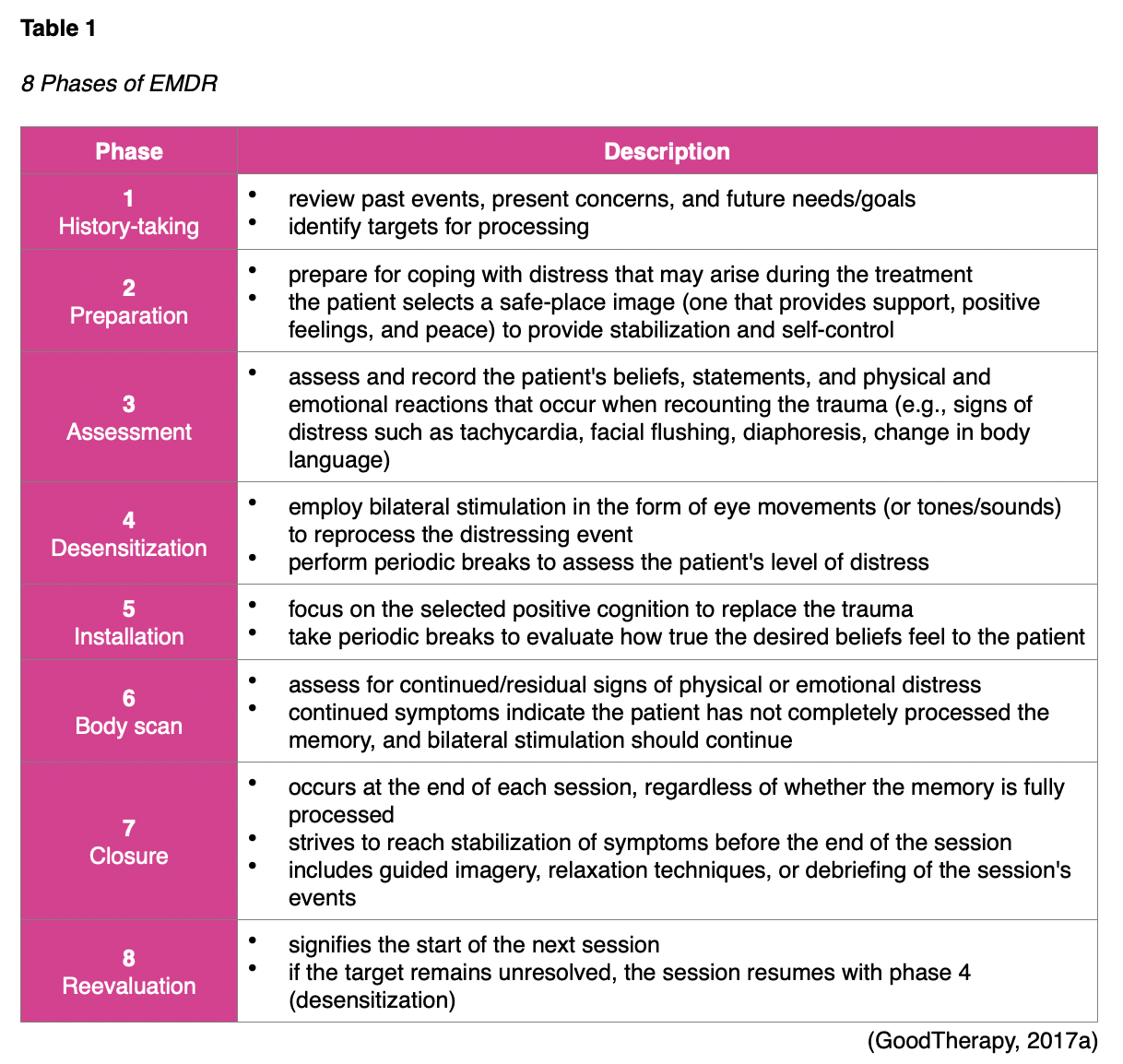
EMDR. EMDR is an effective and widely endorsed treatment for trauma explicitly designed for PTSD therapy. EMDR is premised on the theory of adaptive information processing (AIP), in which patients process experiences by connecting and integrating them with a network of existing emotions and memories. AIP helps patients make sense of experiences and emotions by correlating them with past events. EMDR is grounded in the idea that PTSD occurs when an incident is inadequately processed, and the memory is stored defectively, leading to symptoms. EMDR focuses on reexploring and reprocessing the traumatic event and defective memory by following an 8-phase approach (see Table 1). EMDR helps the patient make sense of the trauma by recalling the event while paying attention to a back-and-forth movement or sound (alternating bilateral stimulation). These simultaneous actions stimulate the brain's ability to reprocess distressing events. It helps integrate the new memory into the patient's memory system, thereby reducing undesirable symptoms. EMDR is typically administered as 90-minute weekly sessions over 3 months, but the duration can vary based on the patient's needs and response to treatment (Goodtherapy, 2017a; National Center for PTSD, 2020b).
Dialectical Behavioral Therapy (DBT)
DBT was developed by Marsha Linehan in the 1970s and incorporates specific Western and Eastern spiritual influences. It is a comprehensive form of CBT that was initially intended to treat chronically suicidal patients with borderline personality disorder, a mental illness characterized by unstable moods, relationships, self-image, and behavior. DBT has a primary objective of reducing non-suicidal self-injury (NSSI) and suicidal behaviors by thwarting therapy-interfering behaviors and altering behaviors interfering with the patient’s QOL. Findings from multiple studies reflect the efficacy of DBT across all aspects of suicide prevention, as well as in the management of SUD, depression, PTSD, attention deficit disorder, bipolar disorder, and eating disorders. This multi-component therapy operates within the context of dialectical methods (i.e., strategies that bring opposing concepts together, such as change and acceptance; DeCou et al., 2019). DBT focuses on problem-solving and acceptance-based interventions to treat issues surrounding emotional dysregulation. It continues to be cited as a highly effective therapy for those at high risk of suicide who also struggle with impulsivity. DBT assumes that many of a patient's problems are caused by skill deficits and combines CBT, skills training, and mindfulness techniques to teach patients how to regulate their emotions, hone their interpersonal skills, and cope with stress.
The APA Dictionary of Psychology defines mindfulness as the awareness of one's internal states and surroundings. It has been applied to various therapeutic interventions to help patients avoid destructive actions and responses by learning to observe their thoughts, emotions, and other present-moment experiences without judging or reacting to them (APA, 2020a). In its most simplistic form, mindfulness increases self-awareness by maintaining contact with the present. DBT includes four primary treatment modes: individual psychotherapy, group skills training, between-session or "in-the-moment" telephone coaching, and a therapist consultation team (DeCou et al., 2019; GoodTherapy, 2018a; Wampold, 2019).
Unlike traditional CBT described earlier, DBT is more time-inclusive, lasting for an average of 6 to 12 months. The standard treatment plan includes weekly individual therapy sessions (averaging 60 minutes per session), weekly group skills training (averaging 120 to 180 minutes per session), between-session telephone coaching (employed as needed based on the patient), and weekly psychotherapist team meetings. The group sessions are designed to help patients develop and practice behavioral skills through group work. Homework assignments encourage the practice and application of learned skills in daily life. Phone coaching provides support when challenging situations develop between sessions. Psychotherapist team meeting sessions are designed to support, motivate, and enhance providers’ skills as clinicians (McCain et al., 2018). Each treatment mode serves a vital role in achieving the core goals of DBT, which include the following:
- improve the patient's skills and motivation
- extend their newly formed skills to the environment
- enhance and maintain the patient's motivation to change
- increase the psychotherapist's motivation and skills
- structure the environment to optimize treatment delivery and execution (DeCou et al., 2019; Falcone & Timmons-Mitchell, 2018; NIMH, 2019; Prada et al., 2018)
Since DBT was initially intended for patients with a risk of suicide, it seeks systematically and comprehensively to treat issues in order of their severity; this preserves patient safety and ensures all concerns are addressed. Based on this understanding, DBT involves four major stages, as described in Table 2. There is no timeline for moving through the stages; some stages may be repeated, and the stages are not chronological. However, most patients begin at stage 1 (GoodTherapy, 2018a; McCain et al., 2018; Psychotherapy Academy, 2020).

DBT approaches are implemented with an ongoing effort to maintain a dialectical balance between accepting reality and changing behaviors. To bridge this gap, DBT employs five core components to balance behavioral change, assist with problem-solving, and regulate emotions:
- capability enhancement (i.e., skills training)
- generalization (i.e., techniques to encourage the transfer and application of skills learned to home, family, and work)
- motivational enhancement (i.e., individual behavioral treatment plans to reduce problematic behaviors)
- capability and motivational enhancement of the psychotherapist (i.e., to cope with burnout)
- structuring of the environment (i.e., to ensure positive, adaptive behaviors are reinforced across all environmental settings)
Skills training includes four essential domains: emotional regulation, mindfulness, interpersonal effectiveness, and distress tolerance. Emotional regulation teaches patients to deal with their primary emotional response before it induces a chain of adverse and distressing secondary reactions. Patients learn to recognize emotions, avoid emotional urges, and solve problems in useful ways. Mindfulness in DBT is centered on creating awareness and acceptance of the present. It helps patients identify and accept their thoughts and feelings without judgment and teaches them to become more mindful by balancing rational thoughts with emotions, taking effective action, and employing skills regularly. Interpersonal effectiveness emphasizes rational thinking, regulating intense emotions and rapid mood changes, and learning how to work through conflict and challenges. Interpersonal effectiveness combines listening skills, psychosocial skills, and assertiveness training to build greater self-respect and solve disputes more constructively. Finally, distress tolerance training refers to strategies such as distraction, relaxation techniques, and self-soothing methods to mitigate harmful behaviors (e.g., angry outbursts, self-harm, or substance abuse; GoodTherapy, 2018a; NIMH, 2019; Prada et al., 2018).
Mindfulness-Based Cognitive Therapy (MBCT)
MBCT is a more recent form of CBT developed by the collaborative efforts of Zindel Segal, Mark Williams, and John Teasdale. The first clinical trial data were not published until the beginning of the 21st century. MBCT was initially developed as a relapse-prevention treatment for depression that encouraged patients to change the function rather than the content of negative thoughts. Patients with a history of depression experience a poor mood, negative memories, and unhelpful cognitive patterns, triggering the reoccurrence of depressive symptoms. Several RCTs have demonstrated the clinical utility and efficacy of MBCT for patients with depression who have endured multiple relapses. In a 2020 systematic review and meta-analysis by McCartney and colleagues, including 14 RCTs (n=2,077), MBCT showed a statistically significant advantage over TAU and the placebo group in preventing depression relapse. Researchers determined MBCT was more effective than TAU in the long-term prevention of depression relapse and had statistically significant advantages over TAU and placebo regarding the time to relapse (McCartney et al., 2020). It has also been successfully applied to patients with chronic pain conditions (e.g., fibromyalgia). Furthermore, studies have also demonstrated that when applied to patients with chronic illnesses such as cancer, heart disease, or diabetes, such patients have shown improvements in their overall well-being (Craske, 2017; Stein, 2020).
MBCT integrates traditional CBT interventions with a mindfulness-based stress reduction (MBSR) modality, an 8-week program designed to help patients cope with the physical and mental impact of health concerns. MBCT helps patients focus on the present moment in a nonjudgmental and accepting manner. It does not seek to modify or eliminate dysfunctional thoughts. Instead, it focuses on assisting patients to become more detached and observe their thoughts objectively, without necessarily attempting to change them. MBCT focuses on developing mindfulness through a series of meditation, imagery, experiential exercises, and relaxation techniques. As highlighted earlier, a few psychotherapy models (DBT and ACT) integrate mindfulness but have slight variations in their utility. Unlike MBCT, DBT and ACT do not teach the principles of mindfulness meditation but instead apply mindfulness exercises to promote awareness and focus attention on the cognitions experienced during a state of mindfulness (Craske, 2017; Stein, 2020).
MBCT teaches patients how to view themselves as distinct from negative thoughts by employing cognitive methods and meditation to interrupt the automatic processes that re-trigger these feelings. This approach emphasizes changing one's reaction to unwanted thoughts, not the content of the thoughts themselves. A judgment of undesirable cognitions creates powerful secondary emotions (e.g., low mood, hopelessness, sadness). Patients learn to distance themselves from these thoughts by engaging in a greater awareness of how they practice judgment. Mindfulness teaches patients to break this cycle by continually refocusing on making deliberate choices to improve how they critique their thoughts. While the delivery of MBCT varies, it is most commonly used in a group setting with weekly sessions lasting 60 to 120 minutes for 8 weeks. Group sessions are accompanied by 30- to 45-minute homework assignments 6 times per week. Homework assignments help the patient develop and practice mindfulness meditation techniques, usually through audio or video recordings. Since the definition of mindfulness can vary across clinical applications, it is difficult to conceptualize a model of mindfulness meditation that applies to all patients; therefore, most sources describe this concept as the practice of developing a deeper awareness of one's mind and body without judgment and in the present moment. Specific strategies may include yoga, breathing meditations and exercises, and walking, among others (Parsons et al., 2017).
Problem-Solving Therapy (PST)
PST is a structured cognitive-behavioral intervention that strives to improve a person’s ability to prevent and cope with stressful life experiences by equipping them with various affective, cognitive, and behavioral tools. PST focuses on developing specific coping skills for problem areas and is particularly effective for stress management and depression. Most sources describe PST as a type of CBT-based psychotherapy, but some argue that problem-solving is the core of PST, and cognitive restructuring is often omitted. As cited in a 2018 meta-analysis by Cuijpers and colleagues, PST is a highly examined psychotherapeutic intervention for managing depression in adults and is comparable to other psychological treatments for depression. PST has also demonstrated efficacy in managing anxiety disorders, including phobias (e.g., social phobia, agoraphobia), HIV-risk behaviors, drug abuse, suicidal behaviors, childhood aggression, and conduct disorders. In a systematic review and meta-analysis including 11 studies and 2,072 participants, Zhang and colleagues (2018) demonstrated an overall significant treatment effect from PST with meaningful improvements in symptomology when applied to patients with depression and anxiety disorders treated in primary care settings (Zhang et al., 2018).
PST offers a flexible therapeutic approach and is employed in a group setting or on an individual basis. It is often used as part of a larger treatment plan, helping patients overcome barriers associated with nonadherence to medical or psychological treatments (e.g., adhering to weight-loss programs, medication compliance). Through a collaborative relationship with the psychotherapist, patients engage in active problem-solving activities. Specific PST interventions include psychoeducation, interactive problem-solving skills training exercises, homework assignments, and practice opportunities. Patients learn how to identify and prioritize key problem areas and break them into manageable tasks to develop appropriate coping behaviors and solutions. PST focuses on empowering patients to learn how to solve problems on their own. Therapy may range from 4 to 12 individual sessions, depending on patient needs, with an average of 45 to 60 minutes per session. While there are different styles of PST, they are all premised on the same principle of resolving depression by engaging the patient in active problem-solving activities. PST typically involves the following seven stages:
- selecting and defining the problem
- establishing realistic and achievable goals for problem resolution
- generating alternative solutions
- implementing decision-making guidelines
- evaluating and choosing solutions
- implementing the preferred solutions
- evaluating the outcome (Craske, 2017; Falcone & Timmons-Mitchell, 2018; Suicide Prevention Resource Center, 2017)
Acceptance and Commitment Therapy (ACT)
ACT is a newer form of psychotherapy developed by Steven Hayes in 1982 as a mixed approach to CBT. Since its inception, a relatively substantial evidence base has accrued regarding its clinical utility, highlighting its efficacy for anxiety and depression. However, there are not enough robust meta-analyses to conclude that it is more effective than traditional CBT (Hacker et al., 2016). ACT has also been increasingly studied in managing chronic pain, with at least 3 published systematic reviews and meta-analyses supporting the effectiveness of ACT and psychological flexibility on chronic pain perception. Favorable findings also demonstrate the proposed cost-effectiveness of ACT but insufficient evidence to establish firm conclusions (Feliu-Soler et al., 2018)
ACT is an action-oriented, process-based intervention that promotes mindfulness techniques to achieve psychological flexibility and help patients live more authentic lives. Psychological flexibility refers to being present, being open-minded, and acting consistently with core beliefs. Unlike traditional CBT, the goal of ACT is not to challenge or replace distorted thoughts and feelings; instead, it encourages patients to shift their perception to develop a new and positive relationship with these cognitions. Patients learn the consequences of avoiding, denying, and suppressing their inner emotions. By recognizing these challenges and accepting their feelings as appropriate responses to life events, patients learn how to behave in ways consistent with their values. ACT encourages patients to acknowledge unwanted emotional experiences as unavoidable aspects of life and forgo viewing them as problems or symptoms. It promotes acceptance of circumstances as they come without attempting to change inevitable things. To achieve psychological flexibility, ACT teaches six core processes that interconnect (see Table 3): acceptance, cognitive defusion, being present, self as context, values, and committed action (Association for Contextual Behavioral Science [ACBS], n.d.; Hacker et al., 2016).

ACT teaches the value of creating hopelessness through which prior attempts at solving unwanted emotions are explored, illuminating the lack of workability through these endeavors. Mindfulness increases a person’s ability to detach from unwanted thoughts, reducing painful feelings, urges, or situations before they are eventually accepted. Once patients recognize that these factors are beyond their control, they can focus on engaging in goal-directed behaviors. ACT emphasizes value clarification—or identifying personal values, beliefs, and desires—which direct patients toward generating value-guided action (i.e., intentional and effective behavior change; ACBS, n.d.; Hacker et al., 2016; Stein, 2020).
Psychiatric Behaviorism
Most behavioral techniques used in psychotherapy are based on the principles of classical conditioning developed by Ivan Pavlov in 1927. Classical conditioning stems from Pavlov's famous work with dogs, assuming that dysfunctional behaviors result from conditioned responses. When proposing classical conditioning, Pavlov demonstrated that he could generate a specific reaction from the dogs (i.e., salivation) by performing a particular action (i.e., ringing a distinctive bell). Variations of conditioning techniques have been employed for decades across rats, primates, and humans to remedy dysfunctional behaviors by replacing them with more desirable behaviors. Several methods have expanded upon Pavlov's early research to treat various emotional and psychological disorders such as phobias, anxiety disorders, and OCD. Furthermore, such practices have been applied to achieve specific behavioral modifications such as control of bedwetting and smoking cessation. Examples of some of the most common conditioning techniques currently used in practice include aversion therapy, counterconditioning, and systematic desensitization (GoodTherapy, 2015a; Hofmann & Asmundson, 2017; Wampold, 2019).
Counterconditioning and Systematic Desensitization
Counterconditioning and systematic desensitization often go hand-in-hand. They are commonly used to mitigate social phobias for large animals (i.e., dogs, horses). Counterconditioning refers to changing how a person or animal feels about something they fear or dislike. Systematic desensitization involves progressively exposing the subject to the feared stimulus in small but increasing amounts that don't trigger fear. For humans, counterconditioning and systematic desensitization are primary treatment modalities for phobias, OCD, sexual disorders, and other anxiety disorders. The patient learns to relax while being exposed to progressively more anxiety-provoking stimuli. Flooding is an element of desensitization that uses repeated exposure to highly distressing stimuli until the lack of reinforcement of the anxiety response can prompt the resolution of symptoms.
Systematic desensitization consists of 3 consecutive steps: relaxation training, hierarchy construction, and desensitization of stimulus. The patient is first taught relaxation training to generate physiologic effects that counteract anxiety. Strategies to promote relaxation include hypnosis, meditation, yoga, breathing exercises, or progressive muscle relaxation. Hierarchy construction refers to the creation of a list that includes all of the conditions that elicit anxiety. The patient generates a hierarchical list of all the events surrounding the anxiety-provoking event, listed in order of increasing anxiety. For example, if a patient has a phobia of dogs, they would rank the hierarchy of events associated with a fear of dogs as follows:
- Discuss an interaction with a dog with the psychotherapist.
- Look at a picture of a dog.
- Walk to the dog park.
- Open the gate to the dog park.
- Walk into the dog park.
- Leave the dog park before a dog approaches.
- Re-enter the dog park with a trusted person.
- Take a step toward a dog with a trusted person.
- Pet a dog with a trusted person.
- Pet the dog alone.
Desensitization of the stimulus is the final step in which the patient processes systematically through the hierarchical list, from the least to the most anxiety-provoking event while in a deeply relaxed state. Following the guidance of the psychotherapist, the patient starts to travel through the list while in a relaxed state, thereby generating a new and conditioned response to the phobia to replace the fear. On average, systematic desensitization occurs over 6 to 8 sessions, but research suggests that the longer the technique takes, the more effective it is (Hofmann & Asmundson, 2017; McLeod, 2021; Wampold, 2019).
Aversion Therapy
Aversion therapy (sometimes called aversive condition) is a specific type of counterconditioning that encourages individuals to give up undesirable habits by associating them with unpleasant effects. Drug and alcohol treatment programs sometimes integrate aversion techniques into their treatment plans. The most common example incorporates the use of disulfiram (Antabuse). When a patient takes disulfiram (Antabuse) and then consumes alcohol, they experience unwanted and uncomfortable side effects such as nausea, vomiting, tachycardia, palpitations, severe headaches, and shortness of breath. Disulfiram (Antabuse) is repeatedly paired with alcohol until the patient links alcohol consumption with these unpleasant feelings, thereby diminishing the patient's desire to consume alcohol. Disulfiram (Antabuse) creates a conditioned aversion to alcohol because it replaces the initial pleasurable response with an unpleasant effect. Electric shock therapy is another form of aversion therapy used to help reduce or eliminate cravings for drugs or other substance abuse disorders. Aversion therapy is considered a highly controversial treatment and has received significant scrutiny regarding the ethics of employing such strategies. For example, aversion therapy has been used as part of conversion therapy. This unethical form of therapy is designed to “convert” homosexual individuals to heterosexual by delivering shocks to a patient’s genitalia or inducing vomiting in association with sexualized images of the same gender. Conversion therapy has been administered to individuals who identify as transgender to “convert” them to their birth gender. Over the last decade, conversion therapy practices have drawn significant criticism and legal action (GoodTherapy, 2015a; Hofmann & Asmundson, 2017; Patra, 2016; Wampold, 2019).
Behavioral Activation (BA)
BA is chiefly indicated for those suffering from depression, presupposing that cognitions are sources of avoidance that sustain depressive symptoms. Research demonstrates that when people feel depressed, they have an increased tendency to disengage from (or avoid) everyday routines and withdraw from social environments. Over time, avoidant behaviors worsen depression as people isolate and lose opportunities for positive reinforcement. A Cochrane review of 53 RCTs involving 5,495 participants evaluated the effects of BA compared to those other psychological therapies, medications, and treatments for depression in adults. Findings revealed no difference in short-term treatment efficacy between BA and CBT based on moderate-certainty evidence, but BA was more efficacious than medication therapy. Not enough data were available to make direct comparisons with other forms of psychotherapy, specifically psychodynamic, interpersonal, and integrative therapies (Hofmann & Asmundson, 2017; Uphoff et al., 2020).
BA involves a technique that targets the connection between behavior, feelings, and depression (see Figure 2). BA is considered a critical and powerful CBT skill for treating depression. It helps patients understand how their behaviors influence their emotions and envision how they can control this process. BA seeks to increase behaviors that bring a patient into contact with positive reinforcements and decrease behaviors that impede contact with positive reinforcement. BA assumes that action precedes emotions. Activation changes an individual's brain state, a concept referred to as reinforcing positive context contingencies. The simplest example of this concept is engaging in cardiovascular exercise (e.g., running) to induce an endorphin release (i.e., endogenous chemicals produced by the body to relieve pain) into the bloodstream, which improves mood. The more an individual activates a specific behavior that derives a perceived benefit, the more situations they will experience that lead to positive emotions. BA focuses on positive reinforcement by increasing a patient's contact with rewarding and pleasant experiences, social activities, or mastery skills. This approach also teaches patients how to identify processes that inhibit activation and encourage avoidant behaviors, encouraging problem-solving skills (Hofmann & Asmundson, 2017; Uphoff et al., 2020).

BA effectively treats depression by generating a balance of goals centered on values, pleasure, and mastery. Patients track their activities and identify the affective and behavioral consequences of such actions. Activity monitoring creates awareness of and insight into underlying behaviors that negatively impact mood. It explores three fundamental elements of behavior change: the patient's values (i.e., things they find meaningful), pleasures (i.e., enjoyable activities or hobbies), and mastery (i.e., actions such as work or sports that involve the development of new skills, a sense of accomplishment, and a feeling of mastery over the environment; Craske, 2017; Stein, 2020). Brief Behavioral Activation Treatment for Depression (BATD) is a type of BA specifically designed to treat depression. The core components of BATD include the following:
- understanding the cyclic nature of depression
- identifying goals and values
- activity and mood monitoring (e.g., tracking moods across activities throughout the day, week, or month)
- building motivation and energy in a stepwise approach by incorporating pleasure and mastery of skills
- activity scheduling (i.e., purposefully scheduling enjoyable and meaningful activities)
- reducing avoidant behaviors
- completing between-session assignments or tasks (e.g., meeting small scale goals by practicing the target behavior; Craske, 2017; Society of Clinical Psychology, 2016; Uphoff et al., 2020)
BA typically occurs over 20 to 24 sessions, but BATD is shorter, lasting for 8 to 15 sessions (Society of Clinical Psychology, 2016).
Psychoanalysis
Psychoanalysis—the first form of psychotherapy—was initially developed by Sigmund Freud in the early 20th century. Freud believed most psychological problems resulted from repressed impulses and trauma endured during childhood. He believed human behavior was motivated by instincts and that the mind functions on three levels of consciousness: the conscious, preconscious, and unconscious. Later, he advanced his model of the mind to include the id, ego, and superego, as detailed in Table 4 (GoodTherapy, 2017b).

Freud believed that people could be cured by making unconscious thoughts and motivations conscious. The role and utility of psychoanalysis have been modified and expanded upon since Freud's early work. Modern-day psychoanalytic therapies center on changing a patient’s problematic behaviors, feelings, and thoughts by uncovering and exposing their unconscious meanings and motivations. The main objective is to bring unconscious material into consciousness and enhance the ego's functioning, helping the patient become less controlled by biological drives or demands of the superego. Treatment focuses on bringing the repressed conflict to consciousness, thereby allowing the patient can address it. Unlike CBTs, which are time-limited, psychoanalysis is long-term and typically extends for years. It fosters a longstanding partnership between the psychotherapist and the patient through which the patient reveals a great deal about themselves. The concept of transference is prominent in psychoanalysis, in which the patient transfers all the positive or negative emotions associated with their other relationships or underlying issues to the psychoanalyst. For example, if a patient is undergoing psychoanalysis with a psychotherapist for many years, they may view the therapist as a mother figure over time. Eventually, the patient transfers feelings about their mother onto the therapist, perhaps to gain the love and attention she did not receive from her mother. Other core psychoanalytic techniques include free association, dream analysis, and resistance analysis, as outlined in Table 5 (GoodTherapy, 2017b; Hofmann & Asmundson, 2017; Wampold, 2019).

Psychodynamic Psychotherapy
Psychodynamic psychotherapy is grounded in the principles of psychoanalysis but was created as a simpler, more concise alternative. Psychodynamic therapy can be used as a short-term or long-term therapy. Brief psychodynamic therapy is goal-oriented and takes an average of 25 sessions, whereas long-term psychodynamic therapy may last for more than 2 years. Psychodynamic psychotherapy is indicated when a patient's problems are linked to unconscious factors that lead to interpersonal difficulties, maladaptive coping, and distorted self-perceptions. Research demonstrates the clinical efficacy of this approach when offered to patients with depression, anxiety, or trauma. Psychodynamic psychotherapy addresses the foundation and formation of psychological processes to reduce distressing symptoms and improve QOL. Psychodynamic psychotherapy analyzes the impact of life events (particularly early life experiences) on current issues. It focuses on making the unconscious conscious, thereby helping patients acquire insight into their lives and current problems by drawing on emotions, thoughts, experiences, and core beliefs. Similar to psychoanalysis, the therapeutic relationship between the patient and the psychotherapist is vital. Patients learn about themselves by exploring their interactions in the therapeutic relationship (PsychDB, 2021b).
This approach targets identifying compromises patients have made to protect themselves against painful thoughts or emotions, which may serve as unconscious defense mechanisms. By recognizing patterns, patients learn how they have avoided distress and developed maladaptive (defensive) coping mechanisms. Defense mechanisms can inadvertently sustain painful thoughts, memories, and feelings in the unconscious. Three of the most common defense mechanisms include denial, rationalization, and repression. Denial refers to the rejection of a fact, experience, or event that is too painful for an individual to accept. Repression is similar to denial in that a painful thought, memory, or feeling is unconsciously pushed outside an individual's realm of consciousness. Over time, the individual becomes unaware of its existence, but the repressed memory can still affect their behavior. Rationalization refers to an attempt to justify immoral, deviant, or generally unacceptable behavior logically. By encouraging patients to speak freely about these emotions and fears, therapists help them acquire insight into defense mechanisms to change certain behaviors (GoodTherapy, 2015b, 2016, 2018c).
Interpersonal Psychotherapy (IPT)
IPT is a structured, evidence-based treatment that draws upon the principles of psychodynamic therapy to focus on interpersonal difficulties that lead to psychological problems. IPT was designed as a brief intervention for patients with depression, with the primary objective of improving relationships to alleviate depression. Although a specific event or relationship may not cause depression, depression commonly affects relationships and creates interpersonal problems. Meta-analyses have demonstrated that IPT works at least as well as other psychotherapies for treating depression. Cuijpers and colleagues (2016) performed a meta-analysis of 14 RCTs comparing IPT with other psychotherapies (BA, CBT, PST, psychodynamic psychotherapy). Findings demonstrated that IPT produced comparable benefits and clinical efficacy in patients with depression and eating disorders. For those with anxiety disorders, IPT was as effective as TUA, and IPT did not appear less effective than CBT (Cuijpers et al., 2016).
IPT is an adaptive and versatile treatment that is easily modified for disorders, demonstrating efficacy for SUD, bipolar disorder, and postpartum depression. Treatment is present-focused (e.g., on psychological difficulties sparked by recent conflicts or transitions), but aspects of attachment theory are used to analyze how past relationships affect current relationships. Attachment theory maintains that the relationship between a caregiver and infant is crucial to survival and remains essential throughout life. A secure attachment early in life provides a strong foundation for psychological security and healthy intimacy in adult relationships. In contrast, early disturbances in attachment increase a person’s vulnerability to depression and other psychological difficulties, particularly interpersonal relationships. IPT teaches patients to evaluate their interactions to build an awareness of how they relate to others. The short-term goals of IPT are to achieve a rapid reduction of symptoms and improve social adjustment, whereas the long-term goal is to help patients learn how to make necessary adjustments independently in the future (Lebow, 2021; Swartz et al., 2021).
This approach targets the social and interpersonal context of a patient's problems. IPT focuses on the present and highlights the patient’s interpersonal life in 4 problem areas:
- role disputes (conflicts with significant others, non-reciprocal expectations between individuals)
- interpersonal skill deficits (communication shortfalls, impaired social skills, social isolation, series of unfulfilling relationships)
- grief over loss (death of a close contact, loss of an intimate relationship)
- role transitions (changing roles, such as going from working to retiring or from married to divorced; Lebow, 2021; Swartz et al., 2021)
IPT is typically limited to 3 or 4 months (up to 20 sessions) and is organized into three session groups (opening, middle, and final), as outlined in Table 6). IPT can be administered as a sole form of therapy or in conjunction with medications. Most studies indicate that the combination of medication and IPT may be more beneficial than either method alone. Psychotherapists may employ techniques such as role-playing to help patients understand and adjust how they relate to their world (Craske, 2017; GoodTherapy, 2018b; Stein, 2020).

Refrences
American Psychiatric Association. (2019). What is psychotherapy? https://www.psychiatry.org/patients-families/psychotherapy
American Psychiatric Association. (2020a). APA dictionary of psychology. https://dictionary.apa.org/
American Psychiatric Association. (2020b). Understanding psychotherapy and how it works. https://www.apa.org/topics/psychotherapy/understanding
Angermeyer, M. C., van der Auwera, S., Carta, M. G., & Schomerus, G. (2017). Public attitudes toward psychiatry and psychiatric treatment at the beginning of the 21st century: A systematic review and meta-analysis of population surveys. World Psychiatry, 16, 50-61. http://doi.org/10.1002/wps.20383
Association for Contextual Behavioral Science. (n.d.). The six core processes of ACT. Retrieved April 15, 2021, from https://contextualscience.org/the_six_core_processes_of_act
Children’s Bureau. (2018). Trauma-focused cognitive-behavioral therapy: A primer for child welfare professionals. US Department of Health and Human Services. https://www.childwelfare.gov/pubPDFs/trauma.pdf
Cook, S. C., Schwartz, A. C., & Kaslow, N. J. (2017). Evidence-based psychotherapy: Advantages and challenges. Neurotherapeutics, 14, 537-545. https://doi.org/10.1007/s13311-017-0549-4
Craske, M. G., (2017). Cognitive-behavioral therapy (2nd ed.). American Psychiatric Association.
Cuijpers, P., Donker, T., Weissman, M. M., Ravitz, P., & Cristea, I. A. (2016). Interpersonal psychotherapy for mental health problems: A comprehensive meta-analysis. American Journal of Psychiatry, 173(7), 68-687. https://doi.org/10.1176/appi.ajp.2015.15091141
Cuijpers, P., de Witt, L., Kleiboer, A., Karyotaki, E., & Ebert, D. D. (2018). Problem-solving therapy for adult depression: An updated meta-analysis. European Psychiatry, 48, 27-37. https://doi.org/10.1016/j.eurpsy.2017.11.006
Cuijpers, P. (2019). Targets and outcomes of psychotherapies for mental disorders: An overview. World Psychiatry, 18(3), 276-285. https://doi.org/10.1002/wps.20661
David, D., Cristea, I., & Hofmann, S. G. (2018). Why cognitive behavioral therapy is the current gold standard of psychotherapy. Frontiers in Psychiatry, 9(4). https://doi.org/10.3389/fpsyt.2018.00004
DeCou, C. R., Comtois, K. A., & Landes, S. J. (2019). Dialectical behavior therapy is effective for the treatment of suicidal behavior: A meta-analysis. Behavior Therapy, 50(1), 60-72. https://doi.org/10.1016/j.beth.2018.03.009
Espinoza, R. T., & Unutzer, J. (2019). Diagnosis and management of late-life unipolar depression. UpToDate. Retrieved April 15, 2021, from https://www.uptodate.com/contents/diagnosis-and-management-of-late-life-unipolar-depression
Falcone, T., & Timmons-Mitchell, J. (Eds.). (2018). Suicide prevention: A practical guide for the practitioner. Springer. https://doi.org/10.1007/978-3-319-74391-2
Feliu-Soler, A., Montesinos, F., Gutierrez-Martinez, O., Scott, W., McCracken, L. M., & Luciano, J. V. (2018). Current status of acceptance and commitment therapy for chronic pain: A narrative review. Journal of Pain Research, 11, 2145-2159. https://doi.org/10.2147/JPR.S144631
Feng, G., Han, M., Li, X., Geng, L., & Miao, Y. (2020). The clinical effectiveness of cognitive-behavioral therapy for patients with insomnia and depression: A systematic review and meta-analysis. Evidence-Based Complementary and Alternative Medicine, 8071821, 1-14. https://doi.org/10.1155/2020/8071821
GoodTherapy. (2015a). Aversion therapy. https://www.goodtherapy.org/learn-about-therapy/types/aversion-therapy
GoodTherapy. (2015b). Repression. https://www.goodtherapy.org/blog/psychpedia/repression
GoodTherapy. (2016). Rationalization. https://www.goodtherapy.org/blog/psychpedia/rationalization
GoodTherapy. (2017a). Eye movement desensitization and reprocessing therapy (EMDR). https://www.goodtherapy.org/learn-about-therapy/types/eye-movement-desensitization-and-reprocessing
GoodTherapy. (2017b). Psychoanalysis/modern psychoanalysis. https://www.goodtherapy.org/learn-about-therapy/types/psychoanalysis
GoodTherapy. (2018a). Dialectical behavior therapy (DBT). https://www.goodtherapy.org/learn-about-therapy/types/dialectical-behavioral-therapy
GoodTherapy. (2018b). Interpersonal therapy (IPT). https://www.goodtherapy.org/learn-about-therapy/types/interpersonal-psychotherapy
GoodTherapy. (2018c). Psychodynamic therapy. https://www.goodtherapy.org/learn-about-therapy/types/psychodynamic
Hacker, T., Stone, P., & MacBeth, A. (2016). Acceptance and commitment therapy - Do we know enough? Cumulative and sequential meta-analyses of randomized controlled trials. Journal of Affective Disorders, 190, 551-565. https://doi.org/10.1016/j.jad.2015.10.053
Hofmann, S. G., & Asmundson, G. J. G. (2017). The science of cognitive-behavioral therapy. Elsevier.
Jensen, T. K., Holt, T., & Ormhaug, S. M. (2017). A follow-up study from a multisite, randomized controlled trial for traumatized children receiving TF-CBT. Journal of Abnormal Child Psychology, 45, 1587-1597. https://doi.org/10.1007/s10802-017-0270-0
Lebow, J. (2021). Overview of psychotherapies. UpToDate. Retrieved April 15,
2021, from
https://www.uptodate.com/contents/overview-of-psychotherapies
Luo, C., Sanger, N., Singhal, N., Pattrick, K., Shams, I., Shahid, H., Hoang, P., Schmidt, J., Lee, J., Haber, S., Puckering, M., Buchanan, N., Lee, P., Ng, K., Sun, S., Kheyson, S., Chung, D. C., Sanger, S., Thabane, L., & Samaan, Z. (2020). A comparison of electronically-delivered and face-to-face cognitive behavioural therapies in depressive disorders: A systematic review and meta-analysis. The Lancet, 24(100442). https://doi.org/10.1016/j.eclinm.2020.100442
McCain, S. F., Chapman, A. L., Kuo, J. R., Guimond, T., Streiner, D. L., Dixon-Gordon, K. L., Isaranuwatchai, W., & Hoch, J. S. (2018). The effectiveness of 6 versus 12 months of dialectical behavior therapy for borderline personality disorder: The feasibility of a shorter treatment and evaluating responses (FASTER) trial protocol. BMC Psychiatry, 18(230). https://doi.org/10.1186/s12888-018-1802-z
McCartney, M., Nevitt, S., Lloyd, A., Hill, R., White, R., & Duarte, R. (2020). Mindfulness-based cognitive therapy for prevention and time to depressive relapse: Systematic review and network meta-analysis. Acta Psychiatrica Scandinavica, 143(1), 6-21. https://doi.org/10.1111/acps.13242
McCurry, S. M., Zhu, W., Von Korff, M., Wellman, R., Morin, C. M., Thakral, M., Yeung, K., & Vitiello, M. V. (2021). Effect of telephone cognitive behavioral therapy for insomnia in older adults with osteoarthritis pain: A randomized clinical trial. JAMA Internal Medicine, 181(4), 530-538. https://doi.org/10.1001/jamainternmed.2020.9049
McLeod, S. (2021). Systematic desensitization as a counterconditioning process. https://www.simplypsychology.org/Systematic-Desensitisation.html
National Center for PTSD. (2017). 2017 clinical practice guidelines for the management of PSTD. https://www.ptsd.va.gov/professional/treat/txessentials/cpg_ptsd_management.asp
National Center for PTSD. (2020a). Cognitive processing therapy for PTSD. https://www.ptsd.va.gov/professional/treat/txessentials/cpt_for_ptsd_pro.asp
National Center for PTSD. (2020b). Eye movement desensitization and reprocessing (EMDR) for PTSD. https://www.ptsd.va.gov/professional/treat/txessentials/emdr_pro.asp
National Center for PTSD. (2020c). Prolonged exposure for PTSD. https://www.ptsd.va.gov/professional/treat/txessentials/prolonged_exposure_pro.asp#one
National Center for PTSD. (2021). Treatment essentials. https://www.ptsd.va.gov/professional/treat/txessentials/index.asp
National Institute of Mental Health. (2019). Suicide prevention. https://www.nimh.nih.gov/health/topics/suicide-prevention/index.shtml#part_153179
National Institute of Mental Health. (2021). Mental illness. https://www.nimh.nih.gov/health/statistics/mental-illness.shtml
Parsons, C. E., Crane, C., Parsons, L. J., Fjorback, L. O., & Kuyken, W. (2017). Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behaviour Research and Therapy, 95, 29-41. https://doi.org/10.1016/j.brat.2017.05.004
Patra, S. (2016). Conversion therapy for homosexuality: Serious violation of ethics. Indian Journal of Medical Ethics, 1(3), 194-195. https://doi.org/10.20529/IJME.2016.056
Prada, P., Perroud, N., Rufenacht, E., & Nicastro, R. (2018). Strategies to deal with suicide and non-suicidal self-injury in borderline personality disorder, the case of DBT. Frontiers in Psychology, 9, 2595. https://doi.org/10.3389/fpsyg.2018.02595
PsychDB. (2021a). Interpersonal therapy (IPT). https://www.psychdb.com/psychotherapy/ipt
PsychDB. (2021b). Psychodynamic psychotherapy. https://www.psychdb.com/psychotherapy/psychodynamic/home
Psychotherapy Academy. (2020). DBT online training: The 4 stages and targets of DBT. https://psychotherapyacademy.org/dbt/the-4-stages-and-targets-of-dbt/
Reynolds, M. E., & Cone, P. H. (2018). Managing adult insomnia confidently. The Journal for Nurse Practitioners, 14(10), 718-724.E1. https://doi.org/10.1016/j.nurpra.2018.08.019
Selchick, F. (2021). BA for depression [image].
Stein, M. B. (2020). Psychotherapy and psychosocial interventions for posttraumatic stress disorder in adults. UpToDate. Retrieved April 11, 2021, from https://www.uptodate.com/contents/psychotherapy-and-psychosocial-interventions-for-posttraumatic-stress-disorder-in-adults#H1772362614
Society of Clinical Psychology. (2016). Treatment: Behavioral activation for depression. https://div12.org/treatment/behavioral-activation-for-depression/
Substance Abuse and Mental Health Services Administration. (2020). 2019 national survey on drug use and health: Veteran adults. https://www.samhsa.gov/data/release/2019-national-survey-drug-use-and-health-nsduh-releases
Suicide Prevention Resource Center. (2017). Problem-solving therapy (PST). https://www.sprc.org/resources-programs/problem-solving-therapy-pst
Swartz, H. A., Roy-Byrne, P. P., & Soloman, D. (2021). Interpersonal psychotherapy (IPT) for depressed adults: Indications, theoretical foundation, general concepts, and efficacy. UpToDate. Retrieved April 11, 2021, from https://www.uptodate.com/contents/interpersonal-psychotherapy-ipt-for-depressed-adults-indications-theoretical-foundation-general-concepts-and-efficacy
Terlizzi, E. P., & Zablotsky, B. (2020). Mental health treatment among adults: United States, 2019. NCHS Data Brief, 380, 1-7. https://www.cdc.gov/nchs/data/databriefs/db380-H.pdf
Uphoff, E., Ekers, D., Robertson, L., Dawson, S., Sanger, E., South, E., Samaan, Z., Richards, D., Meader, N., & Churchill, R. (2020). Behavioural activation therapy for depression in adults. Cochrane Database of Systematic Reviews, 7, CD013305. https://doi.org/10.1002/14651858.CD013305.pub2
US Department of Veterans Affairs. (2019). 2019 national veteran suicide prevention annual report. https://www.mentalhealth.va.gov/docs/data-sheets/2019/2019_National_Veteran_Suicide_Prevention_Annual_Report_508.pdf
Wampold, B. E. (2019). The basics of psychotherapy: An introduction to theory and practice (2nd ed.). American Psychiatric Association.
Winkelman, J. W. (2021). Overview of the treatment of insomnia in adults. UpToDate. Retrieved April 15, 2021, from https://www.uptodate.com/contents/overview-of-the-treatment-of-insomnia-in-adults
Zhang, A., Park, S., Sullivan, J. E., & Jing, S. (2018). The effectiveness of problem-solving therapy for primary care patient’s depressive and/or anxiety disorders: A systematic review and meta-analysis. Journal of the American Board of Family Medicine, 31(1), 139-150. https://doi.org/10.3122/jabfm.2018.01.170270