The purpose of this activity is to enable the learner to recognize the steps of the primary survey for trauma patients and recognize current evidence-based practice as it relates to the management of trauma patients when their airway and breathing is compromised, when they experience life-threatening bleeding and shock, and when they experience musculoskeletal trauma.
...purchase below to continue the course
lumen esophageal tube has two ports, one in the esophagus and one in the airway. The tube is inserted and the port that is in the airway is identified. The esophageal port is then occluded, and ventilation provided through the bronchial port. End-tidal CO
2 (ETCO
2) can be used to confirm placement. Either of these devices should be replaced by a definitive airway as soon as clinically possible (ACOS, 2018).
Endotracheal tubes are definitive airways, defined as a tube that is placed in the trachea with a cuff below the vocal cords that is inflated to prevent aspiration. A surgical airway (cricothyroidotomy or a tracheostomy) is also a definitive airway. Criteria for the placement of a definitive airway includes:
- inability to maintain airway or breathing,
- GCS less than eight, or
- sustained seizure activity (ACOS, 2018).
Drug-assisted intubation is an updated term to describe rapid sequence intubation (RSI) with pharmacologic intervention (Henry, 2018). RSI has historically been defined as the administration of a sedative and a neuromuscular blocking agent to induce unconsciousness and paralysis to facilitate intubation (Chapleau, 2009). Etomidate (Amidate)(.3 mg/kg) and ketamine (Ketalar)(1.5 mg/kg) are commonly used induction agents. Both medications in the absence of acute shock have cardiovascular stability. Succinylcholine (Anectine)(1-2 mg/kg) is the paralytic of choice. Hospital protocols for drug-assisted intubation should be followed (Chapleau, 2009; Crewdson & Lockey, 2016; Horton et al., 2014)
Clinical assessment to validate the proper placement of an ETT includes:
- visual observation of rise and fall of the chest,
- auscultation of the lungs,
- chest x-ray,
- pulse oximetry, and
- ETCO2 (ACOS, 2018; Craig-Brangan & Day, 2016).
ETCO2 through capnography is the most reliable assessment parameter to validate that the ETT is in the trachea and is the standard of care for patients who have been intubated (Craig-Brangan & Day, 2016; Crewdson & Lackey, 2016). A chest x-ray is often performed to validate proper positioning of the tube in the trachea (ACOS, 2018).
Breathing
Regardless of whether an airway is required, providing adequate ventilation is critical. The American Heart Association (AHA) guidelines state that once an advanced airway is placed, the patient should be ventilated at a rate of one breath every six seconds or ten breaths per minute (Craig-Brangan & Day, 2016). Most trauma patients require supplemental oxygen. Breathing and ventilation changes can occur quickly. Continuous pulse oximetry is recommended for all trauma patients to provide rapid assessment of any oxygen changes. If a patient requires ventilation but does not have a definitive airway, the use of a bag-mask is standard of care. If possible, it is recommended that two people assist with the bag-mask ventilation to ensure an adequate seal (ACOS, 2018). The MOANS mnemonic helps the nurse to identify patients who may be difficult to ventilate:
- Mask seal
- Obesity/obstruction
- Aged (over the age of 55)
- No teeth
- Stiff lungs (Horton et al., 2014)
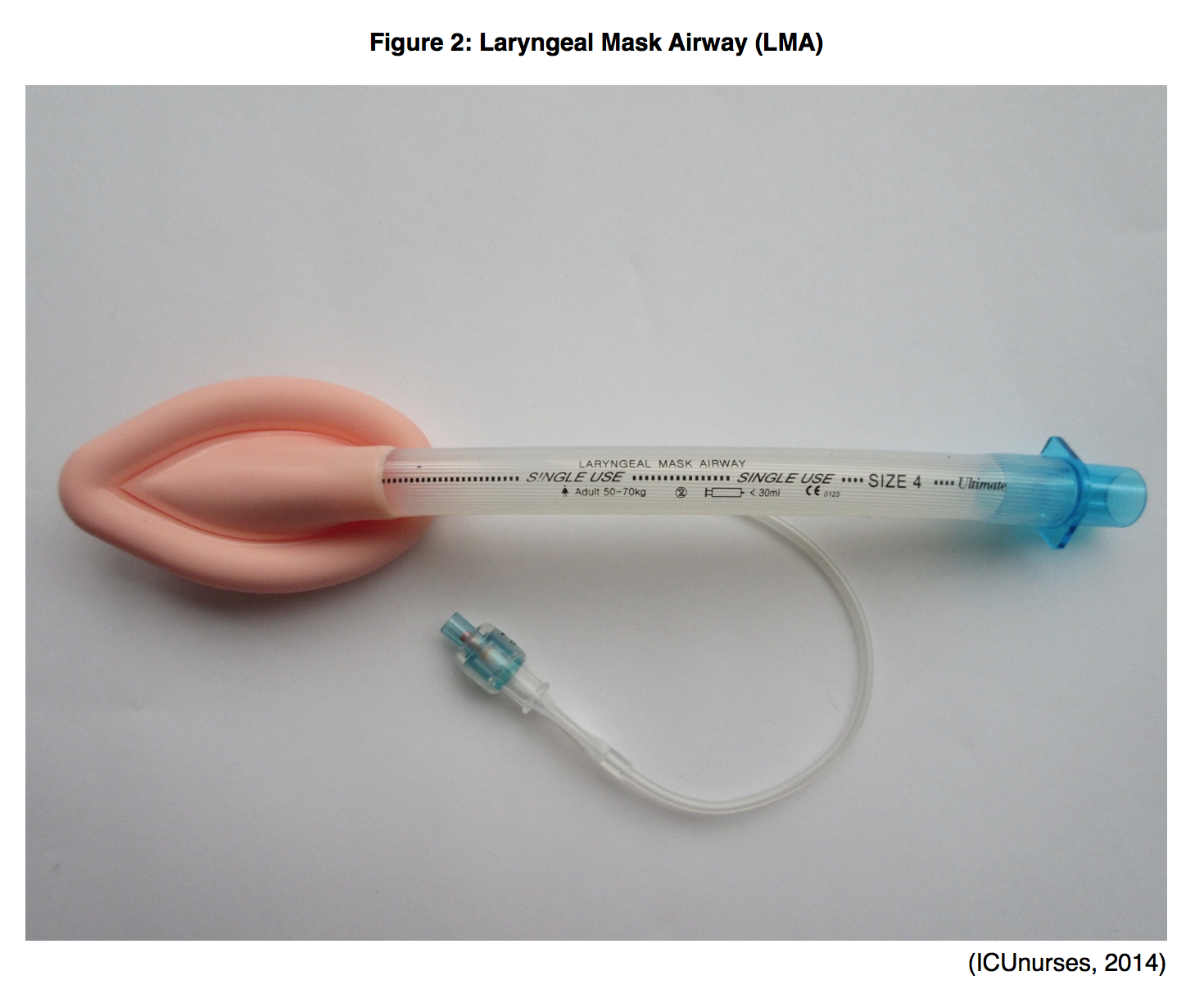
Patients that are difficult to ventilate with a bag-mask may require an airway that enables the use of a bag-valve (LMA or a multi-lumen esophageal airway) until a definitive airway can be placed (ACOS, 2018).
Circulation and Hemorrhage Control
Circulation with hemorrhage control is the third step in the primary survey. In a mass casualty/combat scenario, life-threatening hemorrhage takes priority to airway and breathing in the primary survey (ACOS, 2018). 30-40% of preventable trauma deaths are due to uncontrolled bleeding (Uhlenbrock, 2015). This statistic increases to 90% within combat settings (ACOS, 2018). It is critical to control hemorrhaging in the immediate aftermath of trauma. A major arterial bleed can cause death in less than five minutes (Quail, 2017). Standard of care dictates direct manual pressure to the site, but when this does not control the bleeding, the use of a tourniquet should be considered (Henry, 2018; Scerbo et al., 2017).
The United States military has a long history of using tourniquets as a first-line intervention for extremity hemorrhage control. By contrast, data relating to tourniquet use in civilians is lacking (Day, 2016; Kauvar, Dubick, Walters, & Kragh, 2017). While prolonged use of a tourniquet can lead to permanent neurovascular damage that can lead to amputation, recent retrospective studies that compared outcomes from using tourniquets in the prehospital setting versus no tourniquet in cases of uncontrolled bleeding demonstrated better overall outcomes for those trauma patients who received a tourniquet prehospital. Results included increased systolic blood pressure upon arrival to the trauma center, decreased need for blood products, decreased limb complications, and decrease in mortality related to hemorrhagic shock (Scerbo et al., 2017; Schroll et al., 2015; Smith et al., 2019).
After the Sandy Hook mass shooting in 2012, the Hartford Consensus Group came out with recommendations for the management of injuries in a mass casualty setting. They identified that after suppressing an actual threat, the priority is to stop the bleeding. This led to an initiative signed by President Obama in 2015 called the Stop the Bleed campaign. The motto of this campaign is if you see something, do something (Quail, 2017). The goal of the campaign is to teach bystanders how to stop bleeding by providing free education and advocating for bleeding control kits to be available in public places wherever defibrillators are available (Uhlenbrock, 2015). Tourniquets are an essential tool to stop severe bleeding if applying direct pressure does not work. In addition, the AHA updated their First Aid Guidelines to include consideration of a tourniquet when direct pressure does not control the bleeding. The guidelines also state that a tourniquet can be considered as a first-line intervention when an individual is unable to provide standard bleeding control. Situations where standard bleeding interventions may be inadequate include mass casualties, multisystem traumas, or an inaccessible wound (American Heart Association, 2015).
The goal of using a tourniquet is to stop the arterial bleeding. Commercial tourniquets should be used when available. One option is the windlass device which is a manual tourniquet. Once applied, the windlass is tightened until the arterial blood flow stops and pulses distal to the injury disappear. Another option is the pneumatic tourniquet which is inflated with air to a pressure that stops the bleeding and distal pulses disappear (ACOS, 2018). In a situation where a commercial tourniquet is not available, belts, clothing, or cables could be used (ACOS, 2018). The ideal tourniquet should be at least two inches wide. A wider tourniquet requires less pressure to stop the blood flow. Also, it should be made of inelastic material to avoid the tourniquet slipping (Day, 2016). Tourniquets should never be applied over a joint, and once a tourniquet has been applied, it should not be removed until the patient has access to definitive care (Bulgar et al., 2014). Improper application of a tourniquet can lead to compartment syndrome (ACOS, 2018; Day, 2016). Because the risk of long-term complications from a tourniquet are rare, the decision to save a life over a limb has to be made when intervening with a tourniquet (ACOS, 2018).
Steps for controlling external hemorrhage:
- Apply direct pressure to the site with clothing or a clean towel.
- If the wound is large, pack clothing or towel into the wound and then apply pressure.
- Pressure should be applied with two hands and not released until definitive care is available.
- If the hemorrhage is uncontrolled, a tourniquet should be considered.
- Place the tourniquet above the injury site.
- Apply the tourniquet by tightening until the bleeding stops and distal pulses are no longer palpable.
- If the bleeding does not stop, consider applying a second tourniquet.
- Mark the patient’s forehead with a T and the time that the tourniquet was placed.
- Do not cover the tourniquet with clothing or blankets.
- Frequently assess the site.
- Do not release the tourniquet until definitive care is available.
- If it is a joint injury with uncontrolled bleeding, consider a topical hemostatic agent with direct pressure (ACOS, 2018; Bulgar et al., 2014; Day, 2016).
Because massive blood loss can lead to shock, obtaining vascular access in trauma patients is critical. The recommended access is an 18 gauge or larger peripheral intravenous (IV) catheter. When adequate peripheral access cannot be obtained quickly, intraosseous (IO) access should be considered for all age groups (ACOS, 2018). If emergency medications are required, IV/IO access provide better absorption of medications than the ETT route, and IO medications are absorbed more rapidly into central circulation than a peripheral IV (Faminu, 2014).
The IO provides access to the medullary space of the long bones. This space in noncollapsible and highly vascular. The proximal humerus and proximal tibia are the most common sites. Fluids, blood products, medications, and contrast media can all be infused through an IO access. The IO access can be established in as little as 10 seconds, allowing fluid resuscitation to begin immediately. Fluids administered through an IO reach the central circulation at the same rate as fluids infused through a central line. The use of an IO reduces the risk of infection when compared to peripheral and central access, most likely due to the short dwell time (less than 24 hours) (Faminu, 2014).
IO devices should only be placed by specially trained providers. Nurses may place IO devices if allowed by their institution and the board of nursing for their particular state. Contraindications to using an IO are a bone fracture and previous insertion in the same site within the last 24 hours. Also, an MRI cannot be performed in a patient with an IO (Faminu, 2014).
The nurse should appropriately verify placement of an IO by:
- A loss of resistance once the needle passes through the bone;
- the absence of signs of infiltration;
- the needle remains in position when flushed; and
- successful aspiration of bone marrow or blood (but the absence of either of these does not necessarily indicate incorrect placement) (ACOS, 2018; Faminu, 2014).
Nursing implications after insertion of IO access include:
- Stabilize the device per facility protocol.
- Immobilize the involved extremity to protect from accidental dislodgement.
- Maintain device patency with a continuous infusion of 0.9% normal saline.
- Manage infusion pain from pressure receptors in the bone (infusion pain is more intense than insertion pain) (ACOS, 2018; Faminu, 2014).
Complications from the use of an IO may include:
- osteomyelitis (dwell time should be limited to 24 hours,
- infiltration (same manifestations as a peripheral IV),
- compartment syndrome (rare),or
- occlusion of the needle with fibrin mesh or bone marrow (minimized by using stylet during insertion of the IO) (ACOS, 2018; Faminu, 2014).
Removal of an IO can only be performed by a qualified provider. As with any IV removal, inspect the device to make sure it is still intact. If the needle detaches from the hub, use needle forceps to withdraw the needle. The nurse should also document the time of removal. The same site cannot be accessed for the next 24 hours (Faminu, 2014). The use of an IO should be reserved for emergency resuscitation situations. Once adequate venous access is obtained, the IO should be discontinued (ACOS, 2018).
Disability
The disability step of the primary survey includes a brief neurologic examination to assess level of consciousness and measures to prevent long-term neurological damage. The GCS is an easy, objective assessment of this (refer to GCS in airway section). The 10th edition of ATLS introduced a new GCS that adds a nontestable for each of the components of the scale. A decrease in GCS may indicate a perfusion problem or a decrease in oxygen to the brain, and the provider should immediately reassess airway, breathing, and circulation. Raising the head of the bed slightly and mild hyperventilation may help maintain/reduce the intracranial pressure. It is important to avoid moderate to severe hyperventilation, aiming for a PCO2 above 25 (ideal is 35). Pupils should also be assessed for size, shape and reactivity. Systolic blood pressure should be greater than 100 mg Hg for individuals between the ages of 50 and 69 and greater than 110 mg Hg for individuals between the ages of 15 and 49 and those older than 70. The nurse should advocate for a neurosurgical consult if the disability step indicates worsening neurological function (ACOS, 2018; Henry, 2018).
Exposure and Environmental Control
Removing all clothing from a trauma patient allows for visualization of the entire body. Identifying musculoskeletal trauma is critical to preserving circulation and maintaining neurovascular function (Chapleau, 2009). Following the assessment, hypothermia is prevented by applying warm blankets, an external warming device, or infusing warmed IV fluids. A high-flow fluid warmer is recommended to heat crystalloids; if not available, a microwave can be used. Blood products should never be heated in the microwave (ACOS, 2018).
Stabilization of Musculoskeletal Injuries
When musculoskeletal trauma is identified, the goal of trauma care is to immobilize the injured extremity to manage pain, decrease swelling, and prevent further neurovascular damage (Do, 2017). Also, splinting may help to control bleeding (McKelvin, 2018). While there are no absolute contraindications to the use of a splint in trauma, caution should be exercised in the presence of open fractures, evidence of compartment syndrome, and neurovascular compromise. The goal of splinting is temporary immobilization until definitive treatment is available (Do, 2017).
When considering how to splint a fracture, the nurse should consider how the fracture presents. For simple fractures, the patient should have a distal pulse. In this case, the splint should be applied to maintain the current position of the extremity. If the extremity is in an abnormal position and no distal pulse is assessed, the limb may require manipulation before the splint can be applied. The research is lacking on whether or not an angulated bone should be straightened before splinting American Heart Association, 2015). This procedure can be painful, so sedation and analgesia are recommended if available. If an open fracture is present, realignment should not be attempted. If a splint is applied, it should be applied to maintain the current position of the extremity (ACOS, 2018).
Splints should not take priority over resuscitation, but they can control bleeding and should be considered essential treatment to prevent circulatory collapse if internal bleeding is suspected. It is critical that splinting be done before transport of the patient (ACOS, 2018). Any of the following injuries should be considered for splinting:
- fractures,
- dislocations,
- severe strains and sprains, or
- torn tendons or ligaments (McKelvin, 2018).
There are multiple types of splints to immobilize injuries. These can be cardboard, metal, pneumatic, or plastic (Chapleau, 2009). A spine board provides splinting for the entire body but padding should be added to protect pressure points. Long-leg splints are used for tibia fractures. These may be metal or cardboard and should also be padded. Pillow splints or padded cardboard splints are good for ankle fractures. Injuries to the upper extremities and hands should be splinted in normal anatomic position using a flat splint or pillow splint. When splinting a knee injury, it is critical to flex the knee 10° to relieve pressure (ACOS, 2018).
Traction splints are used to realign a femoral fracture and promote adequate blood flow (ACOS, 2018). Types of traction splints include the Hare and Sager splints (Chapleau, 2009). General considerations for the application of a traction splint include:
- Two personnel are required.
- Evaluate distal pulses before splint placement.
- The upper splint should be placed at the crease of the buttock.
- The distal end of the splint should be six inches past the ankle.
- Straps should be placed above and below the knee.
- Align the femur by manual traction at the ankle and maintain traction while the splint is applied.
- Once the splint is in place, apply traction in increments until the extremity is stabilized.
- Evaluate distal pulses again after splint placement (ACOS, 2018).
Pneumatic trousers are used for pelvic fractures. Caution should be exercised when removing this splint device, as hypotension may occur with rapid removal (Chapleau, 2009).
Nursing Implications
Nurses may encounter trauma patients in the pre-hospital setting as a first responder or in the emergency department. In addition, nurses as educators can provide teaching to lay persons who may be the first on the scene of a trauma incident. The primary survey provides a rapid assessment of the immediate needs of the patient so the appropriate interventions can be utilized to manage the airway, ventilate, control hemorrhaging, stabilize musculoskeletal trauma, and prevent hypothermia. Knowing how to maintain an airway, provide ventilation, apply a tourniquet, and splint an extremity may make the difference between life and death for a trauma patient.
References
ACLS Certification Institute (n.d.) Laryngeal Mask Airways (LMA). Retrieved August 2019 from https://acls.com/free-resources/knowledge-base/respiratory-arrest-airway-management/laryngeal-mask-airways-lma
American College of Surgeons. (2018). Advanced trauma life support (ATLS) student course manual. Chicago, IL: American College of Surgeons.
American Heart Association. (2015). ECC Guidelines : Part 15: First Aid. Retrieved from https://eccguidelines.heart.org/circulation/aha-red-cross-first-aid-guidelines/part-15-first-aid/
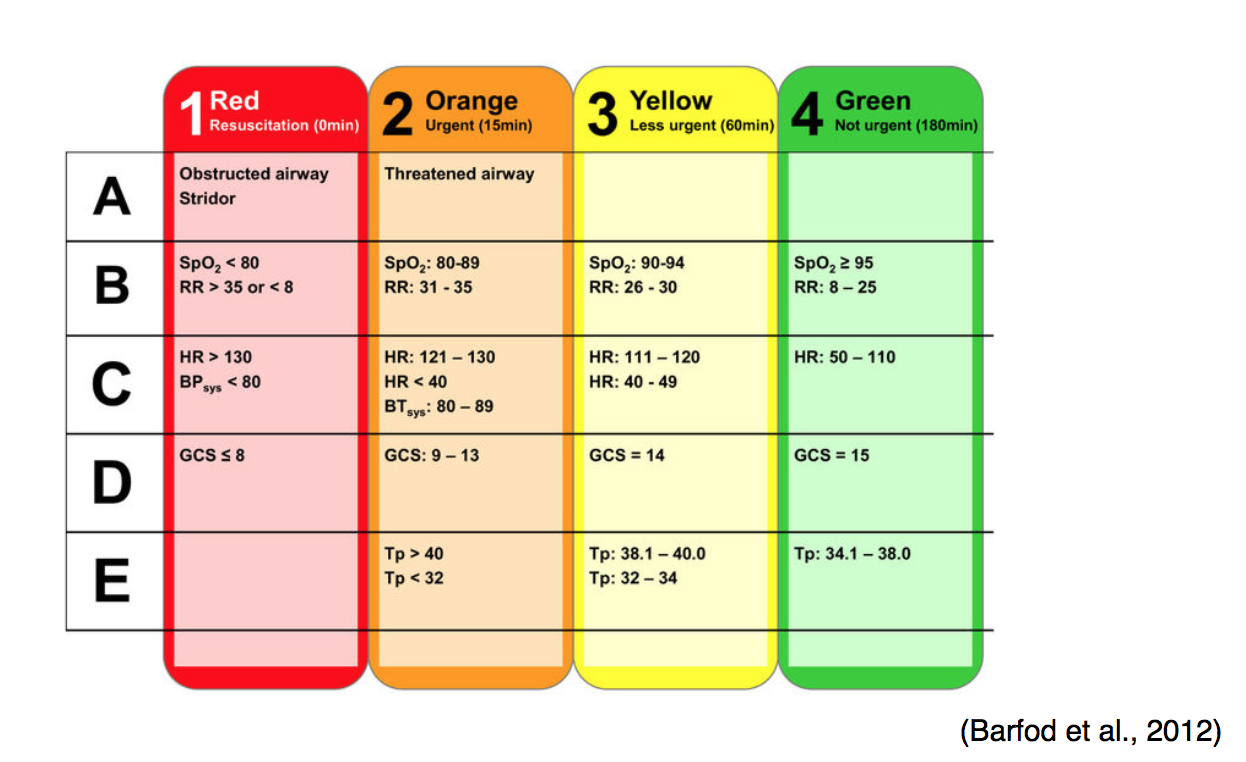
Barfod, C., Lauritzen, M. M. P., Danker, J. K., Sölétormos, G., Forberg, J. L., Berlac, P. A., … Lange, K. H. W. (2012). Abnormal vital signs are strong predictors for intensive care unit admission and in-hospital mortality in adults triaged in the emergency department—A prospective cohort study. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 20(1), 28. doi: 10.1186/1757-7241-20-28
Bulgur, E.M., Snyder, D., Schoelles, K., Gotschall, C., Dawson, D., Lang, E., … McSwaing, N. (2014). An evidence-based prehospital guideline for external hemorrhage control: American College of Surgeons committee on trauma. Prehospital Emergency Care, 18 (2), 163-173. doi: 10.3109/10903127.2014.896962
The Centers for Disease Control and Prevention (n.d.) Glasgow Coma Scale. Retrieved November 1, 2019 from https://www.cdc.gov/masstrauma/resources/gcs.pdf
Chapleau, W. (2009). Prehospital care of the trauma patient. In K.A. McQuillan, M.B. Flynn, and E. Whalen (Ed.), Trauma nursing from resuscitation through rehabilitation. (4th ed, pp. 99-107). St. Louis, MO: Saunders Elsevier.
Craig-Brangan, K.J. and Day, M.P. (2016). 2015 AHA BLS and ACLS guidelines. Nursing, 46(2), 40-45. doi: 10.1097/01.NURSE.0000476229.95631.bf
Crewdson, K., & Lockey, D. (2016). Advanced airway management for pre-hospital trauma patients. Trauma, 18(2), 111-118. doi: 10.1177/1460408615617788
Day, M. (2016). Control of traumatic extremity hemorrhage. Critical Care Nurse, 36(1), 40-51. doi: 10.4037/ccn2016871
Do, T.T. (2017). Splinting. Retrieved from https://emedicine.medscape.com/article/1997864
Faminu, F. (2014). Intraosseous vascular access: Boning up on the basics. Nursing, 44(8), 60-64. doi: 10.1097/01.NURSE.0000451529.25903.4b
Kauvar, D.S., Dubick, M.A., Walters, T.J., & Kragh, J.F. (2017). Systematic review of prehospital tourniquet use in civilian limb trauma. J Trauma Acute Care Surg, 84(5), 819-825. doi: 10.1097/TA.0000000000001826
Henry, S. (2018). ATLS 10th edition offers new insights into managing trauma patients. Retrieved from bulletin.facs.org/2018/06/atls-edition-offers-new-insights-into-managing-trauma-patients/#printpreview.
Horton, C.L., Brown, C.A., Raja, A.S. (2014). Trauma airway management. The Journal of Emergency Medicine, 46(6), 814-820. doi: 10.1016/j.jemermed.2013.11.085
ICUnurses (2014). Laryngeal Mask Airway [Image]. Retrieved from https://upload.wikimedia.org/wikipedia/commons/7/79/LMA_Adult_size_4.JPG
McKelvin, R. (2018). Splinting of injuries: best practice guidance. Journal of Paramedic Medicine, 10(12), 534-536. doi:10.12968/jpar.248.10.12.534
Quail, M. (2017). What’s the Stop the Bleed Campaign? Nursing, 47(12), 15-16. doi:10.1097/01.NURSE.0000526884. 10306. 68
Scerbo, M.H., Holcomb, J.B., Taub, E., Gates, K., Love, J.D., Wade, C.E., Cotton, B. A. (2017). The trauma is too late: Major limb trauma without a pre-hospital tourniquet has increased death from hemorrhagic shock. J Trauma Acute Care Surg, 83(6), 1165-1172. doi: 10.1097/TA.0000000000001666
Schroll, R., Smith, A., McSwain, N.E., Myers, J., Rocchi, K., Inaba, K., … Meade, P. (2015). A multi-institutional analysis of prehospital tourniquet use. J Trauma Acute Care Surg, 78(1), 10-14. doi: 10.1097/TA.000000000000689
Smith, A.A., Ochoa, J.E., Wong, S., Beatty, S., Elder, J., Guidry, C., … Schroll, R. (2019). Prehospital tourniquet use in penetrating extremity trauma: decreased blood transfusions and limb complications. J Trauma Acute Care Surg, 86(1), 43-51. doi: 10.1097/TA.0000000000002095
Uhlenbrock, J.S. (2019). Emergency Nurses Association position statement: Trauma nursing education. Retrieved from https://www.ena.org/practice-resources/resource-library/position-statements