About this course:
The purpose of this two-part educational series is to enhance clinical practice and improve patient outcomes by educating advanced practice registered nurses (APRNs) on the various types of diagnostic radiology imaging tests, ensuring satisfactory understanding of the appropriate indications for ordering each exam, as well as the risks, benefits, and important clinical considerations regarding the use of contrast media.
Course preview
This is a two-part educational series on diagnostic radiology. Part I will focus on the diagnostic imaging process, the components of imaging quality, a detailed account of several types of contrast agents, with regards to their clinical considerations, risks, monitoring parameters, and regimens for managing contrast allergies. Part II will proceed with an overview of radiation safety with diagnostic imaging, radioactive contrast agents used in nuclear medicine, the various modalities of diagnostic radiology testing, including their indications for use and an overview of the appropriate use criteria, essential components of patient education, as well as contraindications to testing.
By the completion of this module, the APRN should be able to:
- Discuss the various aspects of radiation, the essential components of radiation safety, and identify the amount of radiation in some of the most common imaging tests.
- Differentiate between the general risks of medical imaging tests with radiation exposure and those without radiation exposure, and briefly discuss the guidelines for diagnostic imaging during pregnancy and lactation.
- Recognize the components of the Appropriate Use Criteria for Advanced Diagnostic Imaging as devised by the Centers for Medicare & Medicaid Services.
- Describe the different types of diagnostic radiology tests and the indications for ordering, key patient teaching points, what to expect during the test, how long the test should take, as well as the associated risks and benefits.
The purpose of this two-part educational series is to enhance clinical practice and improve patient outcomes by educating advanced practice registered nurses (APRNs) on the various types of diagnostic radiology imaging tests, ensuring satisfactory understanding of the appropriate indications for ordering each exam, as well as the risks, benefits, and important clinical considerations regarding the use of contrast media.
Diagnostic radiology refers to a sector of medicine that includes various kinds of medical imaging technologies widely utilized throughout the US healthcare system, with millions of patients undergoing imaging evaluations on a daily basis. These are non-invasive and minimally invasive medical procedures used to view the inside of the body as a means to assess, diagnose, monitor, and treat a wide array of medical conditions. Several of these tests also serve as the backbone of preventative medicine and routine heath maintenance, including cancer prevention, screening, and early detection. While diagnostic radiology is a valuable and critical component to proper diagnosis of numerous medical conditions, they are not without risks. Many of these tests are linked to potential harms that must be considered prior to ordering the test, as well as a high cost burden to patients and society. To promote patient safety and safeguard optimal outcomes, clinicians have an obligation to ascertain an appropriate understanding of each type of imaging modality, as well as a keen awareness of the clinical risks, benefits, and management of adverse events (Elsayes & Oldham, 2014).
Radiation
Radiation is energy in the form of particles or waves emitted by both natural and synthetic sources. Comprised of two forms, ionizing and non-ionizing, radiation surrounds us in our daily lives. As demonstrated in Figure 1, radiation exists on the electromagnetic (EM) spectrum, ranging from lower energy microwaves to higher energy gamma rays. EM energy travels in waves, and the strength of the radiation depends on the frequency (how rapidly the waves move up and down) and the distance the wavelength is traveling. In general, the smaller the wavelength, the higher the energy of the radiation (The Centers for Disease Control and Prevention [CDC], 2015d).
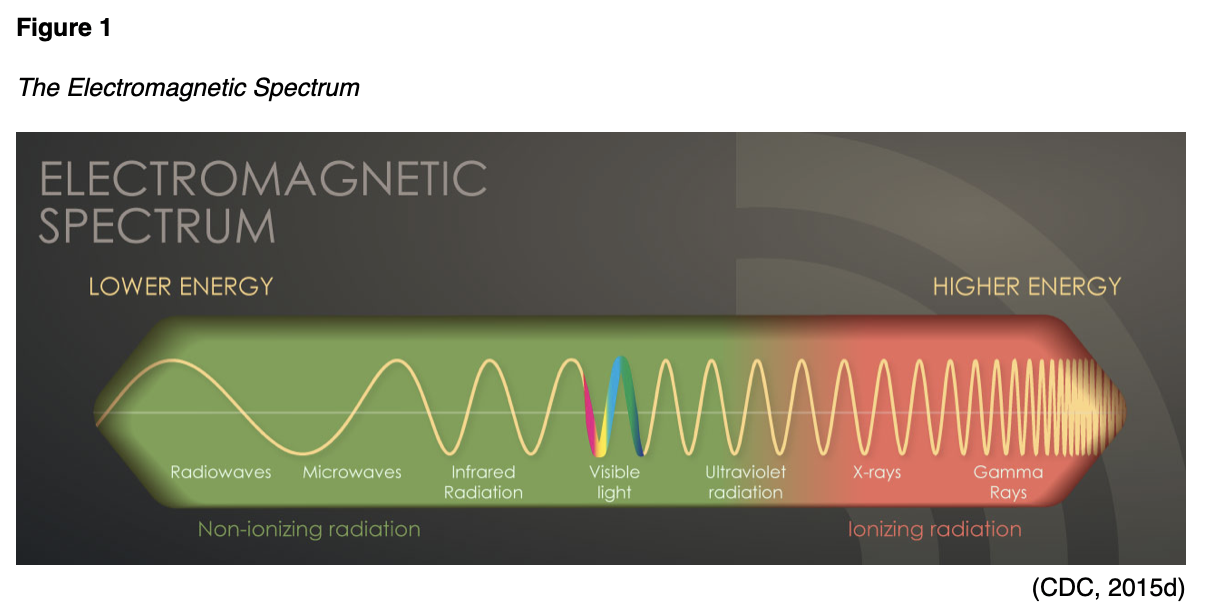
Non-ionizing radiation is the most prevalent form of radiation that is freely available in low levels within our environment. It can heat substances, yet it does not have the ability to remove electrons from atoms and molecules. The most common types of non-ionizing radiation include radiofrequency (RF) waves in many communication and electronic devices, kitchen microwaves, visible light, and lower energy forms of ultraviolet (UV) radiation. Intense, direct exposure to RF waves and microwaves can result in tissue damage due to heat. In contrast, overexposure to UV rays can result in skin burns, premature skin aging, eye damage, and skin cancer. The vast majority of skin cancers are directly related to intense, prolonged, and unprotected exposure to UV radiation from the sun and tanning beds. The line dividing ionizing and non-ionizing radiation becomes somewhat blurred in the UV section of the EM spectrum demonstrated in Figure 1. Radiation in the UV section at lower energies is considered non-ionizing, whereas, at higher energies, extreme UV radiation becomes more harmful, rendering it ionizing radiation (CDC, 2015d).
Ionizing radiation removes electrons from atoms and molecules, causing the atom to become ionized (or charged), thereby enabling the wavelengths to pass through air, water, and tissue. Ionizing radiation is considered a carcinogen, or a substance capable of causing cancer, as it can penetrate the human body (Agency for Healthcare Research and Quality [AHRQ], 2019). When absorbed by living tissue, ionizing radiation has the potential to induce harm, especially when exposed at high levels. Most humans are exposed to low levels of ionizing radiation daily, and these radiation sources may be natural or manmade (CDC, 2015a). Exposure can occur through construction and building materials, terrestrial radiation (radiation from the earth), cosmic radiation (radiation from space), and air travel (CDC, 2015d). Some people are exposed to higher amounts of natural background radiation, such as those who live at higher mountain elevations, as well as those who engage in frequent air travel (American College of Radiology [ACR], 2018). X-rays are the most classic example of ionizing radiation; they penetrate the body to visualize underlying bony structures. Ionizing radiation has enough energy to alter molecules within the cells of the human body, targeting genetic material, or DNA. Radiation interacts with DNA directly and indirectly, as it is capable of destroying bonds within the DNA and the water molecules that surround the DNA. When the water molecules are broken, they generate free radicals, or unstable oxygen molecules that damage cells, tissues, and organs (CDC, 2015d). When a cell is damaged from radiation exposure, one of the following three events will occur:
- The cell will repair itself and restore its normal function;
- The cell will remain altered, or only partially repair the damage, thereby heightening the risk for future cancer development;
- The cell will die, and your body will recover; however, if there is widespread cell death, this can increase the risk for organ failure (CDC, 2015b).
Risks with Medical Imaging
Many types of diagnostic radiology imaging tests and procedures involve exposure to ionizing radiation, which increases the risk of harmful effects. Some of the most common examples of imaging tests associated with the highest ionizing radiation exposure include x-rays, computed tomography (CT scans), fluoroscopy, and nuclear medicine scans. Ionizing radiation can penetrate deep into the body, and repeated exposure from imaging tests increases the risk for cancer later in life (CDC, 2019). Certain populations are more vulnerable to the harmful health effects of radiation exposure, such as infan
...purchase below to continue the course
The health effects associated with ionizing radiation are strongly linked to the dose. The radiation dose or the amount of radiation is the critical factor when evaluating the risk for future unintended health consequences, as the risks are dose-dependent. However, the amount of ionizing radiation that is absorbed by the body is what induces harm to health. At high doses, radiation can be lethal; at lower doses, it can lead to serious health consequences (CDC, 2015b). As described in Table 1, the radiation dose is not the same as a dose of standard medication. There are three principal ways in which radiation doses are measured: absorbed dose, equivalent dose, and effective dose.

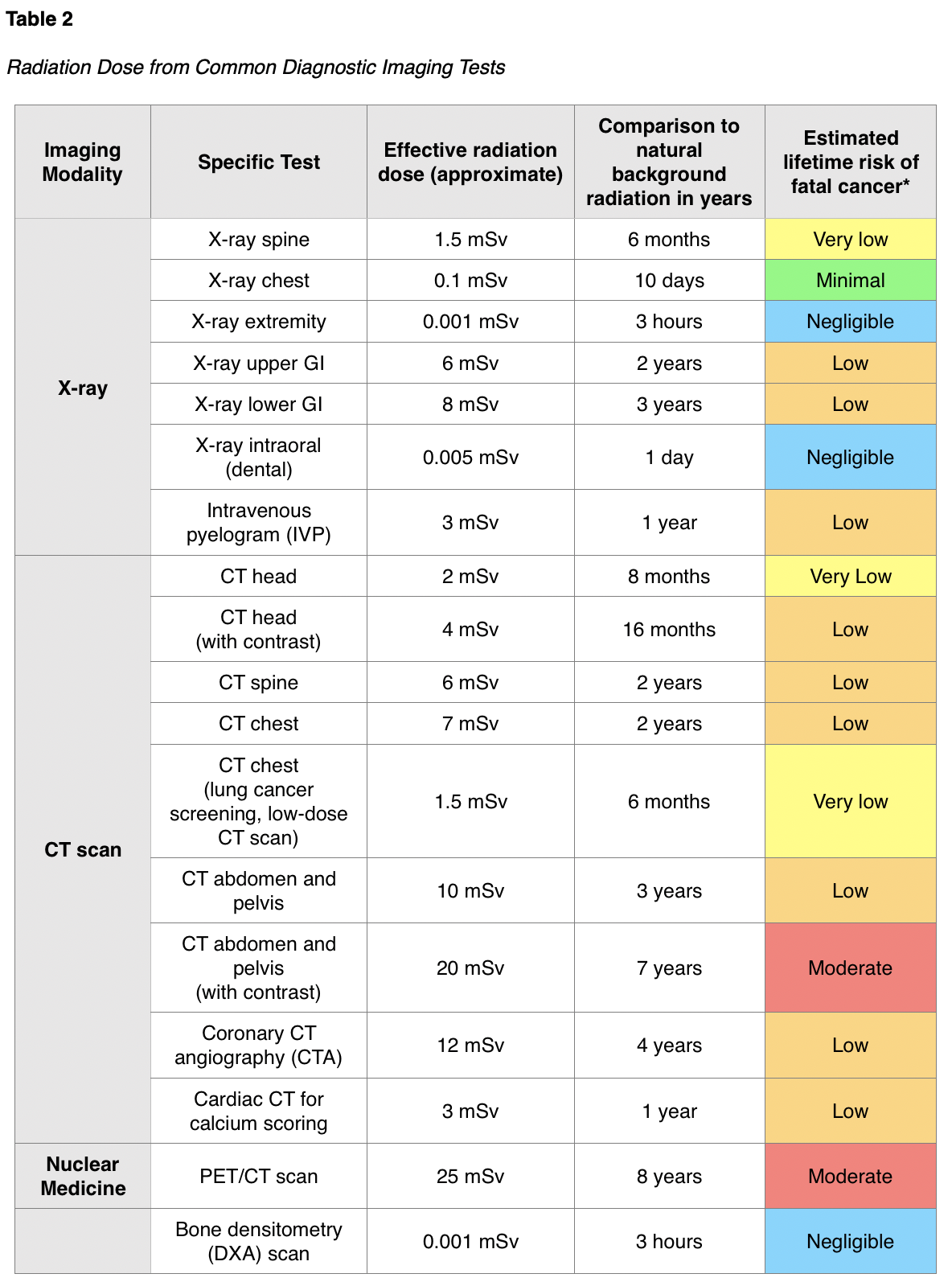
The absorbed dose and equivalent dose are used to evaluate the short-term effect of radiation on tissue, which ranges from weeks to months. When diagnostic imaging is performed correctly, there are generally no short-term effects; therefore, the absorbed and equivalent doses are less meaningful in clinical practice. For the majority of patients, the effective dose is the most important and useful dose quantity, since it applies to long-term effects (RadiologyInfo.org, 2018c). The speed at which the dose is administered also has implications on health and long-term effects. For example, if a person receives the radiation dose over an extended period, the impact on health will not be as severe as if the dose were received all at once (CDC, 2015b). The absorbed radiation dose varies widely based on the different types of examinations. Among the most common medical imaging tests, nuclear medicine scans such as the positron emission tomography – computed tomography (PET/CT) scan have the highest associated radiation exposure. A PET/CT scan is comparable to eight years of natural background radiation and poses a moderately increased (1 in 1,000 to 1 in 500) estimated lifetime risk of dying from fatal cancer. Table 2 provides a detailed overview of the radiation dose to adult patients associated with common diagnostic radiology imaging examinations, as well as a classification of risk levels. Further, the radiation dose varies based on the operator and the facility equipment as well (RadiologyInfo.org, 2015). Aside from increasing one's risk for future cancer development, ionizing radiation exposure can also contribute to the development of cataracts, skin reddening or skin burns, and hair loss. However, these health effects most commonly result from exposure to very high levels of radiation associated with radiation oncology treatment fields, which require a significantly higher dose of radiation delivered directly to a localized area of the body (CDC, 2019c).
Diagnostic Imaging During Pregnancy and Lactation
Diagnostic imaging during pregnancy and lactation is a controversial topic with various opinions. In general, the most common documented adverse effects from high-dose radiation exposure on the developing fetus include growth restriction, microcephaly, and intellectual disability. The American College of Obstetricians and Gynecologists [ACOG] Committee on Obstetric Practice (2017) makes the following recommendations regarding diagnostic imaging procedures during pregnancy and lactation:
- Ultrasound and magnetic resonance imaging (MRI) are the imaging techniques of choice for the pregnant patient. Still, they should be used only when use is strongly predicted to provide medical benefit to the mother or fetus.
- The majority of radiation exposure through CT scan or nuclear medicine imaging is provided at a dose that is considered much lower than the exposure associated with fetal harm. If these techniques are deemed medically necessary, they should not be withheld solely based on pregnancy.
- Iodinated contrast: it generally is recommended that contrast only be used if required to obtain essential additional diagnostic information that will affect the care of the fetus or mother during the pregnancy. Breastfeeding can be continued without interruption following the use of iodinated contrast materials.
- Gadolinium contrast: the use of gadolinium contrast with MRI should be limited, and it should be used only if it significantly improves the predicted diagnostic outcomes for the fetus or mother. Breastfeeding should not be interrupted following gadolinium administration.
- Radioactive iodine: iodine-123 (I-123) and iodine-131 (I-131) readily crosses the placenta, and use should be avoided in pregnancy. If a thyroid scan is essential, it is recommended that the radioactive isotope technetium 99m is used.
- Since specific nuclear materials excreted into breast milk can have deleterious effects on the infant, consultation with experts in breastfeeding and nuclear medicine are recommended when these compounds are used in lactating women (ACOG, 2017).
Radiation Safety
While the potential for increased risk of adverse health effects from diagnostic imaging is clearly described, there is no universally recognized threshold for specific radiation dose and associated effects. Therefore, it has been argued that there is "no safe level" of radiation exposure. To safeguard patients, the priority measure is to ensure the potential risks of ionizing radiation is continuously weighed against the benefit derived from performing the imaging test or procedure. This is a clinical decision that should be made between the ordering provider and the patient with full disclosure of the potential risks of imaging from radiation exposure in comparison with the predicted benefits (ACR, 2018). The US Department of Labor Occupational Safety and Health Administration (OSHA, n.d.), outlines standards for controlling ionizing radiation hazards and preventing radiation exposure to both healthcare workers and patients. Diagnostic radiology departments within hospitals, as well as free-standing diagnostic radiology facilities, must implement radiation protection programs that are managed by a radiation safety officer (RSO), who is a qualified expert, such as a radiologist or a medical physicist. The radiology equipment is housed in designated areas within hospitals, usually on the ground floor, and secured behind lead doors to reduce exposure to employees and patients. Radiologists and radiology technicians must undergo specialized training in radiation safety practices, which are governed by both state and federal law. OSHA standards require appropriate radiation caution signage to alert individuals to radiation usage in designated areas, such as the x-ray caution sign displayed in Figure 2 (OSHA, n.d.)
A central concept of radiation protection programs is keeping each healthcare worker's occupational radiation dose as limited as possible by implementing "As Low As Reasonably Achievable" (ALARA) programs. ALARA is premised on three chief components of time, distance, and shielding as follows:
- Time: minimize the time spent in areas with elevated radiation levels;
- Distance: maximize the distance from sources of radiation, as a worker's radiation dose decreases as the distance from the source increases;
- Shielding: Use shielding for radiation sources (i.e., placing an appropriate shield between sources of radiation and the worker), Inserting the proper shielding (e.g., lead, concrete, or special plastic shields depending on the type of radiation) between a worker and a radiation source will greatly reduce or eliminate the dose received by the worker. Shielding also refers to lead doors and geographic locations within the facility to reduce exposure to other individuals who are not directly working within that environment (CDC, 2015c; OSHA, n.d.).
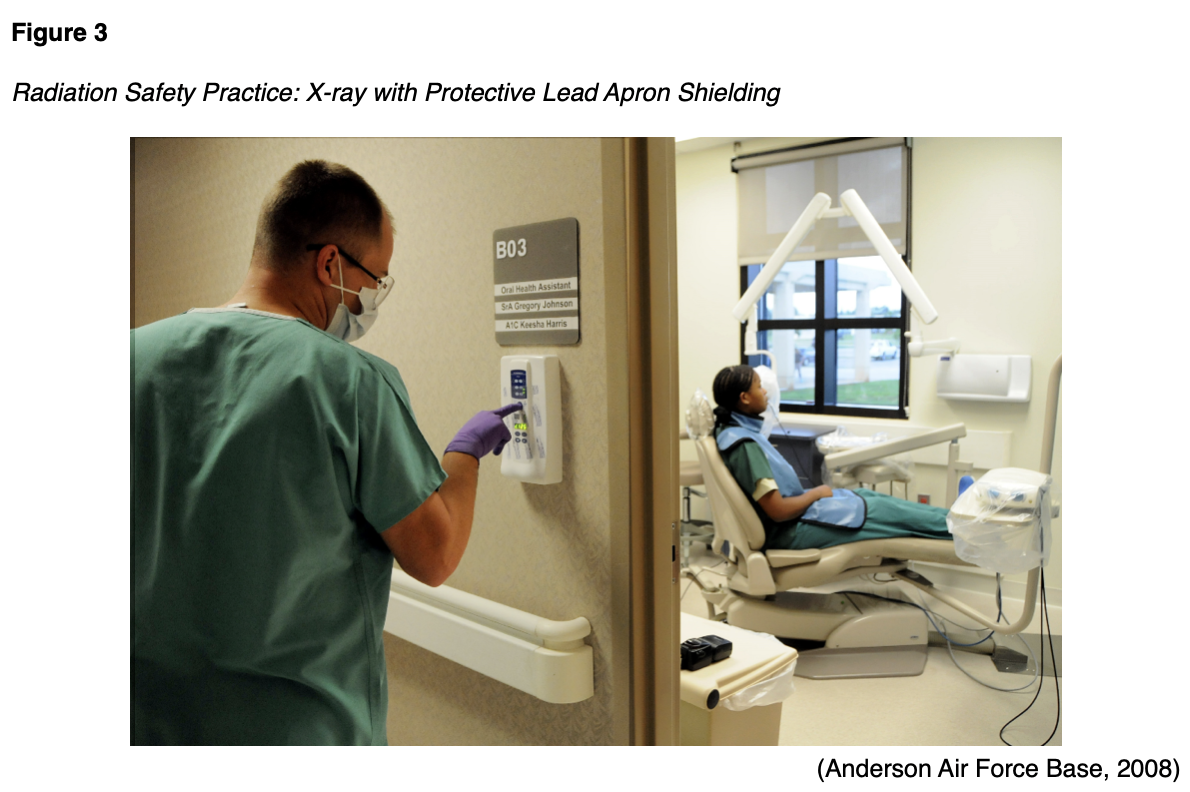
As demonstrated in Figure 3, shielding patients with lead aprons and lead coverings during diagnostic imaging tests has been the standard practice in diagnostic imaging since its endorsement by the US Code of Federal Regulations in 1976. This practice originated due to concerns related to hereditary risks with fertility (such as mutations in germ cells affecting future generations), and gonadal shielding was advised and implemented for all x-rays. Shielding has historically been justified as protection from hereditary risk, but not as an overall reduction in risk from radiation exposure. To date, no hereditary effects from radiation have ever been observed or concluded in humans (Marsh & Silosky, 2019).
However, over recent years, a growing body of evidence has demonstrated that patient shielding provides negligible or no benefit. Some studies have begun to establish evidence that shielding actually carries a substantial risk of increasing the absorbed radiation dose and compromises the diagnostic efficacy of the acquired images. Part of these risks is related to advancements in diagnostic imaging technologies. Modern x-ray imaging systems have an automatic exposure control, in which a sensor detects when the target dose is obtained. In fluoroscopy procedures, automatic brightness control algorithms function as a feedback loop, so that the x-ray tube output is constantly adjusted to ensure quality images are consistently obtained. Therefore, with these new technologies, if a lead shield is applied and enters the field of view, the radiographic tube will automatically adjust and drastically increase the radiation output to try to penetrate the shield. This heightens the risk of increased absorbed radiation by the patient.
Furthermore, studies continually demonstrate that gonadal shielding is often positioned incorrectly, obscuring the image of the intended body part, and thus increasing repeat imaging rates (Marsh & Silosky, 2019). In 2012, Frantzen and colleagues demonstrated that gonadal shields were incorrectly positioned in 91% of pelvic x-ray examinations and several other studies have subsequently replicated these findings (Frantzen et al., 2012). The focus on the discontinuation of patient shielding practices has become increasingly prominent in radiology literature over the last few years. On April 2, 2019, the American Association of Physicists in Medicine (AAPM, 2019) released a position statement supporting the discontinuation of patient gonadal and fetal shielding in routine practice. On May 30, 2019, the ACR submitted a letter to the AAPM, endorsing their position on patient gonadal and fetal shielding. The ACR is in the process of adapting this new change into their guidelines, with the objective that this recommendation is universally adopted and becomes the standard of care across diagnostic radiology (ACR, 2019a).
The Burden of Overuse and Misuse of Medical Imaging
The rate of diagnostic imaging and associated radiation exposure has expanded tremendously over the last few decades. Currently, medical radiation comprises nearly 50% of the per capita radiation doses compared with 15% in 1980. Since 1980, medical radiation exposure has increased by 600% in the US (McCance & Huether, 2019). Findings from a population-based study spanning 15 years demonstrate that the number of adult CT scans tripled between 1996 and 2010 (Smith-Bindman et al., 2012). In 2011, more than 85 million CT scans were performed in the US, with CT scans accounting for approximately half of all medical radiation exposure, which is nearly a 28-fold rise from the 3 million CT scans performed in 1980. An analysis of data from 2013 to 2016 across the US compared to 10 other high-income countries demonstrated that the US occupies the top usage ranks of CT scans, with population rates of annual CT scans to be 245 per 1000 people (compared with a mean of 151 per 1000 people) (Papanicolas et al., 2018). This rise in radiation exposure is secondary to the increased amount of CT scans being performed, but also due to the increase in the radiation dose in each scan. Due to advancements in technology, modern CT scans are multiphasic, which means they are performed using repeated scanning before and after injection of a contrast dye agent. The multiphasic scanning process generates more precise and significantly higher resolution images, allowing for increased diagnostic accuracy. However, they also expose patients to 30-50% more radiation than older CT scanners (AHRQ, 2019).
Medical imaging does not always produce useful results. Within the US, there are too many imaging tests being performed that are either the incorrect type of test or not indicated based on the patient's clinical situation. Aside from the high-cost burden to society, unnecessary and inappropriate medical imaging notoriously leads to incidental findings, overdiagnosis, overtreatment, and patient anxiety, contributing to repeated imaging and more radiation exposure (Litowski et al., 2016). While radiation exposure is a widely recognized and well-described health risk of medical imaging, the National Cancer Institute (NCI, 2016) also describes the risk for false-positive and false-negative test results. False-positive results occur when an abnormality is identified on the scan (such as cancer), but no abnormality or cancer is actually present within the patient. False positives often lead to additional diagnostic work-up, which can include further radiology imaging tests carrying additional radiation exposure, or invasive tests, such as a biopsy. False-negative results mean that no abnormality was identified on the imaging test, despite the presence of some underlying pathologic process within the patient. False-negative results lead to delays in treatment and a false sense of security for the affected patient. Incidental findings refer to the identification of a previously undiagnosed medical condition that is discovered unintentionally during evaluation for another condition or ailment. Incidental findings pose several medical and ethical dilemmas for clinicians and patients and often lead to additional unnecessary diagnostic work-up and monitoring, contributing to further unnecessary radiation exposure, depending upon the condition identified. There are times where incidental findings can be life-saving, such as when a pancreatic tumor is identified during imaging performed for another reason. However, the vast majority of incidental findings contribute to the overuse of medical imaging services and inflate the cost burden to the patient, the healthcare system, and the economy. Similarly, overdiagnosis and overtreatment are well-described in medical imaging literature. One of the most prominent and controversial examples of overdiagnosis and overtreatment is ductal carcinoma in situ (DCIS) of the breast, which is commonly identified on screening mammography. DCIS is a non-invasive tumor of atypical cells that have not spread outside of the ducts or lobules into the surrounding breast tissue. DCIS has been the topic of tremendous debate over the last few decades regarding how to classify the condition and its definitive treatment pathway (NCI, 2016).
One of the most common misuses of medical imaging relates to the diagnosis and management of low back pain. Low back pain is the biggest cause of disability worldwide and one of the most common reasons for seeking medical care, as nearly 80% of the US population will experience low back pain at least once in their lifetime (Kim et al., 2019). To reduce the burden of unnecessary medical imaging, the American Board of Internal Medicine (ABIM) Foundation launched the Choosing Wisely campaign in 2012. The choosing wisely campaign has compiled evidence-based recommendations from various medical specialty societies about potentially unnecessary medical testing and procedures. It is intended to guide clinicians on the proper ordering of diagnostic imaging and promote conversations between clinicians and patients; it helps patients to choose care that is "supported by evidence, not duplicative of other tests or procedures already received, free from harm, and truly necessary" (ABIM Foundation, 2020). As part of the Choosing Wisely campaign, the American College of Physicians, American Pain Society, American Academy of Family Physicians, and the North American Spine Society all recommend against imaging studies in patients presenting with nonspecific low back pain (Litowski et al., 2016).
Expanding on the Choosing Wisely campaign, the Centers for Medicare & Medicaid Services (CMS) established the Protecting Access to Medicare Act (PAMA) of 2014, Section 218(b), to increase the rate of appropriate advanced diagnostic imaging services provided to Medicare beneficiaries. This led to the development of the Appropriate Use Criteria (AUC) for Advanced Diagnostic Imaging, which serves as a resource modality to increase the rate of appropriate advanced diagnostic imaging services while decreasing the risk for medically unnecessary imaging. The objective is to ensure that clinicians order the most patient-appropriate test based on the specific clinical condition (CMS, 2020). Initially, participation was voluntary, but as of January 1, 2020, PAMA released a statement removing the voluntary participation clause, informing providers ordering Medicare Part B advanced diagnostic imaging services on the need to consult the AUC before ordering the test. This applies to CT, MRI, nuclear Medicine, and PET scans, for all Medicare patients, to be rendered in outpatient and emergency department settings. CMS (2018) uses the data collected from the AUC program to identify any outlier ordering clinicians, who then become subject to a system of prior authorization. The AUC information is available to clinicians through an electronic, interactive tool called a Clinical Decision Support Mechanism (CDSM). The CDSM tool helps with clinical decision making and can be available through certified health record (EHR) technology, private-sector mechanisms, or those established by CMS (CMS, 2018). Currently, the program is still within its educational and operations testing period and is set to be fully implemented by January 1, 2021. By this date, all providers will be required to engage in AUC consultations utilizing a qualified CDSM, furnishing the consultation information with their claims to render payment for services. Claims that are missing this information will not be paid (CMS, 2020).
In summary, the recommendations when ordering medical imaging tests:
- Justification: each diagnostic radiology imaging test and procedure must be justified and only performed when necessary. The benefits and risks of the intended test must be considered, and alternatives which pose less risk should be contemplated.
- Optimization and ALARA: tests should be performed using the minimal effective radiation dose required to achieve quality images, thereby reducing the radiation exposure as much as possible.
- Avoid unnecessary repeat testing: repeat testing is often necessary to monitor disease status and evaluate for treatment response, such as with cancer; however, all unnecessary repeat testing should be avoided (CMS, 2020; International Atomic Energy Agency [IAEA], n.d.b.).
Diagnostic Imaging Tests with Radiation Exposure
Imaging studies can be divided into two main categories: planar and cross-sectional. Planar studies produce two-dimensional (2D) images and include basic diagnostic radiology testing such as x-rays and mammography. Cross-sectional imaging techniques address the three-dimensional (3D) aspects of human anatomy by capturing more detailed images, often referred to as "slices." This type of imaging technology can then create a composite analysis of 2D slices to provide a 3D visualization of the anatomy. Cross-sectional imaging includes CT scan, ultrasound, and MRI (Elsayes & Oldham, 2014).
X-Ray
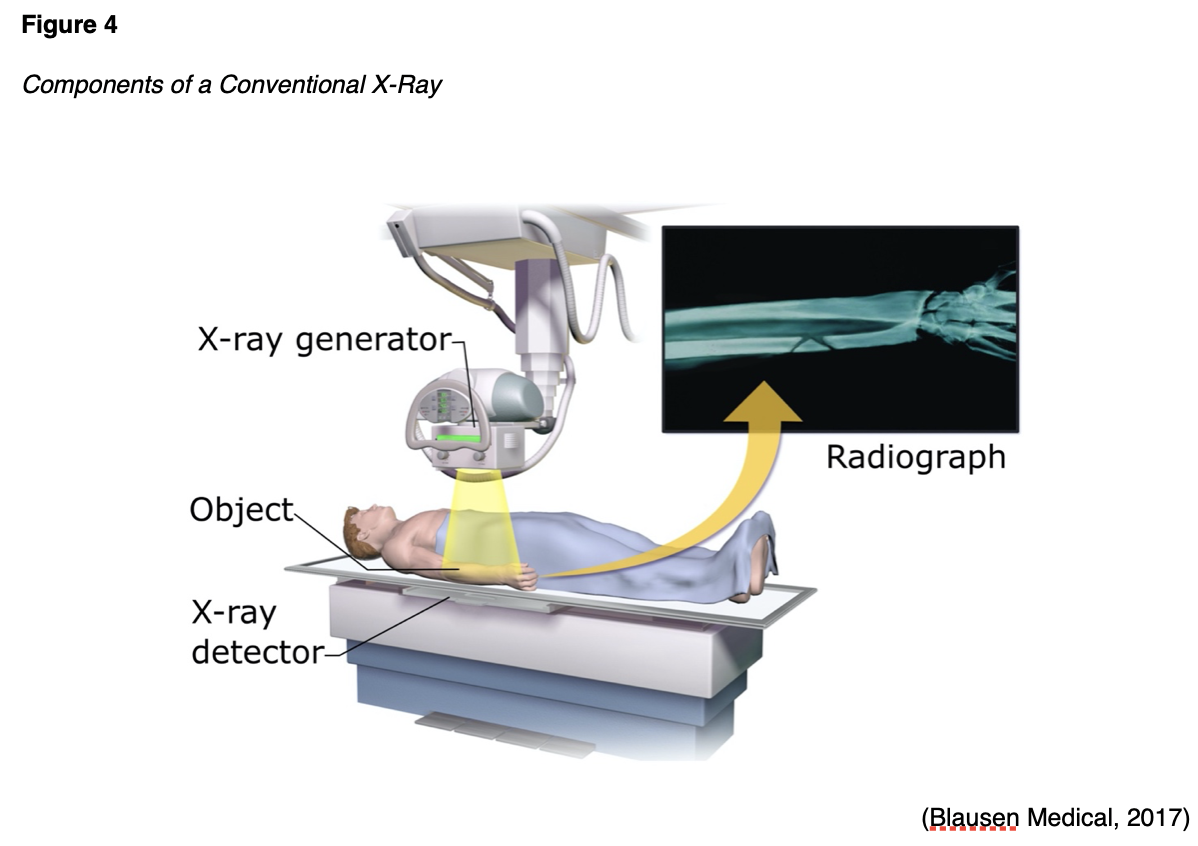
X-ray is the most common and readily available type of diagnostic imaging test. Often referred to as a plain film, an x-ray is a quick, noninvasive, and painless imaging modality that produces images of the structures inside the body. In a standard x-ray, a beam of energy is aimed at the intended body part, and a plate is placed behind the body part to capture the variations of the energy beam. As demonstrated in Figure 4, a conventional x-ray is the simplest example of how ionizing radiation produces a 2D image. For optimal imaging quality, the positioning of the x-ray detector should be as close to the body part as possible. The radiation beams should be perpendicular (situated at a right angle) to the body part, as this helps to minimize the magnification and enhance the sharpness of the resulting image, thereby producing a clearer result (Elsayes & Oldham, 2014).
X-rays are widely utilized throughout various healthcare domains with several indications. They are particularly useful for diagnosing acute bone fractures and cardiopulmonary conditions, such as cardiac enlargement, pneumonia, or pleural effusion (fluid inside the lung). X-rays are commonly used in dental care as a means of identifying cavities and underlying dental pathology. They are also useful for diagnosing arthritis and identifying foreign bodies or bowel obstructions. In addition, x-rays may be used to assist in fluoroscopy procedures, facilitating the placement of tubes or other devices inside the body. Similarly, x-rays are also used to verify the proper placement of a device following surgery or to ensure no medical devices were left in the body following major surgery (IAEA, n.d.b).
Patients are required to remove any clothing or jewelry, particularly metal, that may interfere with the procedure. This standard applies to all forms of diagnostic imaging tests and procedures. The patient should be educated that they will either lie, sit, or stand still while the x-ray machine takes images. The patient may be asked to move into several specific positions to obtain the highest quality imaging results. For instance, when evaluating a patient for pneumonia, the patient is usually asked to take a deep breath in and hold it, which helps to expand the lung fields and provide a higher quality image. In addition, several images may be taken from different viewpoints to facilitate a proper view. The entire process should take no more than 15 minutes at most. As described in Table 2, the ionizing radiation exposure from a conventional x-ray is very low to negligible, and adverse effects are rare; however, the risk versus benefit ratio must be carefully considered before ordering any x-ray (Elsayes & Oldham, 2014).
Fluoroscopy
Fluoroscopy is a medical imaging test used to study the motion of internal body structures. According to the CDC (2016), fluoroscopy uses an x-ray beam that passes continuously through the body to create an image, and the image is projected on a monitor, which allows clinicians to evaluate the movement of internal organs or devices in real-time. Medical imaging tests using fluoroscopy are generally non-invasive diagnostic tests performed to evaluate specific areas of the body. Fluoroscopy can help evaluate the bones, muscles, joints, as well as solid organs, such as the heart, lung, or kidneys. It can be used alone as a diagnostic procedure or in combination with other procedures. Fluoroscopy plays an important role in preventing health problems and diagnosing diseases. It is used in many types of diagnostic testing and procedures, and the amount of exposure to ionizing radiation during fluoroscopy depends on the test being performed and the equipment used. Some of the most common include, but are not limited to, the following:
- Barium x-rays (examination of the gastrointestinal [GI] tract);
- Intravenous pyelogram (visualization of the kidney, ureters, and bladder);
- Arthrography (visualization of a joint);
- Cardiac catheterization;
- Locating foreign bodies;
- Guiding medical procedures involving placement of catheters, stents, or other devices within the body;
- Image-guided anesthesia injections into joints or the spine (Johns Hopkins Medicine, n.d.b).
Barium X-Rays
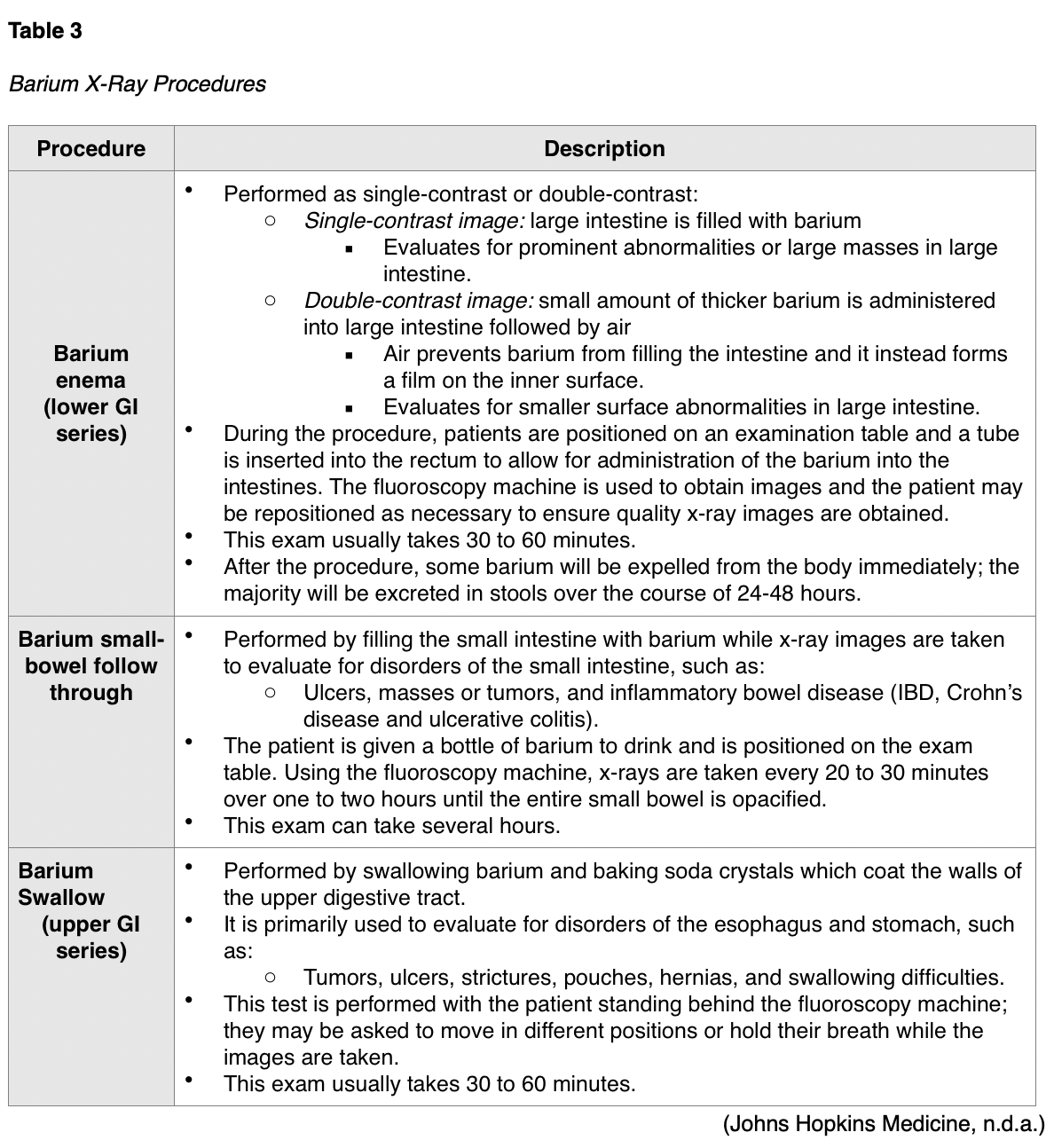
Barium x-rays are used to diagnose underlying pathology within the GI tract, which may include ulcers, inflammation, tumors, hernias, or strictures. Barium is a white, chalk-like powder that is mixed with water to create a liquid that is either ingested by the patient or administered via enema. The barium coats the lining of the GI tract, providing visualization of the walls of the esophagus, stomach, and intestines. This allows radiologists to evaluate the contour, shape, size, and patency of these structures to identify any underlying pathology. After the barium is administered, fluoroscopy allows the radiologist to see the movement of the barium through the GI tract. There are three types of barium x-ray procedures, which include the barium enema, or lower GI series, the barium small-bowel follow-through, and the barium swallow or upper GI series. Barium x-ray tests are typically performed as an outpatient procedure, and the defining features and details of each test are described in Table 3. Prior to any of these procedures, patients usually require a bowel preparation to empty the large intestine and any feces that can obscure the x-ray images, and preparation instructions generally include some variation of the following:
- Adherence to a special liquid diet for up to two days prior to the test;
- A bowel cleanse (laxatives, suppositories);
- Remain NPO after midnight before the procedure (Johns Hopkins Medicine, n.d.a.).
Following all barium x-ray procedures, patients should be advised to increase the consumption of foods high in fiber as well as oral hydration to facilitate bowel movements. Bowel movements may be white or lighter in color for one to two days following the procedure. Further, patients should be counseled to contact their provider if they are unable to pass gas or if they do not have a bowel movement for more than two days following the procedure, as they may require a laxative or enema to assist with eliminating the barium (Johns Hopkins Medicine, n.d.a.).
Intravenous Pyelogram
Intravenous pyelogram (IVP) is a fluoroscopic procedure that uses iodinated contrast material to assess for abnormalities within the kidneys, ureters, and bladder. The contrast is injected into the patent intravenously, and it travels to and collects within the kidneys and urinary tract. The contrast makes these areas appear bright white on the resulting x-ray images, thereby allowing the radiologist to identify any underlying pathology. This test is commonly performed to evaluate the etiology of hematuria or flank pain generating from the kidneys. An IVP is most commonly ordered to evaluate for the following suspected conditions:
- Kidney stones;
- Enlarged prostate;
- Tumors in the kidney, ureter, or bladder;
- Congenital abnormalities of the urinary tract;
- Complications from surgery on the urinary tract (RadiologyInfo.org, 2019a).
Typically performed as an outpatient procedure, patients will need to empty their bladder immediately before the scan to allow for the best quality images. Following contrast administration, the patient will lie flat on an exam table, and a series of x-ray images are taken while the kidneys are processing the contrast. Patients may be asked to lie on their side for enhanced images depending on the underlying issue. The exam usually takes up to one hour in duration, but in patients with impaired or sluggish renal function, the exam may take up to four hours. Following the procedure, patients are advised to increase oral hydration to flush the contrast out of the renal system (RadiologyInfo.org, 2019a).
Mammography
Mammography is a type of breast imaging test that uses low-dose x-rays to view the breast tissue as a means to identify abnormalities that are suspicious for breast cancer. A mammogram is one of the most widely used cancer screening tools that has been successful in identifying early breast cancer in asymptomatic women and preventing breast cancer deaths. Approximately 33 million screening mammography exams are performed each year. Since the introduction of screening mammography in the late 1980s, the breast cancer death rate in the US has decreased by nearly 40% (Arleo et al., 2017). According to the NCI (2019), 12.8% of women born in the US will develop breast cancer at some point in their lives, which means that each female in the US has a 1 in 8 risk level of being diagnosed with breast cancer throughout her lifetime; and this risk increases with age (NCI, 2019). Randomized clinical trials have demonstrated that routine screening mammography can reduce the number of deaths from breast cancer in women aged 40 to 74 years (NCI, 2016).
In modern practice, mammography is performed for one of the following two indications: as a screening modality or as a diagnostic test. As described above, screening mammography is central to detecting precancerous and cancerous breast lesions in women who have no symptoms. Current guidelines put forth by the ACR and the National Comprehensive Cancer Network (NCCN) recommend annual mammography screening for all women at average risk beginning at age 40 and for women at higher risk to begin prior to age 40 (for additional information regarding the specifics on breast cancer screening for early detection, please refer to the NursingCE.com course entitled Cancer Prevention and Early Detection). Diagnostic mammography is ordered in a patient who presents with abnormalities, such as a palpable breast lump, nipple discharge, or skin changes. Diagnostic mammography may also be advised following an abnormal screening mammogram as a means of obtaining enhanced and dedicated images of the area of concern. In many patients, a diagnostic mammogram is performed in combination with an ultrasound of the breast tissue (RadiologyInfo.org, 2019b).
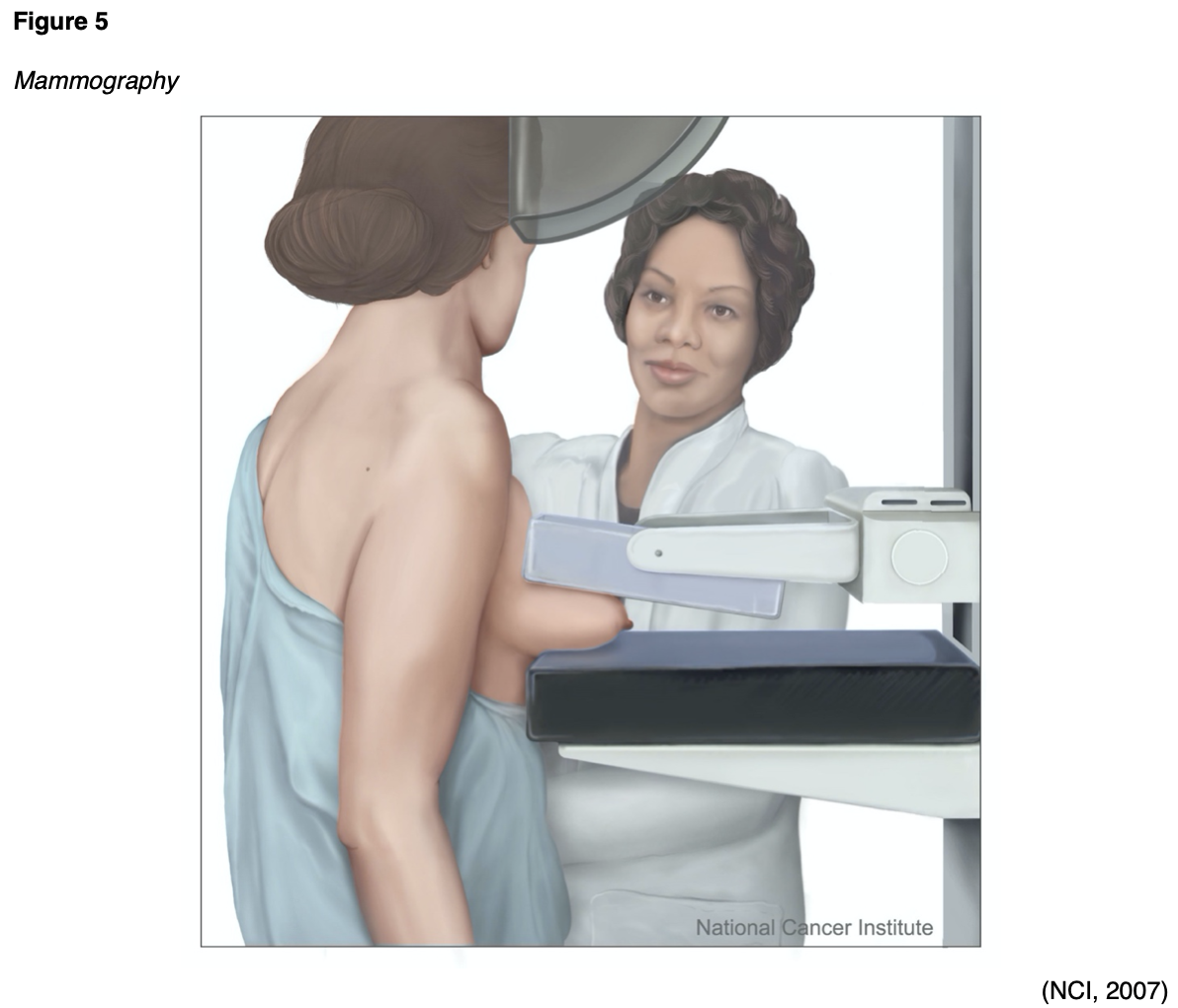
As demonstrated in Figure 5, a mammogram is performed by compressing the breast tissue within a machine that looks like a rectangular metal box, which spreads out the breast tissue and eliminates motion. The patient is instructed to stand facing the mammography machine during the exam, one breast is placed on the flat surface at a time, and a lever called a compression paddle is lowered to squeeze the breast tissue. Compression of the breast tissue is essential to ensure that all of the breast tissue can be visualized, and to allow the x-ray beam to penetrate through the breast tissue. Further, compressing the breast tissue also allows for the use of lower doses of radiation when a thinner amount of breast tissue is imaged. Once the images are acquired, they are subsequently processed on a special computerized system. The patient will be advised to remain very still during the test and, at times, may be asked to hold their breath to reduce motion and artifact when the x-ray is acquiring the images. Most women describe the exam as uncomfortable due to the pressure on the breast tissue from the compression paddle, but it is generally not considered a painful test. A mammogram usually takes about 30 minutes, and patients can resume normal activities immediately following the test (Mayo Clinic, 2019a; RadiologyInfo.org, 2019b).
Standard mammography imaging has evolved significantly over the last few decades, with the development of computer-aided detection (CAD), digital mammography, and breast tomosynthesis (RadiologyInfo.org, 2019b). CAD is a form of artificial intelligence that was devised as a means to help identify possible abnormalities on the mammogram that may otherwise have been missed by highlighting them for the radiologist. While CAD is increasingly used, the efficacy of the system remains controversial due to mixed results from research studies. Its clinical benefits and efficacy continue to be studied; however, its use does not replace the need for a qualified radiologist to interpret mammogram images directly (Katzen & Dodelzon, 2018).
Some women may opt to undergo digital mammography. This modality is similar to a digital camera and produces higher quality images using lower amounts of radiation. Breast tomosynthesis is also referred to as 3-D mammography and is an advanced imaging modality that can capture several images of the breast from different angles. The images are then compiled into 3-D images. The radiation dose for breast tomosynthesis is slightly higher than conventional mammography. However, large population-based studies have demonstrated improved breast cancer screening detection rates and reduced need for additional views for women with dense breasts. Although breast tomosynthesis is a newer imaging modality, some of its clinical benefits include the following:
- Earlier detection of small breast cancer that may not have been seen on a conventional mammogram due to clearer images;
- Particularly helpful in patients with dense breasts;
- Increased likelihood of detecting multiple breast tumors during one imaging test and pinpointing the size, shape, and specific location of the abnormalities;
- Reduced number of unnecessary biopsies or additional imaging tests (RadiologyInfo.org, 2019b).
CT Scans
CT scans, sometimes referred to as computed axial tomography (CAT) scans, use a series of x-rays and computer technology to create cross-sections of the inside of the body, including bones, blood vessels, organs, and soft tissues (Elsayes & Oldham, 2014). The x-ray detector moves in a circle around the body to generate several different views of the same body structure being evaluated. It sends x-rays through the body during each scan rotation to form a complete picture in much greater detail than a conventional x-ray. CT scans use ionizing radiation as their imaging method and may be performed with or without intravenous contrast administration. Some types of scans use iodine-based contrast, which may be given intravenously (IV), orally (PO), or both. When contrast is used, patients are typically required to fast or remain nothing by mouth (NPO) for several hours prior to the scan to provide a better picture of the body area in question. Oral contrast is administered about two hours prior to the examination and is most useful with visualizing the structures of the abdomen and pelvis. For those receiving IV contrast, patients will need to have a needle inserted into the arm for the injection. Patients should be informed that almost immediately following contrast injection, they may feel warm or flushed, and may experience a metallic taste in the mouth. These symptoms are generally transient, and only last seconds to minutes before they resolve (RadiologyInfo.org, 2018a). Additional details regarding the multifaceted aspects of iodinated contrast administration are described in Part 1 of this module.
CT scans are used to diagnose injuries from trauma such as bone fractures, infections, internal bleeding, tumors, masses, and cancers, and are also used to guide biopsies. The CT scan is considered a first-line screening modality for patients presenting with acute head trauma or stroke, as it can quickly and easily evaluate for hemorrhage or an ischemic event. In these cases, the CT scan of the head is usually ordered without contrast, as it is obtained emergently. When malignancy or infection is suspected, the use of IV contrast is recommended to better visualize the internal structures of the head (Elsayes & Oldham, 2014).
CT scans are also commonly used in the care of oncologic patients, as part of the cancer staging work-up, to evaluate response to cancer treatments, and monitor for cancer progression or recurrence. CT scans may also be ordered of the face, sinuses, orbits, or neck, and are generally performed to evaluate for suspected infection (sinusitis, orbital infection) or mass (malignant or benign tumors) within these locations. A CT scan of the chest is commonly performed to evaluate the lung parenchyma as well as the mediastinum for the presence of pulmonary nodules, masses, pleural effusions, or other signs of lung disease. CT imaging of the abdomen and pelvis has a wide range of ordering indications. In general, contrast is advised when evaluating for suspected appendicitis, diverticulitis, abscess, or other infection, as well as small bowel obstruction. CT angiography (CTA) is a type of CT scan performed to evaluate the blood vessels in a particular area for narrowing, obstruction, or thrombosis. Most commonly, a CTA scan is ordered to evaluate for suspected pulmonary embolism (pulmonary CTA), aortic dissection (thoracic aorta CTA), and brain aneurysm (intracranial CTA). There are numerous additional indications for CT scans and specific imaging protocols in place based on the suspected injury or illness to ensure the highest quality of images are obtained, which are beyond the scope of this module (IAEA, n.d.a.).
Patients should be advised that they will be required to lie flat and remain still on a table that slides into the scanning machine, which resembles a large doughnut, as displayed in Figure 6. The machine will rotate around the patient to take all the necessary images. The test takes about 10 to 15 minutes to complete (IAEA, n.d.a). As explained earlier, patients who undergo CT scans with high doses of radiation, as well as patients who undergo several repeated CT scans, are at heightened risk for cancer later on in life as a result of these scans. CT scans and CT-based diagnostic procedures are associated with significantly higher doses of radiation than conventional x-ray (AHRQ, 2019).

Nuclear Medicine Imaging
Nuclear medicine imaging is different than conventional diagnostic imaging as it is capable of visualizing how the body is functioning at the cellular and molecular levels. Nuclear imaging uses small quantities of radioactive tracers (radiotracers) to diagnose and treat disease. The radiotracers are most commonly injected into a vein, but may also be taken orally or inhaled. The radiotracer travels through the body, releasing energy in the form of gamma rays. It gets absorbed by specific tissues and organs. It is then detected by the external scanning device to provide information on organ function and cellular activity (Society of Nuclear Medicine & Molecular Imaging [SNMMI], n.d.).
The radiotracers are comprised of molecules that are bonded tightly to a radioactive atom, and these molecules vary greatly depending on the purpose of the scan (National Institute of Biomedical Imaging and Bioengineering [NIBIB], 2019). Radiotracers must meet US Food & Drug Administration (FDA) standards for safety due to radiation exposure. The use of radioactive materials for nuclear medicine is regulated by the Nuclear Regulatory Commission (NRC), the FDA, and individual states to ensure the safety of patients, healthcare professionals, and the general public. Each nuclear medicine imaging test uses a specific radioactive agent. There are various types of nuclear medicine imaging tests available, many of which are integral to the care of patients with cancer, heart disease, and bone disorders. Some of the most common include:
- Positron emission tomography/Computed tomography (PET/CT);
- Single photo emission computed tomography (SPECT);
- Thyroid scintigraphy and radioactive iodine uptake (RAIU) test;
- Skeletal scintigraphy (Bone Scan);
- Bone densitometry scan (DXA);
- Multigated acquisition scan (MUGA) (SNMMI, n.d).
Positron Emission Tomography/Computed Tomography (PET/CT)
PET/CT imaging uses the radiotracer fluorodeoxyglucose (FDG) to create 3D images and is combined with CT scans to better locate areas of abnormal cell activity. There are a few types of PET/CT scans, but the most common is a full-body PET/CT, which evaluates the internal structures from the mid-portion of the skull down to the thigh area ("eyes to thighs"), in combination with a low dose CT scan. This is a hybrid imaging modality; the resulting images acquired from each test are fused using advanced computerized technology to create enhanced images of higher quality. The functional imaging obtained by the PET scan illustrates the spatial distribution of metabolic or biochemical activity in the body, which is then more precisely aligned with the anatomic imaging obtained by the CT scan. PET/CT scans provide superior information for evaluating tissues, the staging and restaging of cancers, and are useful for monitoring the effectiveness of cancer treatments. Since cancer cells take in glucose faster than normal tissue, the FDG tracer is a superior radiotracer for evaluating cancerous tissue, as FDG is a compound similar in chemical composition to glucose. The FDG accumulates in areas of the body that are most metabolically active, which helps differentiate between physiologic uptake (healthy tissue) and pathologic uptake (diseased tissue; Thayalan, 2014).
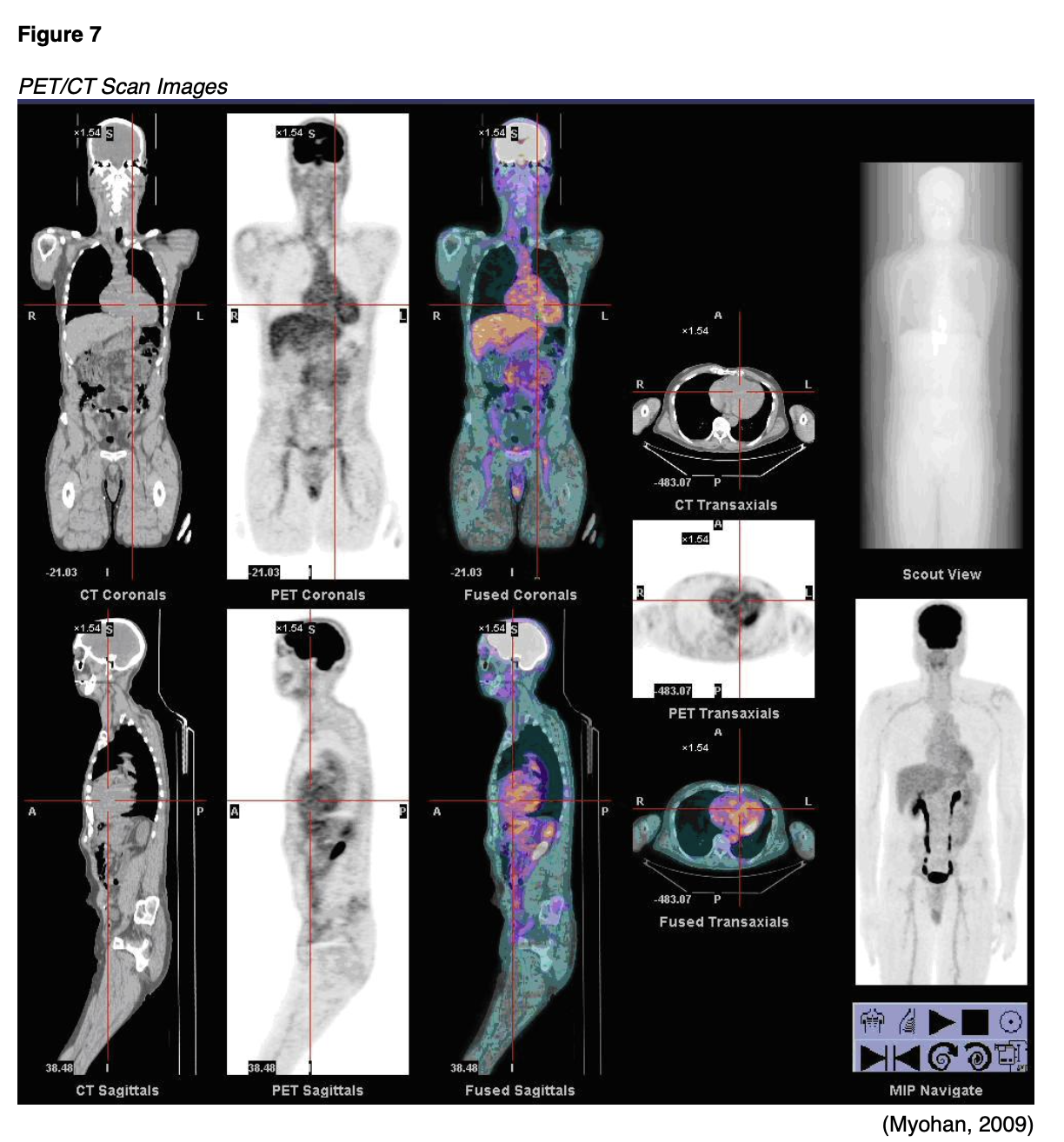
The FDG radiotracer is injected into the patient's bloodstream, and the PET/CT scan creates images that show the distribution of the radiotracer throughout the body and determine if abnormalities are present. Highly active cancer cells show higher levels of uptake of FDG, whereas brain cells affected by dementia consume smaller amounts of glucose, indicated by lower FDG uptake (Memorial Sloan Kettering Cancer Center [MSKCC], 2019). An example of the resultant images obtained from a PET/CT scan are displayed in Figure 7.
For 24 hours prior to the PET/CT scan, patients are advised to avoid strenuous activities such as running or cycling, as these activities can impair the quality of the images obtained. Since the PET/CT scan measures the uptake of glucose, strenuous activity can lead to increased uptake of the radiotracer in strained and recovering muscles, which increases the likelihood of false-positive results. Patients are advised to fast for six to eight hours before the scan and follow a low glucose, low carbohydrate diet for 24 hours prior to the scan. On the day of the scan, the patient's fasting blood glucose (FBG) will be obtained, usually through a finger stick. The FBG level should be between 70 and 199 mg/dL for the highest quality imaging results. If the FBG is too high, the scan will be of poor quality, thereby interfering with the clinical benefit and accuracy of the results. Typically, patients with FBG levels of 200 mg/dL or above will be referred back to the ordering provider for glucose management, and their scan will be rescheduled. Patients who have underlying diabetes will be given individual instructions based on their diabetes management plan. However, all are advised to avoid taking any anti-hyperglycemic medications, such as metformin (Glucophage) or insulin, within four hours of the scheduled scan. If insulin or diabetic medications are taken too close to the FDG injection time, too much FDG will collect in the muscles instead of throughout the tissues where it should flow. As demonstrated in Figure 8, the PET/CT scanner resembles a CT scanner, which looks like a large doughnut. The patient will lay down on the table, usually in the supine position, and should be advised to lay very still. The exam table will move slowly through the scanning ring, and the test usually takes 25 to 40 minutes (Thayalan, 2014).

Following the scan, patients should be advised that some security equipment can detect radioactivity, setting off radiation alarms, such as radioactive detectors in police cars and airport security. Therefore, most patients are given a card stating that they had a test performed with a radioactive tracer. Patients should also be advised to limit close contact with infants and pregnant women for at least 12 hours following the scan (MSKCC, 2019). As noted earlier, the ACOG (2017) recommendations for breastfeeding following nuclear imaging scans does not definitively state a position for or against the practice, and patients are advised to consult with a lactation specialist. In general, women who are breastfeeding may opt to stop breastfeeding for 12 hours following the scan, during which time they can continue to pump and discard the milk. Additional aspects of breastfeeding safety are described in part 1 of this module (MSKCC, 2019).
Single Photo Emission Computed Tomography (SPECT)
SPECT is another type of nuclear medicine imaging test that is very similar to PET/CT scans as it integrates CT technology and a radiotracer administered via injection. The primary distinction between PET/CT and SPECT imaging is the type of radiotracer that is used. In SPECT imaging, the radiotracer stays within the bloodstream rather than being absorbed by tissues and organs. SPECT imaging is largely focused on areas where blood flows; it is used to evaluate blood flow to surrounding tissues and organs, and how the organs are functioning. SPECT studies are most commonly used to diagnose or evaluate heart and brain disorders, but may also be used to assess certain types of bone disorders. With regards to the heart, SPECT imaging can be used to detect blockages within the coronary arteries, detect damage to the myocardium (heart muscle) resulting from a heart attack, and determine if the heart is pumping blood adequately, particularly when it is stressed. With brain functioning, SPECT studies may be ordered to evaluate for dementia, as well as the location and etiology of a stroke by visualizing how blood flows through veins and arteries in the brain. It can be used to diagnose areas of ischemia (blood deprivation) within the brain following a stroke or as a result of a tumor. These studies are also used in epilepsy, for detecting and identifying seizure activity. A clinician may also order a SPECT scan to evaluate areas of bone healing and assess for hidden bone fractures, such as spondylolysis (a stress fracture in the spine) (Mayo Clinic, 2019c).
During a SPECT scan, the patient is usually placed in the supine position on the examination table and asked to lie very still for the duration of the examination. Figure 9 depicts a patient undergoing a total body SPECT scan to evaluate their bones. After the radiotracer is injected, a special device called a gamma camera rotates around the patient. The device accumulates pictures which are then used to construct 3D images of the distribution of the radiotracer. The resulting images disclose information regarding blood flow and target organ function (SNMMI n.d.). Unlike PET/CT scans, which primarily use FDG as the radiotracer, SPECT studies can use various types of radioisotopes depending upon the disease suspected and the area of study. Patients are advised to fast for four to six hours prior to the scan, which can take up to two and a half hours to complete. Following the scan, patients are advised to maintain increased oral hydration for about two days to flush the radioactive material from the body. Otherwise, there are generally no special discharge instructions (American Heart Association [AHA], 2015c).

Thyroid Scintigraphy and Radioactive Iodine Uptake (RAIU) Test
There are two types of nuclear medicine imaging tests of the thyroid; thyroid scintigraphy, also called the thyroid scan, and radioactive iodine uptake (RAIU) test. Both scans use a small amount of radioactive iodine, usually in the form of I-123, as the thyroid gland is the only tissue within the body that absorbs and holds onto iodine. The radiation emitted by I-123 is harmless to thyroid cells, and it can be detected externally through the use of thyroid scanning. There are rare instances where I-131 may be used with RAIU scans, but I-131 destroys thyroid cells and is commonly reserved for the treatment of thyroid disorders such as overactive thyroid, thyrotoxicosis, and thyroid cancers, which are beyond the scope of this module (ACR, 2019b).
The thyroid scan is ordered to acquire information about the thyroid function and evaluate for abnormalities within the gland, such as nodules, masses, or inflammation. According to the ACR (2019b), thyroid scans are useful in, but not limited to, evaluation of the following:
- “Size and location of thyroid tissue;
- The cause of overt and subclinical thyrotoxicosis;
- Suspected focal masses or diffuse thyroid disease;
- Clinical laboratory tests suggestive of abnormal thyroid function;
- Function of thyroid nodules detected on clinical examination or other imaging examinations;
- Congenital thyroid abnormalities, including ectopia;
- Differentiating hyperthyroidism from other forms of thyrotoxicosis” (ACR, 2019b, p.2).
When undergoing a thyroid scan, the I-123 is either injected into a vein within thirty to sixty minutes of the scan or administered orally in the form of a pill or liquid. With oral administration, the I-123 must be given approximately four to six hours before the scan, as this allows the radioactive iodine the opportunity to reach and saturate the thyroid gland. The thyroid scan is painless, and patients are usually positioned lying flat (supine) on an examination table with their head tilted back to extend their neck. A scanner will take images of the thyroid from at least three different angles, and the patient will be asked to lie very still. It takes about 30 minutes to complete a thyroid scan (RadiologyInfo.org, 2019c).
The RAIU scan is performed to evaluate the function of the gland or determine the etiology of an overactive thyroid gland (hyperthyroidism). It may also be used to plan treatment for patients who have thyroid cancer. The RAIU uses a specialized probe to measure how much tracer the thyroid gland absorbs from the blood. In most cases, the RAIU scan is performed alongside with the thyroid scan to show if the radiotracer is evenly spread in the gland. According to the ACR (2019b), while the RAIU scan does have overlapping indications with the thyroid scan, it is considered most useful in the following situations:
- “Differentiating hyperthyroidism from other forms of thyrotoxicosis (such as subacute or chronic thyroiditis and thyrotoxicosis factitial [exogenous thyrotoxicosis]);
- Assessing the necessity and calculating iodine-131 sodium iodide administered activity for patients to be treated for hyperthyroidism” (ACR, 2019b, p.2).
Agents that contain iodine can decrease iodine uptake in the thyroid gland and lead to inaccurate test results. Iodine is hidden in many types of commonly used supplements, over-the-counter agents, and certain prescription medications. Therefore, before the test, a comprehensive medication reconciliation should be performed, and patients must be informed to discontinue thyroid hormones, anti-thyroid medications, and any other medication or dietary supplement that contains iodine. Each medication or supplement has a specified period in which it should be discontinued before the scan. For example, levothyroxine (Synthroid) is a thyroid hormone that must be discontinued for four to six weeks before the scan. In contrast, iodine-containing cough syrups should be discontinued two weeks prior to the scan. Other iodine-based agents that need to be discontinued include but are not limited to the following:
- Iodized salt;
- Multivitamins;
- Amiodarone (Nexterone);
- Kelp (algae seaweeds);
- Intravenous iodinated contrast agents;
- Sulfonamides;
- Methimazole (Tapazole) (ACR, 2019b).
In the one to two weeks leading up to the radioactive iodine administration, patients are generally advised to consume a low-iodine diet, avoiding the highest sources of dietary iodine which include salt, grains, cereals, fish, poultry, and milk products (American Thyroid Association [ATA], 2020). The RAIU scan requires administration of the radioactive iodine in liquid or capsule form, and the RAIU scan occurs at two distinct time points: usually at four to six hours following radiotracer administration, and then again at 24 hours. During an RAIU test, the patient is usually seated in an upright position, and a small device called a radioactive detector (uptake probe) is placed against the patient's neck. The uptake probe takes measurements of radioactive iodine uptake, and a gamma camera is used to record pictures of the thyroid gland. Both instruments work to detect and record the distribution of the radioactive material within the thyroid. The RAIU test usually takes several minutes. For patients who undergo both the thyroid scan and the RAIU scan, the oral route is generally preferred, as it can be used for both tests and does not require a second dose of the radiotracer (RadiologyInfo.org, 2019c). Following the test, patients should be advised that the majority of radioactive material is cleared from the body within one to two days. No special precautions need to be taken as I-123 is harmless to thyroid cells. The ACR (2019b) states it is safe to use radioactive iodine in patients who report iodinated contrast allergies or seafood allergies, as the reaction is to the compound containing iodine and not the iodine itself (ACR, 2019b).
Skeletal Scintigraphy (Bone Scan)
Skeletal scintigraphy is also called a bone scan, and it is a type of nuclear medicine imaging test that uses a small amount of radioactive tracer to diagnose and evaluate various bone disorders and conditions (RadioloyInfo.org, 2020b). A bone scan is performed to evaluate for several types of conditions, such as:
- Bone fractures, including stress, occult, accidental, and non-accidental;
- Primary bone masses or tumors (benign or malignant);
- Metastatic bone neoplasms;
- Underlying bone pain that is otherwise unexplained or non-responsive to conservative treatments, such as the case with chronic low back pain;
- Tumor-like conditions such as Paget’s disease;
- Infection such as osteonecrosis;
- Complications from orthopedic hardware or prosthetic joints;
- Congenital or developmental anomalies (ACR, 2017).
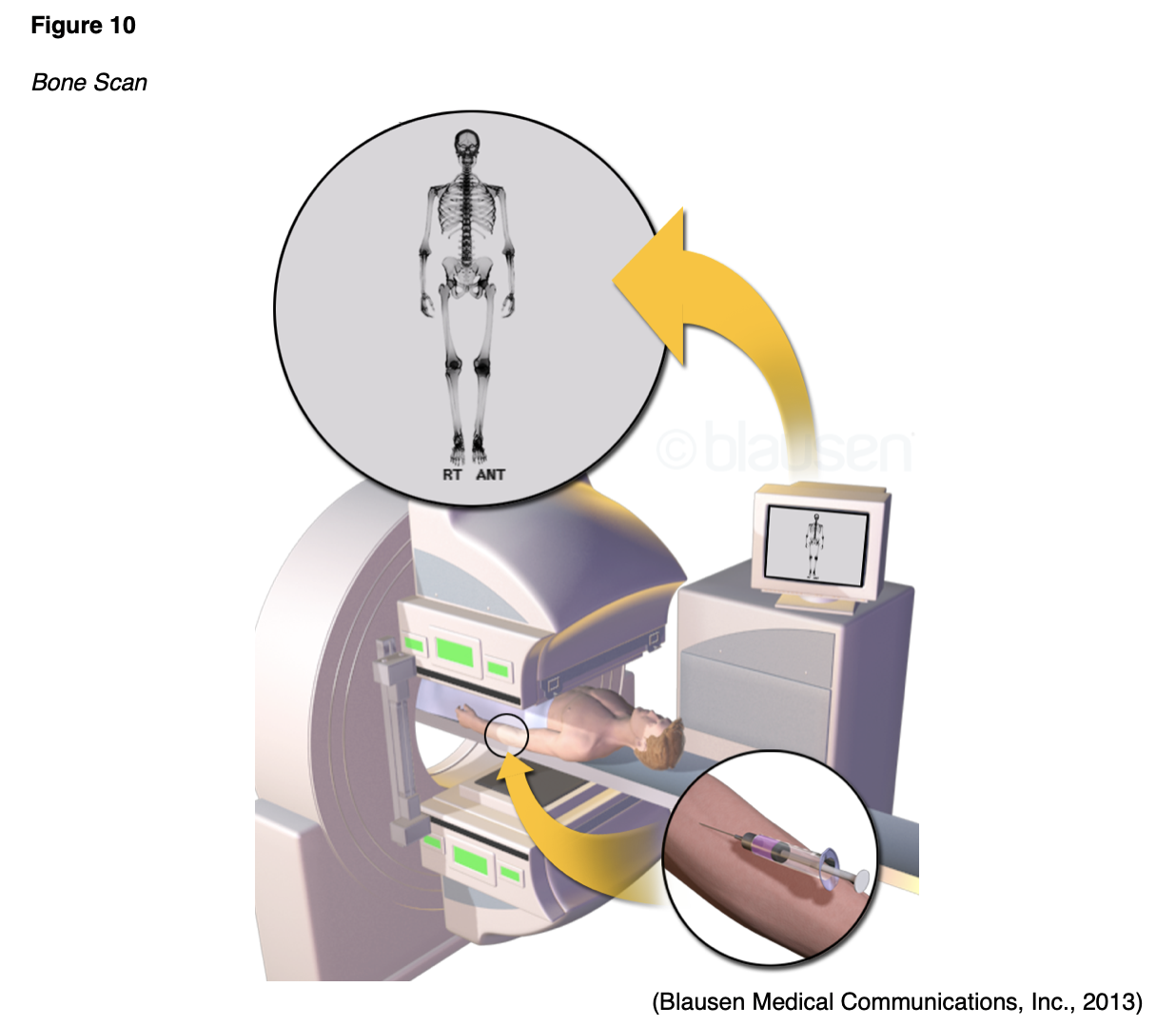
A bone scan is also routinely used to assess for the presence of cancer cells within the bones, to determine if cancer has spread to the bones, as well as for monitoring response to cancer treatment over time. As demonstrated in Figure 10, a radiotracer is injected into the vein and travels through the bloodstream, emitting radiation in the form of gamma rays. These are detected by a specialized gamma camera and fused with computer images to derive an overall picture of the bones (RadiologyInfo.org, 2020b).
A bone scan is capable of detecting changes at the molecular level, thereby allowing the early detection of bone disorders, even at the earliest stages of the disease. Abnormal areas within the bone will take up more or less of the radiotracer, thereby producing brighter or darker areas on the resulting images (RadiologyInfo.org, 2020b). Figure 11 is an example of skeletal scintigraphy of the pelvis highlighting areas of bone metastases from cancer.

In preparation for a bone scan, patients should be counseled to avoid bismuth-containing medications such as Bismuth subsalicylate (Pepto-Bismol, Kaopectate) for at least four days before the scan, as these medications can interfere with the results. In addition, patients should be screened for recent x-ray tests utilizing barium contrast material, which can also skew the results. Barium should similarly be avoided for at least four days before the bone scan. The radiotracers used with bone scans take a few hours to circulate through the body and bind to the bones to produce the highest quality images (RadiologyInfo.org, 2020b).
Patients should be advised that there will be a two to four-hour period between the injection administration and the time in which the scan will take place. During this time, patients will need to consume several glasses of water (usually four to eight) to facilitate the removal of any excess radiotracer from the body. Patients will also be instructed to empty their bladder prior to the scan, as any residual tracer in the bladder can obscure the view of the underlying pelvic bones (RadiologyInfo.org, 2020b). Patients will be asked to lie very still on the examination table during the test. A total body bone scan usually takes about one hour to complete. Following the scan, patients may resume normal activities and are advised to increase oral hydration for one to two days to help facilitate the removal of any residual radiotracer circulating in their system. It generally takes 48 hours for all of the radioactive tracer material to be excreted from the body (Cancer.net, 2018).
Bone Densitometry Scan (DXA)
A bone densitometry scan is also referred to as a dual-energy x-ray absorptiometry (DXA) scan. While it is a nuclear medicine test that uses a small amount of ionizing radiation to generate images of bony structures, it is vastly different than a bone scan. A DXA scan evaluates the bone mineral density (BMD), or the health and strength of the bones, and assesses fracture risk. It is considered the gold standard test to screen for, diagnose, and monitor osteoporosis. Osteoporosis is a chronic, systemic disease characterized by low BMD, weakening of the bones, and deterioration of bone tissue and architecture. It is the most common bone disease in the US, responsible for nearly two million broken bones per year (Porter & Varacallo, 2019). Osteoporotic bones are brittle and porous, heightening the risk for fracture. It is referred to as a silent disease because the loss of bone mass is not painful, and there are generally no warning signs or symptoms preceding bone fracture. The vast majority of people do not know they have osteoporosis until they develop an acute fracture or broken bone, which is the hallmark of the disease. Fractures can occur in any bone within the body but most commonly occur in the hip bones, vertebrae, and wrist. Osteopenia is the precursor condition to osteoporosis and is characterized by a lower than normal BMD that is not severe enough to meet the criteria for osteoporosis. People who have osteopenia are at higher risk for developing osteoporosis, but when identified early through screening with a DXA scan, and appropriate action is taken, progression to osteoporosis can be successfully averted (National Institute of Arthritis and Musculoskeletal and Skin Diseases [NIAMS], 2019).
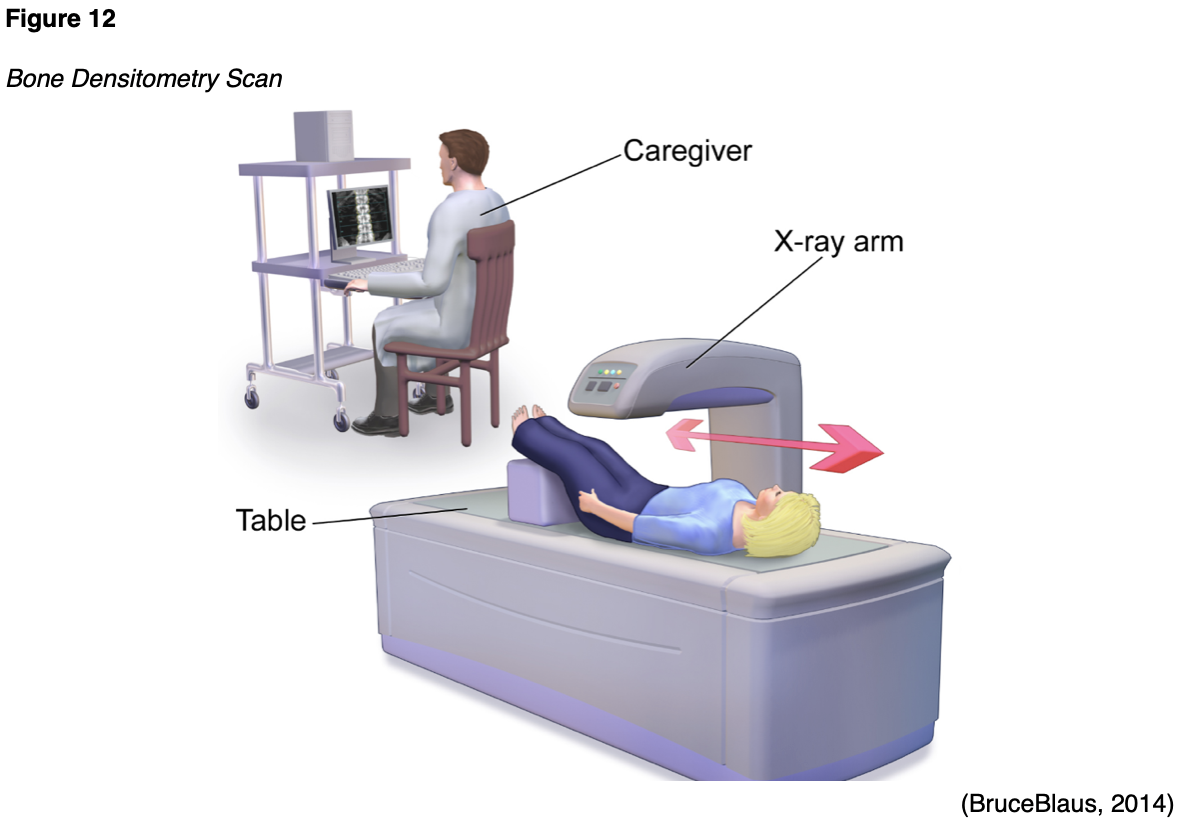
The BMD is most commonly measured at the spine, hip, and wrist levels, and the degree of bone loss is calculated and classified according to defined diagnostic criteria. The DXA scan is a quick, noninvasive, and painless test. As demonstrated in Figure 12, the patient is instructed to lie or sit down for less than ten minutes while the machine scans the body. The test exposes the patient to a small amount of radiation, but less than the amount associated with a chest x-ray (ACOG, 2018).
DXA test results are reported as a T-score for each site measured, which is a number comparing the patient's BMD level to that of a healthy young adult with ethnicity and gender-matched controls. The World Health Organization (WHO) separates those T-scores into four categories: normal, low bone mass (osteopenia), osteoporosis, and severe (established) osteoporosis. A T-score of 0 indicates that the BMD is equal to that of a healthy young adult, a negative T-score indicates that the bones are thinner than normal, and a positive T-score denotes that the bones are stronger than normal. The difference between a patient's BMD and the normal range is measured in units referred to as standard deviations. The more standard deviations below 0, denoted by negative numbers, the lower the BMD, the more severe the osteoporosis, and the higher the risk of fracture. The WHO classifies osteoporosis as a BMD that is 2.5 standard deviations below normal. Treatment is usually recommended when the T-score is -2.5 or lower to prevent fractures. Refer to Table 4 for a comparison of T-scores and the associated BMD level (NIAMS, 2018). Figure 13 is an example of a DXA test result report for a patient with osteopenia of the lumbar spine.

Multigated Acquisition Scan (MUGA)
A MUGA scan may also be called radionuclide ventriculography (RNV) or radionuclide angiography (RNA), and it is a type of nuclear imaging test that evaluates how well the heart is functioning; particularly the left ventricular ejection fraction (LVEF). The LVEF measures the amount of blood that is pumped out of the heart with each contraction and is expressed as a percentage. The normal LVEF in an adult is 50% to 75%. This test may be performed for various reasons, but is most commonly ordered as part of cardiology work-up for chest pain, in follow up to an abnormal electrocardiogram (EKG) or echocardiogram scan, or for monitoring patients with heart failure. MUGA scans are also used for monitoring patients undergoing chemotherapy that is toxic to the heart, chest wall radiation, or other cancer treatment regimens that can impair the heart function. MUGA scans are used to assess baseline cardiac function, as well as monitor for any changes to heart function at defined intervals during specific cancer treatments, such as the use of trastuzumab (Herceptin), a widely utilized breast cancer therapy (AHA, 2015b).
During the MUGA scan, small electrodes are placed on the patient's chest, arms, and legs, similar to an EKG, and these are used to track the patient's heartbeat and heart rhythm during the test. A radioactive tracer is injected into a vein, and a gamma camera takes images of the heart at designated time points during each heartbeat. A MUGA scan may be performed at rest, in which the patient lies on the table while the gamma camera takes photographs of the heart. Alternatively, it may be performed as an exercise or "stress" test, in which the patient walks on a treadmill or rides a stationary bicycle to obtain peak activity level, and is subsequently asked to stop and lie on the table while the gamma camera takes pictures of the heart. The test takes approximately one to two hours to complete, and patients can generally resume normal activities following the test. Patients are advised to drink plenty of water to help flush the radioactive materials through the renal system after the scan (AHA, 2015b).
Diagnostic Imaging Tests without Radiation Exposure
Magnetic Resonance Imaging (MRI)
MRI is a widely utilized diagnostic imaging modality, with an estimated 30 million scans performed in the US each year. MRIs are distinct from other forms of diagnostic imaging as they do not use x-rays or pose radiation exposure to patients, and are considered a very safe imaging test. MRIs utilize strong electromagnetic fields (EM) and radio waves to measure how much water is contained in different tissues within the body as a means to generate detailed images of internal organs and tissues (FDA, 2018). The signal in an MRI image comes mainly from the protons in fat and water molecules within the body. MRI is superior to CT scan at identifying the difference between normal and abnormal soft tissue. MRIs can be performed to image nearly any body part; each scan follows a specific protocol depending upon the clinical concern and may be performed without or without contrast administration. Gadolinium-based contrast agents (GBCAs) are rare earth metals that are administered intravenously to enhance the contrast of the MRI images. MRI contrast injections are distinct from CT scan contrast agents, and patients who have CT contrast allergies can typically safely tolerate GBCA injections (Ibrahim et al., 2020). Detailed information regarding special considerations with the use of GBCAs is contained within Part I of this two-part radiology series.
MRI scans are ordered for numerous indications and are considered one of the most frequently performed imaging tests of the brain and spinal cord. They can be used to diagnose aneurysms, multiple sclerosis, strokes, herniated discs, and tumors. While standard MRI scans are superior for evaluating soft tissues and organs, they also have clinical benefits with regards to imaging of the heart and blood vessels, including structural abnormalities in the aorta, the thickness of the heart walls, and damage caused by heart disease. MRI is used extensively in orthopedics to evaluate for bone and joint conditions, such as torn ligaments or cartilage. In women with dense or fibrotic breasts, MRI may be the preferred screening modality in place of mammography due to superior evaluation of dense breast tissue (MRI, 2019b).
Patients who are undergoing MRI scans of the abdomen or soft tissue pelvic structures are usually advised to remain NPO for six hours before the scan. Prior to an MRI of the prostate, or to evaluate for a vaginal/rectal fistula, a bowel preparation with an enema may be necessary. However, for all other MRIs, there are generally no special instructions that need to be followed the day prior to the scan. The MRI scanner is essentially a large magnet, and they can vary in strength, measured in a unit called tesla (T). Most modern MRI scanners are 1.5 to 3T. To put this into context, an MRI that is of 3T strength is about 60,000 times stronger than the earth's magnetic field. During an MRI, an electric current creates a temporary magnetic field within the patient's body, and radio waves are sent from and received by a transmitter and receiving device within the machine. These signals are used to generate images of the scanned area of the body (FDA, 2018). Patients are advised to lie very still on the table, as motion can create artifact and reduce the clarity of the images. The table slides into the MRI machine, which is somewhat similar in appearance to a CT scanner, as demonstrated in Figure 14. However, an MRI scanner is deeper and narrower than a CT scanner and poses a heightened risk for claustrophobia and anxiety in some patients, who may require a sedative before the scan to ensure relaxation and to manage anxiety. Patients should be advised that they will hear loud noises that sound like thumping and banging throughout the examination. Patients should be reassured that these are harmless sounds produced by the MRI magnets, and some patients will be given earplugs or headphones (Ibrahim et al., 2020). An MRI scan can take anywhere from 20 to 90 minutes, depending on the part of the body being imaged (FDA, 2018).
While there is no risk for radiation exposure with MRIs, there are serious risks for potential injury. Due to the powerful EM fields, the MRI machine can propel magnetic objects toward the center of the machine at dangerous speeds, including medically implanted hardware, such as cardiac pacemakers and infusion pumps. The radiofrequency field can also cause tissue heating and burning, particularly in the presence of implanted devices, which can also heat internally (Ghadimi & Sapra, 2019). All patients must undergo screening evaluations before testing to assess for the presence of metal or any type of implanted hardware. The FDA has received reports of serious adverse events associated with implantable pumps in the MRI setting, such as pump malfunction, including bolus dose, overdose, underdose, or pump failure, and some of these injuries have been fatal. According to the FDA (2017), only implantable infusion pumps labeled "MR Conditional" may be safely used within an MRI environment, and only under the specified conditions of safe use as outlined by the manufacturer of the individual device. During the screening, patients must also be asked if they have ever welded without eye protection or had any facial injury with metal. If the patient responds yes, then an orbit x-ray must be taken to ensure there is no hidden metal in the orbits prior to the MRI (Ghadimi & Sapra, 2019).
Given the strength of the EM fields, the below list is comprised of the most common absolute contraindications to MRI. However it should be noted that given advancements in technology and newer medical devices, some of these may be compatible. It is critical for clinicians to refer to the manufacturer’s instruction of the device when determining safety and compatiblity with MRI imaging.
- Cardiac implantable electronic devices (CIED) such as pacemakers, implantable cardioverter defibrillators (ICDs) and cardiac resynchronization therapy (CRT) devices;
- Metallic intraocular foreign bodies;
- Implantable neurostimulation systems;
- Cochlear implants;
- Catheters with metallic components (Swan-Ganz catheter);
- Metallic fragments such as bullets, shotgun pellets, and so forth;
- Cerebral artery aneurysm clips;
- Magnetic dental implants;
- Tissue expanders;
- Medication patches, hearing aids, body piercing, external drug delivery pumps (insulin pumps), and artificial limbs are all contraindicated and must be removed prior to the MRI (Ghadimi & Sapra, 2019).
Several relative contraindications must be taken into consideration before any MRI scan, as the specific patient situation must be evaluated with caution to confirm it is safe to proceed with the exam. Relative contraindications include patients presenting with any of the following:
- Coronary and peripheral artery stents;
- Non-plastic airway stents or tracheostomy (plastic tracheostomies are safe to proceed with the MRI, but if the composition of the tracheostomy is unknown or unsafe, it must be changed to a plastic source prior to the MRI);
- Intrauterine devices (IUDs) are controversial and currently are only acceptable with 1.5T MRI scanners;
- Ocular prosthesis;
- Stapes implants;
- Surgical clips or wire sutures;
- Certain types of prostheses (joint, penile, etc.);
- If the patient had a colonoscopy procedure within the previous eight weeks and endoscopy clips were used or placed during the procedure, the scan must be postponed (Ghadimi & Sapra, 2019).
Additional consideration must be given to the following situations prior to performing the MRI scan:
- Patients with programmable shunts must be informed that they have to reprogram their shunt with their provider following the MRI;
- Patients with inferior vena cava (IVC) filters that are of unknown composition, must wait six weeks following implantation and can only be scanned with a 1.5T MRI scan;
- Patients with Harrington rods (stainless steel surgical device) can only undergo an MRI on 1.5T scanners;
- Tattoos should be greater than six weeks old and ice packs or padding should be used against any tattoo that is in contact with the bore of the scanner or the MRI coil, and patients must be educated to immediately report any warm sensation that develops around the tattoo site (Ghadimi & Sapra, 2019).
Ultrasound
Ultrasound is a safe, noninvasive imaging modality that uses soundwaves to generate images of internal body structures. Also referred to as sonography, ultrasound does not use x-rays or ionizing radiation and can be used for diagnostic and therapeutic indications. Ultrasound images are obtained by placing a small probe (transducer) and ultrasound gel on the skin. The transducer produces soundwaves at very high frequencies, which exceed the threshold of human hearing. These high-frequency soundwaves travel from the probe through the gel and into the body, and then the soundwaves are used to generate images on a computer. Images are captured in real-time, which allows for the evaluation of the structures and movement of the body's internal organs, including blood flow through vessels. Transducers may be placed external to the body on the skin, such as with a fetal ultrasound, which is demonstrated in Figure 15. To optimize image quality, some transducers can also be placed directly inside the body via the vagina, GI tract, or blood vessels. As shown in Figure 16, a transducer is placed inside the vaginal canal of a nonpregnant female to enhance the visualization of the uterus and ovaries (NIBIB, 2016).
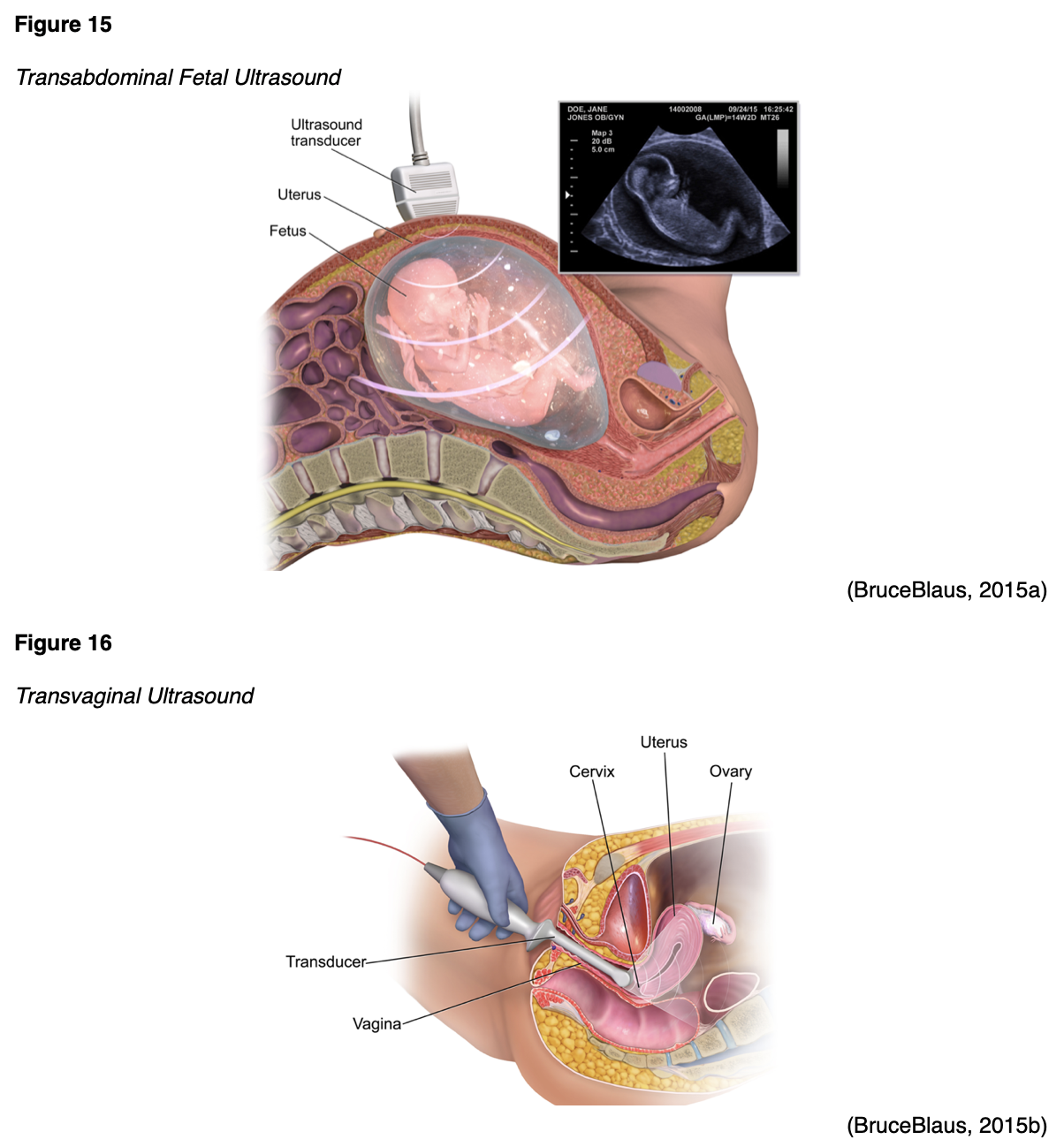
Conventional ultrasound displays images in flat sections of the body, but advancements in technology have led to the development of 3-D ultrasound that allows for the formatting of sound wave data into 3-D images. The most widespread use of a 3-D ultrasound is to assess a developing fetus, and the distinction between the resultant images generated from a conventional sonogram versus a 3-D sonogram is demonstrated in Figure 17 (NIBIB, 2016).
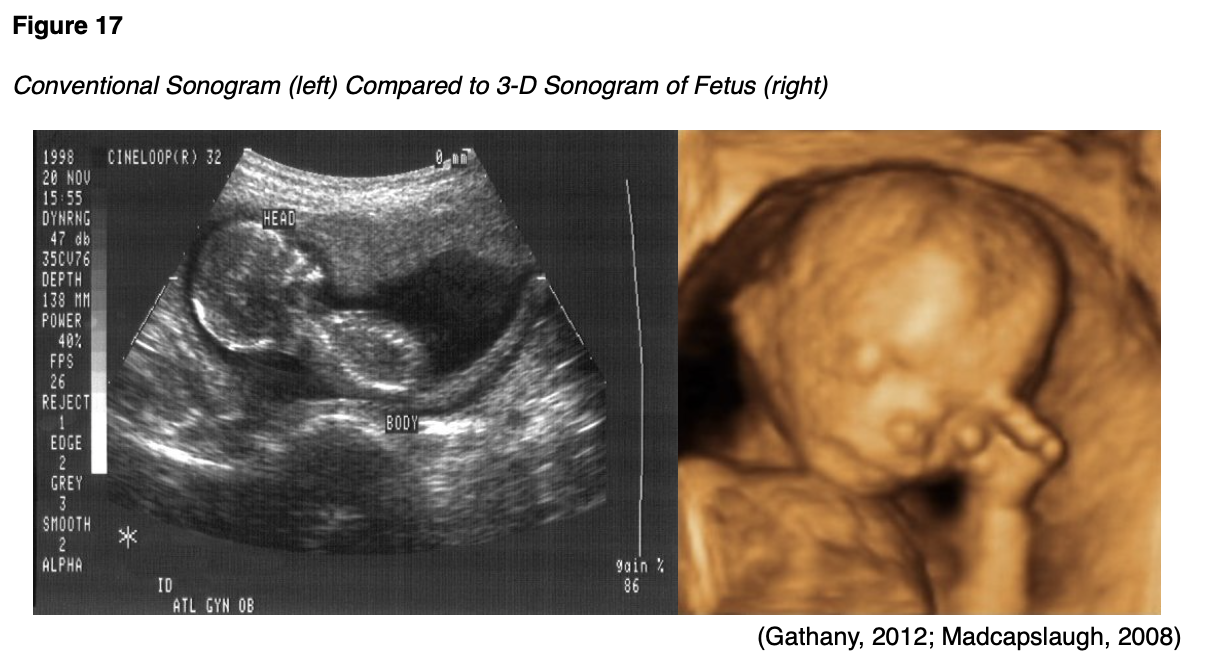
Ultrasound can be performed for diagnostic or therapeutic reasons. Therapeutic ultrasound interacts with tissues in the body to modify or destroy them. For example, therapeutic ultrasound may be used for ablative functions such as dissolving blood clots or delivering drugs to specific locations within the body. Diagnostic ultrasound is used to evaluate the internal organs and structures, movement, and velocity of tissue or blood, as well as any other abnormalities. Ultrasound may also be used during surgery to help guide the placement of a catheter or other medical device or to guide biopsies. An ultrasound-guided needle biopsy is a very common procedure when evaluating a breast mass for breast cancer (RadiologyInfo.org, 2018b).
Doppler ultrasound is a specialized technique that evaluates blood flow through the arteries and veins in the body. Doppler ultrasound is used to evaluate the following:
- Blockages to blood flow (such as thrombosis, deep vein thrombosis, or other blood clots);
- Narrowing of vessels (such as narrowing of the carotid arteries which increases the risk for stroke);
- Tumors or masses;
- Congenital vascular malformations;
- Reduced or absent blood flow to organs, such as the testes or ovaries (RadiologyInfo.org, 2018b).
There is a wide array of indications for ordering a diagnostic ultrasound. Ultrasound may be used to evaluate for symptoms of pain, swelling, or infection, and can be safely performed on nearly every body system. Below is a list of some of the most common body parts imaged by ultrasound and possible indications for ordering a diagnostic ultrasound, but is not a comprehensive list of indications:
- Gallbladder and bile ducts (gallstones, blockage of bile ducts);
- Heart and blood vessels (patency of blood blow, evaluate for abdominal aortic aneurysm (AAA), carotid arteries for narrowing);
- Liver (cirrhosis, cancer or metastatic tumors, infarction);
- Spleen (splenomegaly);
- Pancreas (pancreatitis, tumor);
- Kidneys, bladder, ureters (masses, cancer, patency, hydronephrosis);
- Uterus (fibroids, fetus in pregnant women);
- Ovaries (cysts, tumors);
- Thyroid and parathyroid glands (masses, enlargement, nodularity);
- Scrotum and testes (testicular torsion, swelling, masses, blockage in blood flow) (RadiologyInfo, 2018b).
In some cases, ultrasound imaging may also use contrast agents for enhancement. Microbubble contrast is useful for the assessment of blood perfusion in organs, thrombosis, abnormalities in the heart, liver or kidney masses, or when evaluating inflammatory activity in inflammatory bowel disease. Most ultrasound imaging requires little to no special preparation before the exam. However, ultrasounds ordered to evaluate the abdominal structures such as the gallbladder generally require patients to fast for four to eight hours before the scan. For ultrasounds ordered to evaluate the bladder, as well as many prenatal ultrasounds, the patient may be asked to drink four to six glasses of water prior to your exam and avoid urinating so that the bladder is full and distended for optimal viewing (NIBIB, 2016).
While ultrasound is considered a very safe and painless medical imaging modality that can be used in patients of all ages, it does have limitations. Air and gas can disrupt or interfere with the ultrasound waves, thereby obscuring images. Ultrasound is not considered a useful option for air-filled organs and structures such as the bowels and lungs. Ultrasound waves are not as effective in obtaining high-quality images in patients who have excess fatty tissue, as the soundwaves weaken as they pass deeper into the body. Further, ultrasound cannot penetrate bone; however, it is useful in identifying infection surrounding the bones (RadiologyInfo.org, 2018b).
Echocardiogram
An echocardiogram is an ultrasound of the heart. It is a commonly used cardiac diagnostic imaging test that does not risk any radiation exposure and is considered safe and effective. Utilizing the same sound wave technology as outlined in the above section, an echocardiogram provides critical information about the heart's functioning and structures, including the valves, chambers, walls, and blood vessels. An echocardiogram may be ordered to further evaluate symptoms of shortness of breath, angina (chest pain), as well as to detect any underlying congenital abnormalities. An echocardiogram can provide information regarding the size, shape, thickness, and movement of the heart, including pericarditis (inflammation of the lining of the heart), stenosis (narrowing of the heart valves) and regurgitation (leaking of blood backward through the heart valves). Similar to a MUGA scan, an echocardiogram also provides information regarding the heart's blood pumping strength, through measurements of the LVEF. As demonstrated in Figure 18, the test is usually performed with the patient lying on their back or their left side. Some patients will also be connected to an EKG to monitor their heartbeat and heart rhythm during the exam. The transducer and gel are applied to the chest and provide real-time images of the heart in motion. There are generally no risks associated with the test, and there are no special preparation instructions (AHA, 2015a).
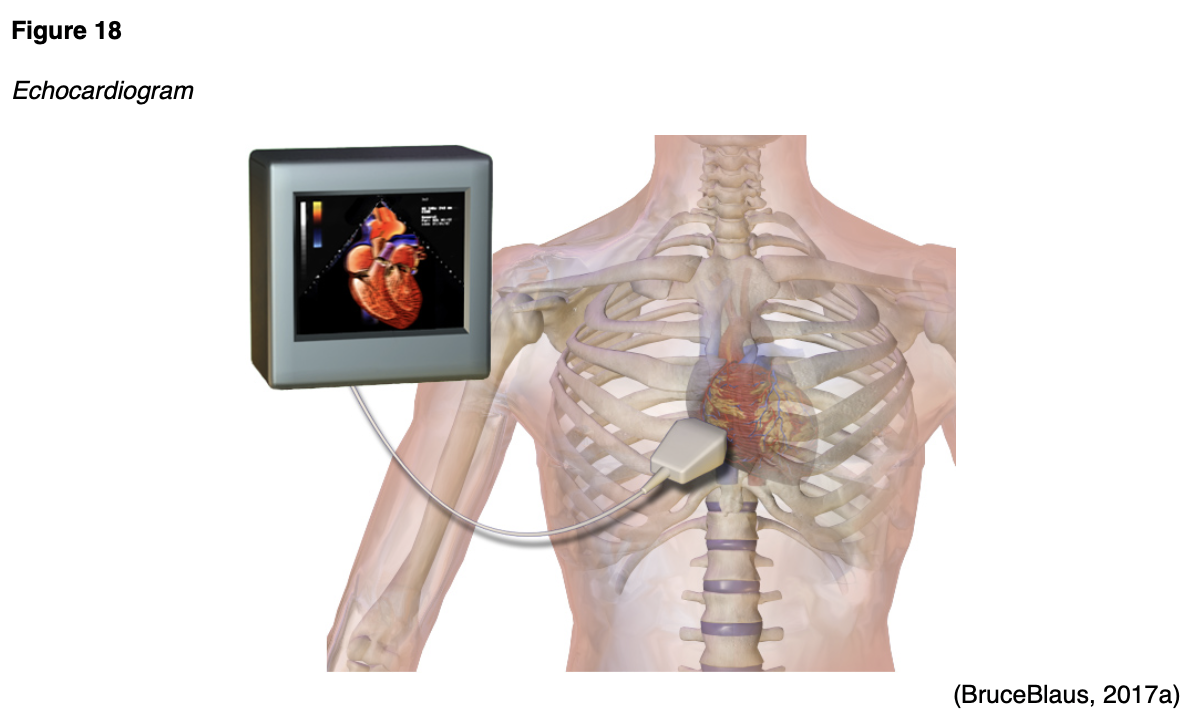
Transesophageal echocardiogram (TEE).
A TEE is a specialized type of echocardiogram that involves the placement of a small, thin tube down into the esophagus as a means of providing a more enhanced evaluation of the heart and its structures than what is provided by a standard (transthoracic) echocardiogram. As highlighted in Figure 19, a tiny transducer is placed at the end of the thin tube, and the soundwaves produce detailed images of the heart, which are translated to a video screen. This is usually performed when additional information is needed following a transthoracic echocardiogram. There are no associated risks of radiation exposure, as ultrasound-based technology is utilized. Patients are usually advised to remain NPO for at least six hours before the scan and are given a sedative immediately before the test to promote relaxation. Some patients report a mild sore throat for one to two days following the test, but generally, there are no reported complications (AHA, 2015d).
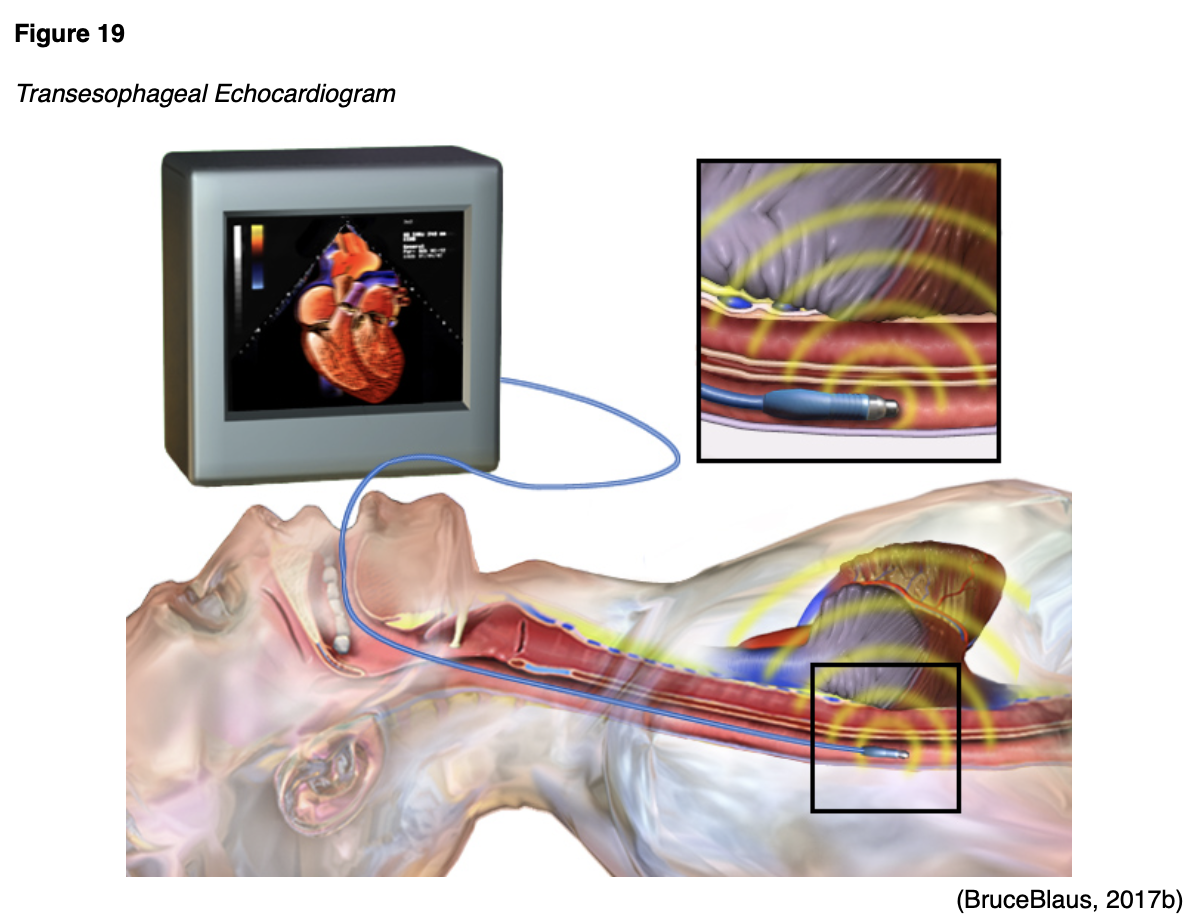
References
American Board of Internal Medicine Foundation. (2020). Choosing wisely: Our mission. https://www.choosingwisely.org/our-mission/
Agency for Healthcare Research and Quality. (2019). Radiation safety. https://psnet.ahrq.gov/primer/radiation-safety#Radiation-Risks-Associated-With-Diagnostic-Imaging
American Association of Physicists in Medicine. (2019). AAPM position statement on the use of patient gonadal and fetal shielding (PP 32-A). https://www.aapm.org/org/policies/details.asp?id=468&type=PP¤t=true
American College of Obstetricians and Gynecologists. (2017). ACOG committee opinion: Guidelines for diagnostic imaging during pregnancy. Obstetrics & Gynecology, 130(4), e210-e216. https://www.acog.org/-/media/project/acog/acogorg/clinical/files/committee-opinion/articles/2017/10/guidelines-for-diagnostic-imaging-during-pregnancy-and-lactation.pdf
American College of Obstetricians and Gynecologists. (2018). Osteoporosis. https://www.acog.org/Patients/FAQs/Osteoporosis?IsMobileSet=false
American College of Radiology. (2017). ACR–SPR practice parameters for the performance of skeletal scintigraphy (bone scan). https://www.acr.org/-/media/ACR/Files/Practice-Parameters/Skeletal-Scint.pdf
American College of Radiology. (2018). ACR-SPR practice parameters for imaging pregnant or potentially pregnant adolescents and women with ionizing radiation. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/Pregnant-Pts.pdf
American College of Radiology. (2019a). ACR endorses AAPM position on patient gonadal and fetal shielding. https://www.acr.org/Advocacy-and-Economics/Advocacy-News/Advocacy-News-Issues/In-the-June-8-2019-Issue/ACR-Endorses-AAPM-Position-on-Patient-Gonadal-and-Fetal-Shielding
American College of Radiology. (2019b). ACR-SNMMI-SPR practice parameter for the performance of scintigraphy and uptake measurements for benign and malignant thyroid disease. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/Thy-Scint.pdf
American Heart Association. (2015a). Echocardiogram (echo). https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/echocardiogram-echo
American Heart Association. (2015b). Radionuclide ventriculography or radionuclide angiography (MUGA scan). https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/radionuclide-ventriculography-or-radionuclide-angiography-muga-scan
American Heart Association. (2015c). Single photon emission computed tomography (SPECT). https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/single-photon-emission-computed-tomography-spect
American Heart Association. (2015d). Transesophageal echocardiography (TEE). https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/transesophageal-echocardiography-tee
American Thyroid Association. (2020). Low iodine diet. https://www.thyroid.org/low-iodine-diet/
Anderson Air Force Base. (2008). Radiation safety practice: X-ray with protective lead apron shielding. [image]. https://www.andersen.af.mil/News/Articles/Article/415997/base-dental-clinic-improves-capabilty-in-areas-of-time-and-efficiency-by-going/
Arleo, E. K., Hendrick, R. E., Helvie, M. A., & Sickles, E. A. (2017). Comparison of recommendations for screening mammography using CISNET models. Cancer, 3673-3680. https://acsjournals.onlinelibrary.wiley.com/doi/epdf/10.1002/cncr.30842
Blausen Medical. (2017). Components of conventional x-ray [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Projectional_radiography_components.jpg
Blausen Medical Communications, Inc. (2013). Bone scan [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Blausen_0098_BoneScan.png
BruceBlaus. (2014). Bone densitometry scan [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Blausen_0095_BoneDensitometryScan.png
BruceBlaus. (2015a). Fetal ultrasound [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Fetal_Ultrasound.png
BruceBlaus. (2015b). Vaginal ultrasound [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Vaginal_Ultrasound.png
BruceBlaus. (2017a). Echocardiogram [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Echocardiogram.png
BruceBlaus. (2017b). Transesophageal echocardiogram [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Transesophageal_Echocardiogram.png
Brudersohn. (2012). PET/CT scan [image]. Wikimedia. https://en.m.wikipedia.org/wiki/File:PET-CT_Siemens_Biograph01.jpg
Cancer.net. (2018). Bone scan. https://www.cancer.net/navigating-cancer-care/diagnosing-cancer/tests-and-procedures/bone-scan
The Centers for Disease Control and Prevention. (2015a). Electromagnetic spectrum: Ionizing radiation. https://www.cdc.gov/nceh/radiation/ionizing_radiation.html
The Centers for Disease Control and Prevention. (2015b). Health effects of radiation: Health effects depend on the dose. https://www.cdc.gov/nceh/radiation/dose.html
The Centers for Disease Control and Prevention. (2015c). Radiation safety. https://www.cdc.gov/nceh/radiation/safety.html
The Centers for Disease Control and Prevention. (2015d). What is radiation? The electromagnetic spectrum. https://www.cdc.gov/nceh/radiation/spectrum.html
The Centers for Disease Control and Prevention. (2016). Radiation in medicine: Fluoroscopy. https://www.cdc.gov/nceh/radiation/fluoroscopy.html
The Centers for Disease Control and Prevention. (2019). Radiation in medicine: Medical imaging procedures. https://www.cdc.gov/nceh/features/medical-imaging-procedures/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Ffeatures%2Fmedical-imaging-procedures%2Findex.html
The Centers for Medicare & Medicaid Services. (2018). Appropriate use criteria for advanced diagnostic imaging. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/AUCDiagnosticImaging-909377.pdf
The Centers for Medicare & Medicaid Services. (2020). Appropriate use criteria program. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Appropriate-Use-Criteria-Program
Chen, C., Hsueh, Y., Lan, T., Lin, W., Wu, K, & Yang, R. (2010). Skeletal scintigraphy of the pelvis with bone metastasis [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Scintigraphy_pelvis_with_bone_metastasis_01.jpg
Elsayes, K. M., & Oldham, S. A. A. (2014). Introduction to diagnostic radiology. McGraw-Hill Education.
Frantzen, M. J., Robben, S., Postma, A. A., Zoetelief, J., Wildberger, J. E., & Kemerink, G. J. (2012). Gonad shielding in paediatric pelvic radiography: Disadvantages prevail over benefit. Insights Imaging, 3(1), 23-32. https://doi.org/10.1007/s13244-011-0130-3
Gathany, J. (2012). Conventional sonogram (left) compared to 3-D sonogram of fetus (right) [image]. http://www.publicdomainfiles.com/show_file.php?id=13526946615346
Ghadimi, M., & Sapra, A. (2019). Magnetic resonance imaging (MRI): Contraindications. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK551669/
Ibrahim, M. A., Hazhirkarzar, B., & Dublin, A. B. (2020). Magnetic resonance imaging (MRI): Gadolinium. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK482487/
International Atomic Energy Agency. (n.d.a.). Computed tomography: What patients need to know. Retrieved April 17, 2020 from https://www.iaea.org/resources/rpop/patients-and-public/computed-tomography
International Atomic Energy Agency. (n.d.b). X-rays: What patients need to know. Retrieved April 18, 2020 from https://www.iaea.org/resources/rpop/patients-and-public/x-rays#1
Jarmoluk. (2019). MRI scan [image]. https://www.needpix.com/photo/1153705/mri-magnetic-resonance-imaging-diagnostics-hospital-the-test-research-medical-health-the-disease
Jmarchn. (2015). DXA scan results: Osteopenia of the lumbar spine [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:DXA_Lumbar_vertebral_column_Osteopenia_es.png
Johns Hopkins Medicine. (n.d.a). Barium x-rays (upper and lower GI). Retrieved April 16, 2020 from https://www.hopkinsmedicine.org/health/conditions-and-diseases/barium-xrays-upper-and-lower-gi
Johns Hopkins Medicine. (n.d.b). Fluoroscopy procedure. Retrieved April 16, 2020 from https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/fluoroscopy-procedure
Katzen, J., & Dodelzon, K. (2018). A review of computer aided detection in mammography. Clinical Imaging, 52, 305-309. https://doi.org/10.1016/j.clinimag.2018.08.014
Kim, L. H., Vail, D., Azad, T. J., Bentley, J. P., Zhang, Y., Ho, A. L., Fatemi, P., Feng, A., Barshneya, K., Desai, M., Veeravagu, A., & Ratliff, J. K. (2019). Expenditures and health care utilization among adults with newly diagnosed low back and lower extremity pain. JAMA Network Open, 2(5), 3193676. https://doi.org/10.1001/jamanetworkopen.2019.3676
Kolla, B. C., Roy, S. S., Duval, S., Weisdorf, D., Valeti, U., & Blaes, A. (2017). Cardiac imaging methods for chemotherapy-related cardiotoxicity screening and related radiation exposure: Current practice and trends. Anticancer Research, 37(5), 2445-2449. https://doi.org/10.21873/anticanres.11584
Litowski, P. E., Smetana, G. W., Zeidel, M. L., & Blanchard, M. S. (2016). Curbing the urge to image. AAIM Perspectives, 129(10), 1131-1135. https://doi.org/10.1016/j.amjmed.2016.06.020
Madcapslaugh. (2008). Conventional sonogram (left) compared to 3-D sonogram of fetus (right) [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:4dsonogram.jpg
Marsh, R. M., & Silosky, M. (2019). Patient shielding in diagnostic imaging: Discontinuing a legacy practice. AJR, 212(4), 755-757. https://doi.org/10.2214/AJR.18.20508
Mayo Clinic. (2019a). Mammogram. https://www.mayoclinic.org/tests-procedures/mammogram/about/pac-20384806
Mayo Clinic. (2019b) MRI. https://www.mayoclinic.org/tests-procedures/mri/about/pac-20384768
Mayo Clinic. (2019c). SPECT scan. https://www.mayoclinic.org/tests-procedures/spect-scan/about/pac-20384925
McCance, K. L., & Heuther, S. E. (2019). Pathophysiology: The biologic basis for disease in adults and children (8th ed.). Elsevier.
Memorial Sloan Kettering Cancer Center. (2019). About your PET-CT with FDG tracer. https://www.mskcc.org/cancer-care/patient-education/pet-ct#section-5
Myohan. (2009). Normal PET/CT scan images [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Nl_petct.jpg
National Cancer Institute. (2007). Mammography [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:MammographyinprocessGraphic.jpg
National Cancer Institute. (2016). Mammograms. https://www.cancer.gov/types/breast/mammograms-fact-sheet#what-are-the-benefits-and-potential-harms-of-screening-mammograms
National Cancer Institute. (2019). Breast cancer risk in American women. https://www.cancer.gov/types/breast/risk-fact-sheet#r1
National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2018). Bone mass measurement: What the numbers means. https://www.bones.nih.gov/health-info/bone/bone-health/bone-mass-measure#c
National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2019). Osteoporosis. https://www.niams.nih.gov/health-topics/osteoporosis#tab-overview
National Institute of Biomedical Imaging and Bioengineering. (2016). Ultrasound. https://www.nibib.nih.gov/science-education/science-topics/ultrasound
National Institute of Biomedical Imaging and Bioengineering. (2019). What is nuclear medicine? https://www.nibib.nih.gov/sites/default/files/Nuclear%20Medicine.pdf
NithinRao. (2009). CT scan [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Ct-scan.jpg
Papanicolas, I., Woskie, L. R., & Jha, A. K. (2018). Healthcare spending in the United States and other high-income countries. JAMA, 319(10), 1024-1039. https://doi.org/10.1001/jama.2018.1150
Porter, J. L., & Varacallo, M. (2019). Osteoporosis. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK441901/
PxHere. (n.d.). Caution x-ray equipment [image]. Retrieved May 5, 2020 from https://pxhere.com/en/photo/1054776
RadiologyInfo.org, Radiological Society of North America, & American College of Radiology. (2015). Radiation dose to patients from common imaging examinations. https://radltd.com/files/Dose-Reference-Card_web_62215.pdf
RadiologyInfo.org. (2018a). Contrast materials. https://www.radiologyinfo.org/en/pdf/safety-contrast.pdf
RadiologyInfo.org. (2018b). General ultrasound. https://www.radiologyinfo.org/en/info.cfm?pg=genus
RadiologyInfo.org (2018c). What is radiation dose? https://www.radiologyinfo.org/en/info.cfm?pg=safety-hiw_09
RadiologyInfo.org. (2019a). Intravenous pyelogram (IVP). https://www.radiologyinfo.org/en/info.cfm?pg=ivp
RadiologyInfo.org. (2019b). Mammography. https://www.radiologyinfo.org/en/info.cfm?pg=mammo
RadiologyInfo.org. (2019c). Thyroid scan and uptake. https://www.radiologyinfo.org/en/info.cfm?pg=thyroiduptake
RadiologyInfo.org. (2020a). Bone densitometry (DEXA, DXA). https://www.radiologyinfo.org/en/info.cfm?pg=dexa
RadiologyInfo.org. (2020b). Skeletal scintigraphy (bone scan). https://www.radiologyinfo.org/en/info.cfm?pg=bone-scan
Smith-Bindman, R., Miglioretti, D. L., Johnson, E., Lee, C., Feigelson, H. S., Flynn, M., Greelee, R. T., Kruger, R. L., Horbrook, M. C., Roblin, D., Solberg, L., Vanneman, N.., Weinmann, S., & Williams, A. E. (2012). Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA, 307(22), 2400-2409. https://doi.org/10.1001/jama.2012.5960
Society of Nuclear Medicine & Molecular Imaging. (n.d.). Fact sheet: What is nuclear medicine and molecular imaging? Retrieved on April 17, 2020 from https://www.snmmi.org/AboutSNMMI/Content.aspx?ItemNumber=5648
Thayalan, K. (2014). The physics of radiology and imaging. Jaypee Brothers Medical Publishers (P) Ltd
US Department of Labor Occupational Safety and Health Administration. (n.d.). Ionizing radiation control & prevention. https://www.osha.gov/SLTC/radiationionizing/prevention.html#PPE
US Food & Drug Administration. (2017). Safety concerns with implantable infusion pumps in the magnetic resonance (MR) environment: FDA safety communication. https://www.fda.gov/medical-devices/safety-communications/safety-concerns-implantable-infusion-pumps-magnetic-resonance-mr-environment-fda-safety
US Food & Drug Administration. (2018). MRI (magnetic resonance imaging). https://www.fda.gov/radiation-emitting-products/medical-imaging/mri-magnetic-resonance-imaging
Ytrottier. (2012). SPECT scan [image]. Wikimedia. https://commons.wikimedia.org/wiki/File:SPECT_CT.JPG